
Blood clots, also called thrombi, are gel-like masses made up of platelets and fibrin. These components work together to stop bleeding after an injury by forming a clot. The clot’s texture can vary from soft to hard, influenced by its age and composition. Knowing the different kinds of blood clots and their makeup is crucial for recognizing potential health risks and understanding how clots affect blood flow and healing.
At Liv Hospital, we know how important it is to find and treat blood clots right. Blood clots are good at first, but where and when they form matters. If they form when they shouldn’t, they can cause big health problems.
Key Takeaways
- Blood clots are formed by platelets and fibrin to prevent bleeding.
- There are various types of blood clots, each with distinct characteristics.
- Understanding the different types is key to spotting health risks.
- Liv Hospital offers expert diagnosis and treatment for blood clots.
- Prompt medical attention is necessary for potentially life-threatening conditions.
What Are Blood Clots and Why Do They Form?

Blood clots are a natural response to injury. They are part of our body’s healing process. Knowing about them is key to understanding health and disease.
A blood clot is a mass of blood that turns from liquid to solid. This stops bleeding when we’re hurt. A thrombus is a clot that stays in one place. An embolus is one that moves.
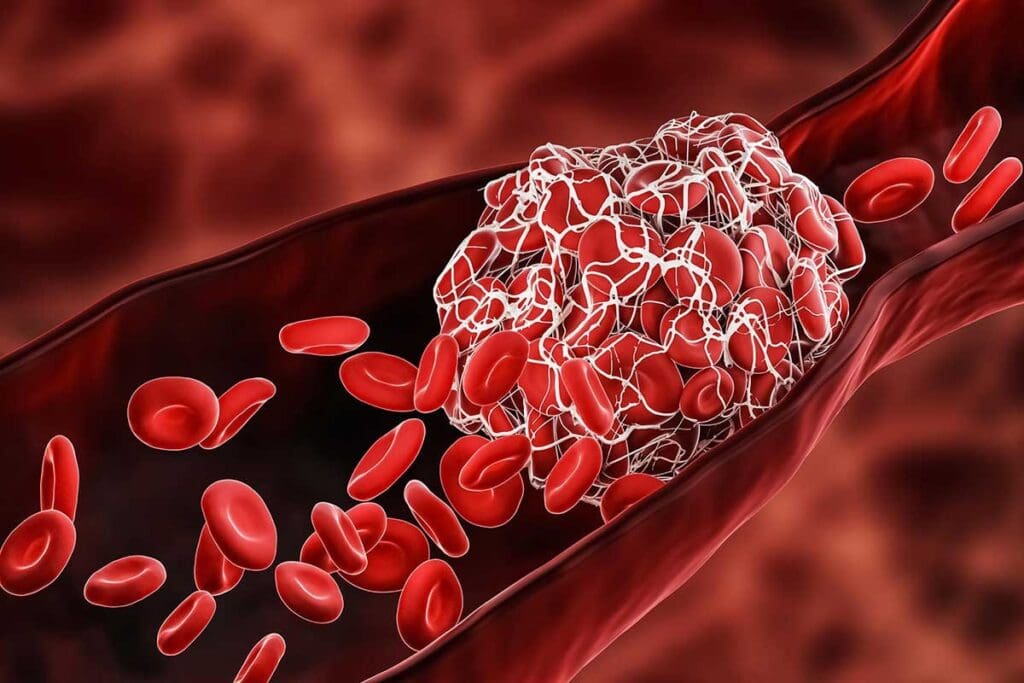
The Composition of Blood Clots
Blood clots are made of platelets and fibrin. When we get a cut, platelets form a plug. Proteins in our blood plasma then make a mesh of fibrin strands to strengthen the plug.
