Last Updated on November 27, 2025 by Bilal Hasdemir

Cancer treatments have greatly improved, saving many lives. Yet, we must acknowledge the risks these treatments pose. At Liv Hospital, we focus on patient care and understanding the risks of secondary cancers from chemotherapy and radiation.
Some chemotherapy drugs, like alkylating agents and platinum-based drugs, can raise the risk of MDS and AML. Radiation therapy also increases the chance of solid tumors and sarcomas. We are committed to providing complete care that addresses these risks.
Key Takeaways
- Chemotherapy and radiation treatments can increase the risk of secondary cancers.
- Certain chemotherapy drugs are associated with a higher risk of MDS and AML.
- Radiation therapy can cause solid tumors and sarcomas.
- Awareness of these risks is key for cancer survivors.
- Liv Hospital is dedicated to providing complete care for cancer patients.
The Double-Edged Sword of Cancer Treatment

Cancer treatment is a complex field. It’s important to know the balance between fighting cancer and the chance of getting secondary cancers. Treatments aim to kill cancer cells but can harm healthy ones too, leading to long-term issues.
Defining Secondary Cancers vs. Recurrence
Secondary cancers are new cancers that come after treatment, different from when the original cancer comes back. Knowing this difference is key for survivors. It affects how they follow up and stay watched.
Overall Risk Statistics
The chance of getting secondary cancers is low, hitting about 1-3% of cancer survivors. But, this risk changes based on the treatment type. Some chemotherapy and radiation increase this risk more.
| Treatment Type | Secondary Cancer Risk |
|---|---|
| Chemotherapy | Increased risk with alkylating agents and platinum-based drugs |
| Radiation Therapy | Risk varies with dose and field size |
Even though the risk is low, knowing what causes secondary cancers is key. It helps in creating better ways to watch and prevent them.
Understanding How Chemotherapy Causing Cancer Works
Chemotherapy is a lifesaver for many cancer patients. But it also has a risk of causing secondary cancers. We must understand these risks to manage and possibly reduce them.
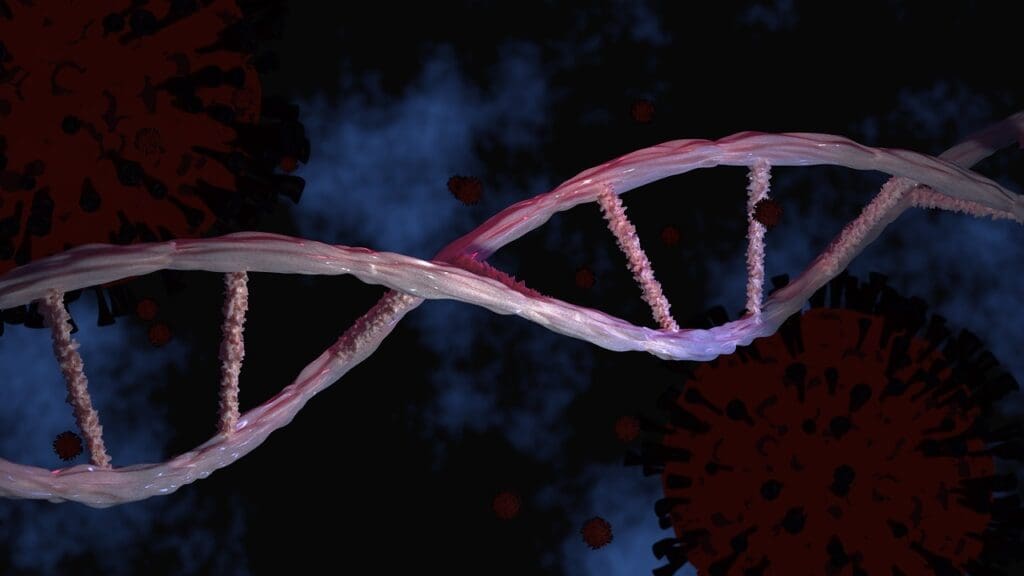
DNA Damage Mechanisms
Chemotherapy drugs target fast-growing cells, including cancer and some healthy cells. This can cause DNA damage, a key way secondary cancers develop. The issue is that these drugs can’t always tell the difference between cancer and healthy cells. This leads to genetic changes in the cells that survive.
