Last Updated on November 17, 2025 by Ugurkan Demir
Spotting B12 and folate deficiency early is key. These conditions share some lab signs but have different health effects. At Liv Hospital, we focus on top-notch care and patient needs. We make sure to test thoroughly and diagnose accurately for the best results.
b12 vs folate deficiency which are vital for our bodies. Not having enough of either can cause serious health problems. We’ll look at how these deficiencies show up differently in symptoms and lab tests. This will help us dive deeper into the topic in the next parts.
Key Takeaways
- Telling B12 and folate deficiency apart is key because of their different health impacts.
- Both can cause megaloblastic anemia, but show different signs in labs and symptoms.
- B12 deficiency often brings on nerve problems, while folate mainly affects blood cells.
- Getting the right diagnosis needs careful testing and knowing the differences.
- Liv Hospital aims to offer top healthcare with full support for international patients.
Understanding B12 and Folate: Roles in the Body
It’s key to know how vitamin B12 and folate work in our bodies. They help with DNA making, red blood cell creation, and brain health.
Vitamin B12 Functions and Metabolism
Vitamin B12 is vital for making DNA, fatty acids, and energy. It helps in metabolizing fatty acids and amino acids. This is important for making red blood cells.
It also keeps our nervous system healthy by making myelin. Myelin is the fatty stuff that protects our nerves.
The way our bodies break down vitamin B12 is complex. It needs specific proteins to absorb and move around. Not having enough vitamin B12 can mess up DNA making and brain function.
Folate Functions and Metabolism
Folate, or vitamin B9, is also key for DNA making and fixing, and for amino acid metabolism. It helps make red blood cells and stops anemia. Folate also helps turn homocysteine into methionine, which keeps blood healthy.
Folate gets changed into 5-methyltetrahydrofolate, its most active form. This process ties in with vitamin B12, as both are part of the methylation cycle.
Interconnected Biochemical Pathways
The ways vitamin B12 and folate work together are important. They’re linked in DNA making and homocysteine methylation. Not having enough of either can cause similar problems, like big red blood cells.
Getting how these pathways work together is key to finding and fixing vitamin B12 and folate shortages. It shows why we should look at both vitamins when we see similar symptoms or lab results.
B12 vs Folate Deficiency: Pathophysiological Differences
It’s important to know how B12 and folate deficiencies are different. Both can cause similar blood problems, but they start from different causes
Mechanisms Leading to B12 Deficiency
B12 deficiency often comes from not being able to absorb it well. This can happen due to gastric mucosa atrophy, pernicious anemia, or if part of the ileum is removed. Vegans or those who don’t eat enough animal products can also get it.
“The most common cause of B12 deficiency is pernicious anemia,” medical texts say. This is an autoimmune disease that damages the stomach’s lining. It stops the body from making a protein needed to absorb B12.
Mechanisms Leading to Folate Deficiency
Folate deficiency is often linked to not getting enough folate from food. This is common in people who don’t eat enough fresh fruits and veggies. It can also happen if someone has celiac disease or has had part of their small bowel removed.
Pregnancy also increases the need for folate. “Folate needs go up during pregnancy to help the baby grow,” health experts say. This is why pregnant women often need to take folate supplements.
Shared Pathways in DNA Synthesis
Even though they start from different places, B12 and folate are both key in making DNA. They help turn homocysteine into methionine, which is vital for making new DNA and fixing old DNA.
The methylation cycle is where B12 and folate work together. B12 helps turn homocysteine into methionine. It uses folate’s active form as a donor of methyl groups.
- Both deficiencies can lead to megaloblastic anemia because of problems with DNA synthesis
- Their shared role in DNA synthesis is why they can cause similar blood issues.
- Knowing this helps doctors find the right treatments for both deficiencies.
Clinical Manifestations: How Symptoms Differ
It’s important to know how B12 and folate deficiencies show up differently. Both can cause similar blood issues, but their effects on the brain and body are quite different.
Neurological Symptoms in B12 Deficiency
Vitamin B12 plays a key role in making myelin, which protects nerves. Neurological symptoms include neuropathy, balance problems, and brain fog. Experts warn that these symptoms can be severe and permanent if not treated.
The impact of these symptoms can greatly affect a person’s quality.
Folate deficiency doesn’t usually cause direct brain problems. But it can affect brain function by changing homocysteine levels.
Hematologic Manifestations in Both Deficiencies
Both B12 and folate deficiencies can cause macrocytic anemia. This is when red blood cells are too big and don’t work properly. Symptoms include tiredness, weakness, and trouble breathing.