The clot has red blood cells, white blood cells, and platelets in a fibrin mesh. Knowing what a blood clot is and what it’s made of helps us understand its role.
| Component | Description | Role in Clot Formation |
| Platelets | Small, colorless cell fragments | Stick together to form the initial plug |
| Fibrin | Protein strands | Creates a mesh that strengthens the clot |
| Red Blood Cells | Cells that carry oxygen | Trapped within the fibrin mesh |
| White Blood Cells | Cells that fight infection | Also trapped within the clot |
The Normal Clotting Process
The clotting process is complex and helps prevent too much bleeding. When a blood vessel is injured, it starts. This involves platelets sticking together and fibrin forming through chemical reactions.
The clot stops blood loss and helps healing start. Knowing how a blood clot forms is key to understanding its role in health.
Physical Characteristics: Are Blood Clots Hard or Soft?
The hardness or softness of blood clots is key to understanding their impact on health. We’ll look at what makes blood clots vary in texture and appearance. These differences can be quite significant.
Blood clots can be soft and fragile or hard and firm. This depends on their age and what they’re made of. Fresh clots are softer and can break easily. Older clots are harder and more solid.
Texture and Appearance Variations
The look and feel of blood clots change based on where they form in the body. Clots in areas with fast blood flow are different from those in slower areas.
Some clots look red or purple because of red blood cells. Others appear white or pale, made mostly of platelets and fibrin.
How Clot Composition Affects Consistency
The type of material in a blood clot affects its firmness. Clots with more fibrin are firmer. Those with more red blood cells are softer and easier to dissolve.
Knowing what makes clots different is important for treating them. It helps manage the risks of blood clots.
Medical Terminology: Names for Blood Clots
Knowing the difference between a stationary and a moving blood clot is key in medical terms. It’s important for doctors and patients to understand these terms well.
Stationary Clots: What is a Thrombus?
A thrombus is a blood clot that stays in one place inside a blood vessel. It’s made of platelets, fibrin, and other blood parts. The process of making a thrombus involves many steps and cell interactions.
Thrombi can happen in both arteries and veins. They can cause big health problems. For example, an artery thrombus can block blood to the heart, leading to a heart attack. A vein thrombus can cause deep vein thrombosis (DVT).
A Moving Blood Clot is Called an Embolus
An embolus is a clot that moves through the blood. It forms when a thrombus breaks off. An embolus can block a smaller vessel, causing an embolism.
The main difference is that a thrombus stays put, while an embolus moves. This makes an embolus more dangerous because it can travel and cause serious problems.
| Term | Description | Characteristics |
| Thrombus | A blood clot that forms within a blood vessel | Stationary, remains at the site of formation |
| Embolus | A clot that breaks loose and travels through the bloodstream | Mobile can lodge in smaller vessels |
It’s vital to know the medical terms for blood clots to diagnose and treat them. By knowing the difference between a thrombus and an embolus, doctors can give better care and prevent complications.
Different Kinds of Blood Clots: The 7 Main Types
It’s important to know about the different blood clots to spot health risks early. Blood clots vary by location, composition, and other factors. Each type has its own risks and treatment needs.
Overview of Classification Methods
Blood clots are divided into two main types: arterial and venous. Arterial clots, or “white clots,” form in arteries and are made of platelets and fibrin. Venous clots, or “red clots,” are in veins and have more red blood cells. This helps doctors choose the right treatment.
Doctors say knowing about blood clots is key to understanding their causes and effects.
“Thrombosis is a complex process, and understanding its various forms is key to managing and treating it effectively.” We will explore the different types of blood clots, including arterial thrombi, venous thrombi, deep vein thrombosis (DVT), pulmonary embolism, superficial venous thrombosis, and microclots.
How Location Affects Clot Characteristics
The place a blood clot forms changes its characteristics and risks. For example, clots in deep veins can cause deep vein thrombosis (DVT). These clots can travel to the lungs and cause a pulmonary embolism. Clots in superficial veins are usually less dangerous but can cause discomfort.
The type and location of a blood clot affect its symptoms and treatment. Arterial clots can cause sudden symptoms like chest pain or stroke. Venous clots may lead to swelling and pain in the affected limb.