Timeframe for Secondary Cancer Development
The time it takes to develop secondary cancers after chemotherapy varies. Knowing this timeline is key to watching for and possibly stopping these cancers.
Short-term Risks (2-5 years)
Some secondary cancers, like certain types of leukemia, can appear within a few years after treatment. These risks are often linked to specific chemotherapy drugs.
Long-term Risks (5-20+ years)
Other secondary cancers may take longer, sometimes showing up a decade or more after treatment. The risk of these cancers depends on the chemotherapy type and the patient’s health.
| Timeframe | Common Secondary Cancers | Risk Factors |
|---|---|---|
| 2-5 years | Acute Leukemias | Alkylating agents, Topoisomerase II inhibitors |
| 5-20+ years | Solid tumors (e.g., breast, lung) | Radiation therapy, Alkylating agents |
Alkylating Agents: The First Pathway to Secondary Malignancies
Chemotherapy with alkylating agents has both good and bad sides. It helps fight cancer but might also raise the chance of getting another cancer later. These drugs add an alkyl group to cancer cells’ DNA, stopping them from copying themselves and killing them.
DNA Damage Mechanisms
Alkylating agents harm DNA by adding alkyl groups. This causes DNA strands to cross-link. This makes it hard for cells to copy their DNA, leading to cell death. But, it can also hurt normal cells, causing mutations and chromosomal damage, which might lead to secondary cancers.
Common Examples and Their Risk Profiles
Some well-known alkylating agents are cyclophosphamide, melphalan, and chlorambucil. They are used to treat cancers like lymphomas, leukemias, and solid tumors.
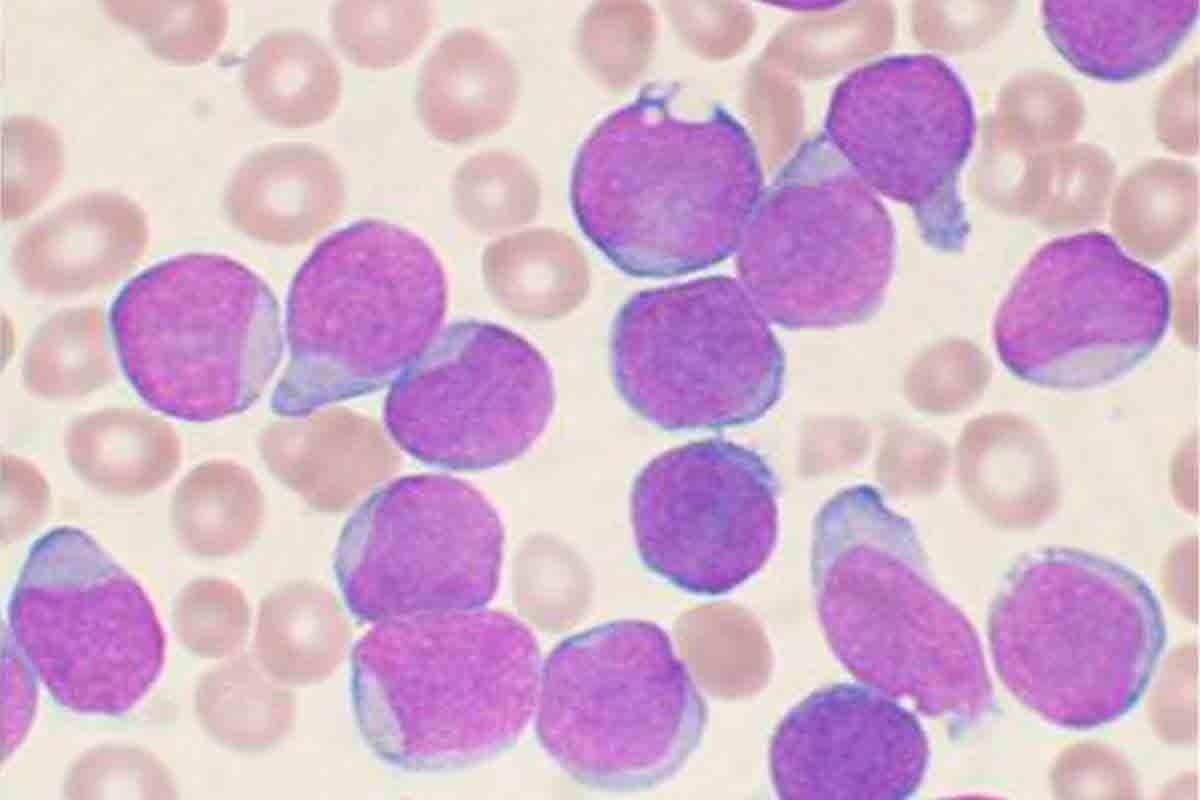
Cyclophosphamide and MDS/AML Risk
Cyclophosphamide is a common alkylating agent. It’s linked to a higher risk of myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). This risk is higher with high doses or when used with other drugs.