As a clinical expert notes, “Macrocytic anemia shows how vital these vitamins are for making DNA and red blood cells.”
Unique Clinical Presentations
B12 and folate deficiencies have some similar signs, but they also have their own special features. B12 deficiency is known for its unique neurological symptoms. Folate deficiency, on the other hand, is linked to fast cell growth, like in pregnancy or certain anemias.
Knowing these differences helps doctors figure out what’s wrong and how to treat it.
In summary, while B12 and folate deficiencies share some symptoms, their unique signs, like neurological issues, are key to diagnosis and treatment.
7 Key Laboratory Differences Between B12 and Folate Deficiency
It’s important to know the differences in lab tests for B12 and folate deficiency. These tests help doctors treat patients right. B12 and folate deficiencies look similar but need different treatments.
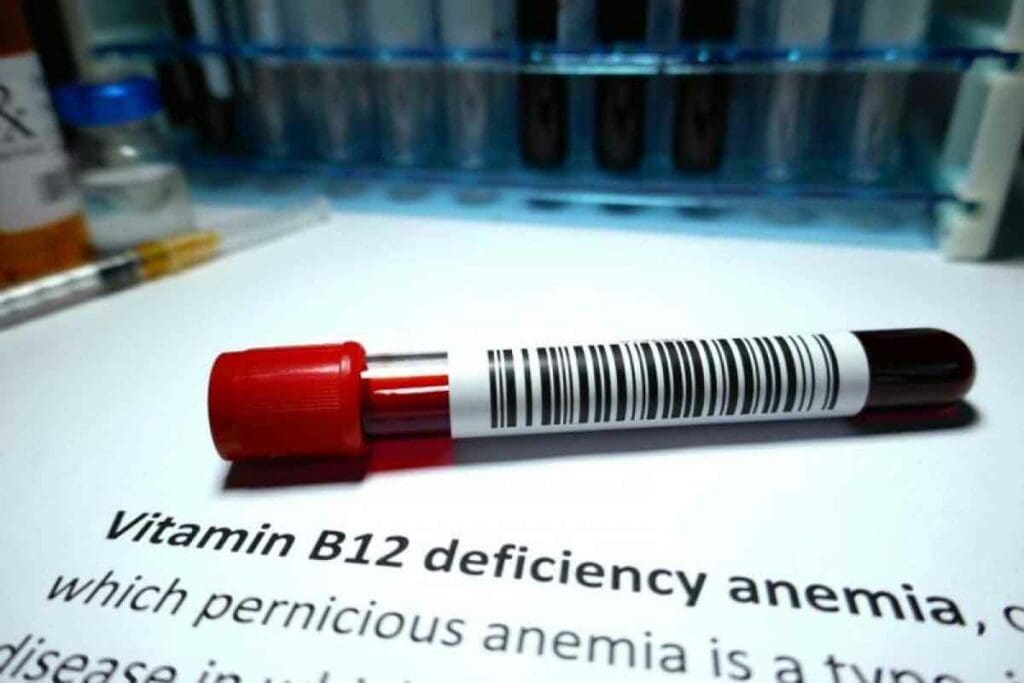
1. Serum B12 and Folate Levels
To tell B12 and folate deficiency apart, we look at their serum levels. Serum vitamin B12 levels are low in B12 deficiency. On the other hand, serum folate levels are normal or high unless folate deficiency is also present.
In folate deficiency, serum folate levels are low. B12 levels might be normal or low if there’s a mix of deficiencies.
2. Methylmalonic Acid (MMA) Levels
Methylmalonic acid (MMA) shows B12 deficiency well. High MMA levels mean B12 deficiency, even if serum B12 is close to normal.
3. Homocysteine Levels
Both B12 and folate affect homocysteine levels. So, high homocysteine levels can point to either deficiency. But homocysteine isn’t specific to either. It’s used with other tests for diagnosis.
4. Complete Blood Count Parameters
A complete blood count (CBC) helps diagnose B12 and folate deficiencies. Both can cause macrocytic anemia, with high mean corpuscular volume (MCV). But macrocytosis can also happen in other conditions.
Here’s a quick summary of the key differences in lab tests for B12 and folate deficiency:
- Serum B12 levels are low in B12 deficiency.
- Serum folate levels are low in folate deficiency.
- MMA levels are elevated in B12 deficiency.
- Homocysteine levels are high in both deficiencies.
Knowing these lab differences helps doctors diagnose and treat B12 and folate deficiencies correctly. This ensures patients get the right care.