Knowing these differences helps doctors diagnose and treat blood clots better.
Arterial Thrombi: The “White Clots”
We look into the characteristics and risks of arterial thrombi, also known as “white clots.” These clots form in arteries, which carry blood away from the heart. They are made of platelets and fibrin, making them white.
Formation and Distinguishing Features
Arterial thrombi often form due to atherosclerosis. This is when arteries get damaged and narrow because of plaque buildup. This damage causes blood to flow unevenly, leading to the formation of a thrombus.
Arterial thrombi are white because they have a lot of platelets. They are firmer and more stable than other clots. This makes them more likely to block blood flow, leading to serious problems.
Common Locations and Associated Conditions
Arterial thrombi usually occur in arteries with a lot of atherosclerotic disease. They often occur in the coronary, carotid, and peripheral arteries. A thrombus in these areas can cause serious issues like myocardial infarction (heart attack) or stroke.
Things like high blood pressure, high cholesterol, diabetes, and smoking can increase the risk. These conditions help atherosclerosis develop, making it more likely for a thrombus to form.
Risks and Complications
The risks of arterial thrombi are serious and can be deadly. If a thrombus blocks blood flow, it can cause sudden ischemia and damage to organs. For example, a thrombus in the coronary artery can lead to a heart attack, while one in the carotid artery can cause a stroke.
Chronic conditions like peripheral arterial disease can also happen due to these clots. It’s important to manage and prevent these risks to improve patient outcomes.
Venous Thrombi: The “Red Clots”
Venous thrombi are blood clots that form in veins. They are called “red clots” because of their red color. This color comes from red blood cells, fibrin, and platelets.
Development of Venous Clots
Venous thrombi form in veins. They can happen because of issues with blood flow or clotting. Things like being immobile for a long time, having a family history, or certain health conditions can raise the risk.
Knowing the risk factors is key to preventing and treating these clots early. These clots often relate to Virchow’s triad. This includes blood stasis, hypercoagulability, and damage to the inner lining of veins.
Identifying Characteristics
Venous thrombi are different from arterial clots. They are more fragile and less firm. They are often linked to deep vein thrombosis (DVT).
| Characteristics | Description |
| Composition | Primarily red blood cells, fibrin, and platelets |
| Appearance | Red due to high red blood cell content |
| Location | Veins, often in lower extremities |
Potential Health Consequences
Venous thrombi can cause serious problems. One big risk is pulmonary embolism. This is when a clot breaks loose and goes to the lungs. It can be very dangerous.
If you notice symptoms or they get worse, get medical help right away. Quick action can make a big difference in treatment outcomes.
Deep Vein Thrombosis (DVT): Clots in Deep Veins
A blood clot in the deep veins is called Deep Vein Thrombosis (DVT). It’s a serious condition that needs quick action. DVT happens when a blood clot forms in the deep veins, usually in the legs.
Risk Factors and Common Locations
Many things can raise your risk of getting DVT. These include prolonged immobility, family history, and some health issues. The deep veins in the lower legs are most often affected.
Being immobile for a long time can increase your risk of DVT. It causes blood to pool in the deep veins, making clots more likely.
A Medical Expert
Symptoms and Warning Signs
It’s important to know the signs of DVT to get help early. Common signs include swelling, pain, and discoloration in the affected limb.
- Swelling in the affected leg
- Pain or tenderness, specially when standing or walking
- Redness or discoloration of the affected area
Complications and Long-term Effects
If DVT is not treated, it can cause serious problems. One big risk is pulmonary embolism. Knowing the long-term effects helps manage the condition better.
Pulmonary Embolism: When Clots Travel to the Lungs
A blood clot that travels to the lungs is a serious condition called pulmonary embolism. It happens when a clot in the deep veins of the legs breaks free. This clot then blocks blood flow in the lungs. It’s a medical emergency that needs quick attention.