The chance of getting MDS/AML after treatment with cyclophosphamide depends on several things. These include the treatment dose and length, and the patient’s health.
Platinum-Based Chemotherapy: The Second Risk Pathway
Our study shows that platinum-based chemotherapy is a big risk for secondary cancers, like leukemia. This is because of how these drugs work. Cisplatin and carboplatin are common treatments for many cancers.
Mechanism of Cellular Damage
These chemotherapy drugs damage DNA in cancer cells, stopping them from growing. But, they also harm healthy cells. This can lead to genetic damage and secondary cancers.
Specific Leukemia Risks with Cisplatin and Carboplatin
Cisplatin and carboplatin increase the chance of getting secondary leukemias, like AML. The risk grows with higher doses and longer treatments.
| Drug | Leukemia Risk | Cumulative Dose Risk |
|---|---|---|
| Cisplatin | High | Increased risk at doses >600 mg/m |
| Carboplatin | Moderate | Increased risk at doses >1000 mg/m |
It’s important to know the risks of platinum-based chemotherapy. This helps in managing and reducing the chance of secondary cancers in cancer survivors.
Topoisomerase II Inhibitors: The Third Risk Factor
Topoisomerase II inhibitors are good against some cancers but can raise the risk of new cancers. They block the enzyme topoisomerase II, which helps with DNA copying and fixing. This can cause DNA damage, leading to new cancers.
How These Drugs Affect DNA Repair
These drugs can cause DNA double-strand breaks. If not fixed right, this can lead to genetic changes and chromosomal problems. Sometimes, the body can’t fix this damage well, leading to mutations that might cause new cancers.
Risk Timeline for Developing MDS and AML
The time it takes to develop Myelodysplastic Syndromes (MDS) and Acute Myeloid Leukemia (AML) after using these drugs varies. Some cases happen soon after treatment, while others may take years. Several things can affect this timeline, including:
- The specific topoisomerase II inhibitor used
- The dose and duration of treatment
- Individual patient factors, such as genetic predisposition
It’s important to understand the risks of topoisomerase II inhibitors for cancer treatment. Knowing the chance of new cancers helps doctors keep a closer eye on patients. They can then work on ways to lower these risks.
Radiation-Induced Solid Tumors: The Fourth Pathway
We’re making great strides in beating cancer with radiation therapy. But, we must also face its dark side: it can cause new tumors. Radiation fights cancer but can harm healthy tissues, leading to new cancers.
Dose-Dependent Cancer Risk
The chance of getting new tumors from radiation depends on how much and for how long you’re exposed. Higher doses and bigger treatment areas raise the risk. We need to weigh the good of radiation against the risk of new cancers.
Most Common Secondary Solid Tumors
Common new tumors from radiation include breast cancer from chest radiation and thyroid cancer from neck radiation.
Breast Cancer After Chest Radiation
Young women who get chest radiation, like for Hodgkin lymphoma, face a higher risk of breast cancer later. Regular checks and monitoring are key for catching it early.