Common Laboratory Findings in Both Deficiencies
Laboratory tests are key in spotting B12 and folate deficiencies. They show similar signs, making it vital to know these for correct diagnosis.
Macrocytic Anemia Characteristics
Macrocytic anemia is a big sign of both B12 and folate deficiencies. It shows red blood cells are bigger than usual. The number of red blood cells also goes down. The mean corpuscular volume (MCV) is high, showing macrocytosis. This is a key finding that needs more checking to find the cause.
Elevated Lactate Dehydrogenase (LDH)
High LDH levels are common in both B12 and folate deficiencies. LDH is in many body tissues, including red blood cells. When red blood cells break down, LDH gets into the blood, raising levels. This shows ineffective erythropoiesis and hemolysis, seen in both deficiencies.
Low Reticulocyte Count
A low reticulocyte count is seen in both B12 and folate deficiencies. Reticulocytes are young red blood cells. A low count means fewer new red blood cells are being made. This matches the megaloblastic anemia in both, where the bone marrow can’t make red blood cells well.
Increased Red Cell Distribution Width (RDW)
An increased RDW is common in both B12 and folate deficiencies. RDW shows how varied red blood cell sizes are. A high RDW means sizes vary more, showing megaloblastic anemia. This helps in diagnosing and tracking anemia’s severity.
At-Risk Populations and Screening Recommendations
It’s important to know who is most at risk for B12 and folate deficiencies. This helps in focusing on those who need screening the most. Both deficiencies have specific risk factors that doctors should watch out for.
High-Risk Groups for B12 Deficiency
Vitamin B12 deficiency is more common in some groups. This is because of diet, how the body absorbs it, and age. Here are the groups at higher risk:
- Older adults, due to decreased gastric acid production and atrophic gastritis
- Individuals with gastrointestinal disorders, such as Crohn’s disease or celiac disease
- Those who have undergone gastric bypass surgery
- Vegans and vegetarians who consume no animal products
- Patients taking certain medications, such as proton pump inhibitors and metformin
For these high-risk groups, regular B12 screening is advised. This is true, even if they show no symptoms or have other health issues.
High-Risk Groups for Folate Deficiency
Folate deficiency is common in certain groups, mainly because of diet and increased needs. The high-risk groups include:
- Pregnant women, due to increased folate requirements for fetal development
- Individuals with a diet lacking in folate-rich foods, such as leafy greens and legumes
- Those with alcohol dependence, as alcohol interferes with folate absorption
- Patients with malabsorption conditions, such as celiac disease
- Individuals taking certain medications, such as anticonvulsants and methotrexate
Screening for folate deficiency is key for pregnant women. It helps prevent neural tube defects in newborns.
Healthcare providers should keep these risk factors in mind when checking for B12 and folate deficiencies. Early detection through targeted screening can greatly improve health outcomes.
| Deficiency Type | High-Risk Groups | Screening Recommendations |
| B12 Deficiency | Older adults, gastrointestinal disorder patients, vegans/vegetarians, patients on certain medications | Regular screening, even with symptoms or related health issues |
| Folate Deficiency | Pregnant women, individuals with poor diets, alcohol-dependent individuals, and patients with malabsorption conditions | Screening during pregnancy, considering diet and health status |
Diagnostic Approach: Up-to-Date Guidelines and Best Practices
Identifying B12 and folate deficiencies requires a detailed diagnostic approach. This involves using the latest testing methods and carefully analyzing lab results. Guidelines suggest testing both vitamin B12 and folate levels together. This is because their symptoms can overlap, and deficiencies often occur together.
Current Recommendations for Testing
For diagnosing B12 and folate deficiencies, we follow certain testing guidelines. These include:
- Measuring serum vitamin B12 and folate levels simultaneously.
- Assessing methylmalonic acid (MMA) levels to confirm B12 deficiency.
- Evaluating homocysteine levels, which can be elevated in both deficiencies.
- Conducting a complete blood count (CBC) to identify macrocytic anemia.
Interpreting Laboratory Results
Understanding lab results is key to diagnosing B12 and folate deficiencies. For example:
| Laboratory Test | B12 Deficiency | Folate Deficiency |
| Serum B12 Level | Low | Normal |
| Serum Folate Level | Normal or Low | Low |
| MMA Level | Elevated | Normal |
| Homocysteine Level | Elevated | Elevated |
Differential Diagnosis Considerations
When diagnosing B12 and folate deficiencies, it’s important to look at other possible causes. These can include other nutritional deficiencies, chronic diseases, or medications that affect B12 or folate.