How Pulmonary Emboli Form
Pulmonary emboli start with a blood clot in a deep vein, known as deep vein thrombosis (DVT). Risks for DVT include being immobile for a long time, having a family history, and certain health conditions. When a piece of this clot breaks off, it can travel to the lungs, causing a pulmonary embolism.
Key factors that contribute to the formation of pulmonary emboli include:
- Prolonged bed rest or immobility
- Genetic clotting disorders
- Cancer and its treatment
- Major surgery or trauma
Recognizing a Pulmonary Embolism
It’s important to know the symptoms of pulmonary embolism to get help fast. Common signs include:
- Shortness of breath
- Chest pain that worsens with deep breathing
- Coughing up blood
- Rapid heart rate
- Lightheadedness or dizziness
If you or someone you know has these symptoms, get medical help right away.
Emergency Response and Treatment
Treating pulmonary embolism means acting fast to stop more clotting and dissolve the clot. Doctors might use medicines, thrombolytic therapy, or surgery in serious cases.
Quick treatment can greatly help patients with pulmonary embolism. It’s key to know the signs and get medical help fast. This can lower the risk of serious problems and improve survival chances.
Superficial Venous Thrombosis: Clots in Surface Veins
Clots in surface veins, or superficial venous thrombosis, can cause a lot of discomfort. They need medical attention. This condition is a blood clot in veins near the skin’s surface. It’s different from deep vein thrombosis (DVT) because it happens in veins closer to the skin.
Distinguishing from Deep Vein Thrombosis
Superficial venous thrombosis and DVT both involve blood clots. But, they are not the same. Superficial venous thrombosis is usually less severe but needs proper treatment.
The main differences are:
- The location of the clot: Superficial venous thrombosis is in superficial veins, while DVT is in deeper veins.
- Symptoms: Superficial venous thrombosis has localized pain, redness, and swelling. DVT can cause more widespread symptoms.
| Characteristics | Superficial Venous Thrombosis | Deep Vein Thrombosis |
| Location | Superficial veins | Deep veins |
| Severity | Generally less severe | Can be life-threatening |
| Symptoms | Localized pain, redness, swelling | More widespread symptoms, potentially including limb discoloration |
Treatment Approaches and Prognosis
Treatment for superficial venous thrombosis includes both conservative management and anticoagulant therapy. The main goals are to ease symptoms, prevent clot extension, and reduce complications.
Common treatments are:
- Warm compresses to reduce discomfort.
- NSAIDs to manage pain and inflammation.
- Compression stockings to improve blood flow.
- Anticoagulant therapy in selected cases to prevent clot progression.
A medical expert notes, “Early diagnosis and proper management of superficial venous thrombosis are key to preventing complications and improving outcomes.”
The prognosis for superficial venous thrombosis is generally good with the right treatment. But, it’s important for patients to watch for complications and seek medical help if symptoms get worse or don’t improve with treatment.
Microclots: Small But Potentially Dangerous
Microclots are tiny blood clots that can block capillaries. This can lead to serious health problems. They have become a focus in medical research, mainly with COVID-19.
How Microclots Affect Capillaries
Microclots can harm capillaries, which are key for exchanging oxygen, nutrients, and waste. When they block these tiny blood vessels, it can damage tissues and organs. The effects of microclots can range from mild to life-threatening.
Research shows microclots are a big problem in severe COVID-19 cases. They add to the disease’s complexity. Knowing how microclots form and affect capillaries is key to finding new treatments.
Emerging Research and Clinical Significance
New studies are uncovering the role of microclots in diseases. They are looking into how microclots form, their effects on organs, and possible treatments. Microclots are very important in understanding many diseases.
As we learn more about microclots, we’ll get better at diagnosing and treating related conditions. We’re moving towards a deeper understanding of microclots and their impact on health. This will guide future medical practices and research.
Critical Blood Clots: Brain, Heart, and Abdominal Clots
Blood clots in key areas of the body can be very dangerous. They can happen in the brain, heart, and abdomen. This can lead to serious health issues. It’s important to know about these risks and how to get help quickly.