Thyroid Cancer After Neck Radiation
Neck radiation, often in kids, boosts the risk of thyroid cancer. Keeping a close eye on these patients is vital.
Knowing these risks helps us create better care plans for cancer survivors. This way, we can catch and treat new cancers early, reducing their number.
Radiation-Induced Sarcomas: The Fifth Risk Mechanism
Radiation therapy saves lives but can also cause secondary cancers, like sarcomas. These rare tumors grow in connective tissue exposed to radiation. We’ll look into how this happens and what increases the risk of getting these sarcomas.
How Radiation Damages Connective Tissue
Radiation therapy harms not just cancer cells but also healthy tissue around them. The connective tissue, which includes bones, fat, and muscles, gets damaged. This damage can cause genetic mutations in these cells, leading to sarcomas. The risk of these mutations depends on the radiation’s dose and intensity.
Typical Latency Period and Risk Factors
The time between radiation exposure and sarcoma development can be long, often 10 to 20 years or more. Several factors increase the risk of getting sarcomas. These include the radiation dose, age at treatment, and genetic predispositions. Knowing these risk factors helps in monitoring and reducing the risk of secondary sarcomas in cancer survivors.
By recognizing the risks and understanding how radiation-induced sarcomas occur, we can help patients better. We provide them with care that addresses their current and future health needs.
Combined Modality Treatment: The Sixth Risk Multiplier
Cancer survivors who get combined modality treatment face a higher risk of secondary cancers. This is because chemotherapy and radiation work together, causing more damage to healthy cells. This approach is used for aggressive or advanced cancers.
Synergistic Effects of Chemo and Radiation
Chemotherapy and radiation together can cause more harm to cells. This can lead to DNA damage in healthy cells, raising the risk of secondary cancers. Studies show that those who get both treatments face a higher risk than those who get only one study.
Most Common Secondary Cancer After Leukemia
Leukemia survivors are at a higher risk for secondary cancers. These include other leukemias and solid tumors. The most common are t-MDS and t-AML, which can happen months to years after treatment.
It’s important to understand the risks of combined modality treatment. This helps in creating better follow-up care for cancer survivors. Healthcare providers can then work to reduce these risks and improve patient outcomes.
Age and Genetic Susceptibility: The Seventh Risk Pathway
Understanding secondary cancer risks involves looking at age and genetics. Both are key in figuring out who might get secondary cancers.
Why Children Face Higher Secondary Cancer Risks
Children are more at risk for secondary cancers because their bodies are growing. They live longer, giving more time for these cancers to appear. Studies show that kids who get strong treatments like chemo and radiation are at even higher risk as highlighted in a recent Nature.
Genetic Predispositions That Increase Vulnerability
Genetics also play a big part in secondary cancer risk. We’re talking about DNA repair gene mutations and cancer predisposition syndromes.
DNA Repair Gene Mutations
When DNA repair genes mutate, the body can’t fix damage from cancer treatments. This makes it more likely for secondary cancers to develop. For example, BRCA1 and BRCA2 gene mutations affect how DNA is repaired.
Cancer Predisposition Syndromes
Cancer syndromes like Li-Fraumeni make people more likely to get multiple cancers. This is because they have inherited genetic mutations. People with these syndromes are more sensitive to the cancer-causing effects of treatments.
| Genetic Predisposition | Description | Impact on Secondary Cancer Risk |
|---|---|---|
| DNA Repair Gene Mutations | Impaired DNA repair mechanisms | Increased risk due to accumulated genetic damage |
| Cancer Predisposition Syndromes | Inherited genetic mutations | Higher vulnerability to treatment-induced cancers |
Knowing about these genetic factors helps doctors create better treatment plans. They can focus on treatments that lower the risk of secondary cancers. This is important for people with certain genetic traits.
Monitoring, Prevention and Risk Reduction Strategies
To lower the risk of secondary cancers, cancer survivors need good monitoring and prevention plans. We know that caring for survivors well means using many strategies. These include regular check-ups, new treatments, and plans made just for them.
Recommended Screening Protocols for Cancer Survivors
Screening regularly is key to catching secondary cancers early. We suggest that survivors get a screening plan that fits their risk and past treatments. This might include yearly mammograms, colonoscopies, or other tests as their doctor advises.
Emerging Treatment Approaches to Minimize Secondary Cancer Risk
New treatments aim to cut down secondary cancer risks. They use precision medicine and targeted therapies to lessen the need for old treatments like chemo and radiation. We’re also looking into immunotherapy to improve treatment and lower long-term risks.
The Role of Genetic Testing in Risk Assessment
Genetic testing is vital for figuring out secondary cancer risks. It helps us give survivors advice based on their genes. This lets them take steps to manage their risk better.
By using screening plans, new treatments, and genetic testing, we can greatly lower secondary cancer risks. Our aim is to give each survivor the care they need, tailored just for them.
Conclusion: Balancing Treatment Benefits Against Future Risks
Cancer treatments save lives but also come with risks of secondary cancers. It’s key to weigh treatment benefits against future risks to help cancer survivors. We’ve looked at how chemotherapy and radiation can lead to secondary cancers.
These risks include DNA damage and the effects of certain drugs and radiation. Knowing these risks helps patients and doctors work together. This way, they can lower the chances of secondary cancers.
It’s important to be aware, monitor, and take steps to prevent secondary cancers. This includes regular screenings and new treatments that aim to reduce risks. Genetic testing also plays a role in assessing these risks.
By focusing on both treatment benefits and future risks, we can improve life for cancer survivors. This approach ensures patients get the best care from start to finish.
FAQ
Can chemotherapy cause secondary cancer?
Yes, some chemotherapy drugs can raise the risk of secondary cancers. This is because they damage DNA.
How does radiation therapy cause secondary cancer?
Radiation therapy can damage normal cells’ DNA. This leads to genetic mutations that might cause cancer. The risk depends on the dose and the area treated.
What are the most common secondary cancers after leukemia treatment?
After leukemia treatment, common secondary cancers include breast, thyroid, and sarcomas. Myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML) are also common.
Are children more susceptible to secondary cancer risks after chemotherapy and radiation?
Yes, children are more at risk due to their developing bodies. They are more likely to get secondary cancers from treatment.
Can genetic predispositions increase the risk of secondary cancers?
Yes, some genetic conditions make people more likely to get secondary cancers. This is because their bodies can’t repair DNA damage well.
What screening protocols are recommended for cancer survivors to detect secondary cancers early?
Cancer survivors should follow specific screening guidelines. These depend on their cancer type and treatment. Regular check-ups and screenings are key.
Are there emerging treatment approaches designed to minimize secondary cancer risks?
Yes, new treatments aim to lower secondary cancer risks. These include targeted therapies and personalized medicine.
How does combined modality treatment (chemotherapy and radiation) affect secondary cancer risk?
Combined treatments can increase secondary cancer risk. This is because they work together to damage DNA and cells.
Can secondary cancers be prevented or their risk reduced?
While total prevention is not possible, risks can be lowered. This is by understanding individual risks, following screening guidelines, and using new treatments.
Does the type of chemotherapy drug used affect the risk of secondary cancer?
Yes, different chemotherapy drugs have different risks. For example, alkylating agents and platinum-based drugs are higher risks.
How long after treatment can secondary cancers occur?
Secondary cancers can happen years or even decades after treatment. The time frame depends on treatment type, age, and individual risk.
References
- American Cancer Society (ACS): https://www.cancer.org/cancer/survivorship/long-term-health-concerns/second-cancers-in-adults/treatment-risks.html
- National Center for Biotechnology Information (NCBI) / PMC: https://pmc.ncbi.nlm.nih.gov/articles/PMC6435077/
- National Center for Biotechnology Information (NCBI) / Bookshelf: https://www.ncbi.nlm.nih.gov/books/NBK13999/
- National Cancer Institute (NCI) / DCEG: https://dceg.cancer.gov/research/what-we-study/second-cancers