Cerebral Thrombosis and Stroke
A blood clot in the brain’s blood vessels can cause a stroke. A stroke happens when blood flow to the brain stops. This can damage the brain a lot, leading to disabilities or death.
Signs of a stroke include sudden weakness, trouble speaking, and vision problems. Getting medical help fast is key to reducing brain damage.
Coronary Thrombosis and Heart Attack
Coronary thrombosis occurs when a clot blocks the heart’s blood supply. This can cause a heart attack, damaging the heart muscle.
Heart attack symptoms include chest pain, shortness of breath, and nausea. Quick medical care is needed to save the heart.
| Condition | Symptoms | Consequences |
| Cerebral Thrombosis | Sudden weakness, numbness, difficulty speaking | Stroke, brain damage, death |
| Coronary Thrombosis | Chest pain, shortness of breath, nausea | Heart attack, heart damage, death |
| Mesenteric Thrombosis | Severe abdominal pain, nausea, vomiting | Intestinal damage, infection, death |
Mesenteric Thrombosis and Abdominal Complications
Mesenteric thrombosis is a clot in the intestines’ blood vessels. It causes severe pain, nausea, and vomiting. Without quick treatment, it can damage the intestines or cause gangrene.
The symptoms of mesenteric thrombosis can be hard to spot. But, fast surgery is often needed to save the intestines and prevent worse problems.
Conclusion: Prevention and When to Seek Help
It’s important to know about different blood clots and their signs. We’ve looked at various types, like arterial and venous thrombi, and deep vein thrombosis. Understanding these can help keep us healthy and know when to get medical help.
Preventing blood clots is key. By knowing the risks and taking steps to lower them, we can avoid many problems. This means living a healthy lifestyle, knowing our family’s health history, and managing any health issues we have.
Knowing when to get help is also critical. If symptoms get worse or don’t go away, we should see a doctor right away. We should all be proactive about our health and talk to doctors if we’re worried about blood clots or other health issues.
By staying informed and taking steps to prevent blood clots, we can all help reduce their occurrence. This is important for our health and safety.
FAQ
What are the different types of blood clots?
There are many types of blood clots. These include arterial thrombi, venous thrombi, and deep vein thrombosis. There’s also pulmonary embolism, superficial venous thrombosis, and microclots. Each type has its own risks and characteristics.
Are blood clots hard or soft?
Blood clots can be either soft and jelly-like or hard and firm. This depends on their age and what they’re made of.
What is a blood clot called when it is stationary?
A stationary blood clot is called a thrombus.
What is a moving blood clot called?
A moving blood clot is called an embolus.
What are the risks associated with different types of blood clots?
Different blood clots pose different risks. For example, a clot in the brain can cause a stroke. A clot in the heart can lead to a heart attack. Pulmonary embolism is another serious risk, as is damage to organs.
How do blood clots form?
Blood clots form when platelets and fibrin come together. This is a natural response to injury. Many factors can influence this process, including blood flow and the condition of the blood vessels.
What is deep vein thrombosis (DVT)?
Deep vein thrombosis is a blood clot in the deep veins, usually in the legs. It can cause pain, swelling, and warmth.
What is a pulmonary embolism?
A pulmonary embolism happens when a blood clot travels to the lungs. It can cause shortness of breath, chest pain, and coughing.
Can blood clots be prevented?
Yes, preventing blood clots is possible. You can do this by living a healthy lifestyle, staying hydrated, exercising regularly, and managing any health conditions you have.
When should I seek medical help for a suspected blood clot?
Seek medical help right away if you have severe pain, swelling, or trouble breathing. This is also true if you think you have a clot in a critical area like the brain, heart, or lungs.
References:
- Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. https://www.sciencedirect.com/science/article/pii/S0049384820301567



