Special Considerations in Different Patient Populations
Some patient groups need special attention when diagnosing B12 and folate deficiencies. For example:
- Pregnant women have a higher demand for folate.
- Vegetarians and vegans are at higher risk for B12 deficiency due to dietary restrictions.
- Elderly individuals, who may have impaired B12 absorption.
Treatment Strategies and Monitoring
Understanding how to treat B12 and folate deficiencies is key to good patient care. It’s important not to just treat the deficiency but also watch how the patient responds. Then, adjust the treatment as needed.
B12 Deficiency Treatment Protocols
For B12 deficiency, vitamin B12 injections are usually the treatment. The first step is often getting injections, then moving to a maintenance phase.
- Initial Therapy: 1,000 mcg of vitamin B12 intramuscularly daily for the first week.
- Maintenance Therapy: 1,000 mcg intramuscularly monthly thereafter.
Oral supplements might be an option for mild cases or those who don’t like injections.
Folate Deficiency Treatment Protocols
Folate deficiency is treated with oral folic acid. The goal is to fill up folate stores and fix the cause of the deficiency.
- Initial Dose: 1-2 mg of folic acid orally per day.
- Maintenance: Keep taking supplements until the cause is fixed and folate levels are normal.
It’s important to treat B12 deficiency first before starting folic acid. This prevents or makes neurological symptoms worse.
Monitoring Response to Treatment
Checking how treatment is working means regular tests and doctor visits. Important things to watch include:
| Parameter | Expected Change | Timeline |
| Hemoglobin | Increase | 2-4 weeks |
| Reticulocyte Count | Increase | 1-2 weeks |
| MMA (for B12) | Decrease | Several weeks to months |
| Folate Levels | Normalization | Several weeks |
Potential Complications of Inappropriate Treatment
Wrong treatment can cause big problems. For example, using folic acid for B12 deficiency can hide blood problems but let nerve damage get worse.
On the other hand, too many B12 shots in people who don’t need them can cause low potassium levels. So, it’s vital to get the diagnosis right and tailor the treatment.
Conclusion: Clinical Pearls for Differentiating and Managing B12 and Folate Deficiencies
Distinguishing between B12 and folate deficiencies is key. They need different treatments, which can lead to serious issues. Knowing how to spot each one is vital for good care.
Important signs of B12 deficiency include nerve damage and brain problems. These symptoms don’t usually show up in folate deficiency. Blood tests help tell these two apart by checking B12 and folate levels, as well as MMA and homocysteine.
When treating these issues, finding the root cause is important. B12 often needs lifelong supplements, but folate might just need diet changes and supplements. Keeping an eye on how treatment works and making changes is critical to avoid problems.
Using these tips, doctors can help patients better and avoid wrong treatments. Understanding the unique signs and tests for B12 and folate is essential for good care.
FAQ
What are the main differences between vitamin B12 and folate deficiencies?
Vitamin B12 and folate deficiencies show different signs and lab results. B12 deficiency can cause nerve problems, but folate deficiency does not. Both can lead to a type of anemia called macrocytic anemia.
How do serum vitamin B12 and folate levels help differentiate between the two deficiencies?
Low B12 levels in the blood point to B12 deficiency. Low folate levels suggest folate deficiency. But other tests, like MMA and homocysteine levels, are also needed to confirm the diagnosis.
What is the significance of elevated MMA levels in B12 deficiency?
High MMA levels are a clear sign of B12 deficiency. This is because B12 is needed to break down MMA. This helps tell B12 deficiency apart from folate deficiency.
Can both B12 and folate deficiencies cause elevated homocysteine levels?
Yes, both B12 and folate deficiencies can raise homocysteine levels. This is because both vitamins help in breaking down homocysteine. But,ighh, homocysteine levels don’t point to just one deficiency.
What are the common laboratory findings in both B12 and folate deficiencies?
Both deficiencies can lead to macrocytic anemia, high LDH, low reticulocyte count, and high RDW. These signs point to a type of anemia but don’t single out either deficiency.
Who is at risk for B12 and folate deficiencies?
Older adults, vegetarians, and people with gut problems are more likely to have these deficiencies. It’s wise to screen these groups regularly.
How are B12 and folate deficiencies treated?
B12 deficiency is treated with B12 injections. Folate deficiency is fixed with oral supplements. It’s key to watch how the treatment works and adjust it if needed.
What are the possible complications of treating B12 and folate deficiencies wincorrectly
Wrong treatment, like using folate for B12 deficiency, can hide symptoms and cause nerve damage. It’s vital to diagnose correctly and tailor treatments to avoid harm.
How do high vitamin B12 and folate levels affect the diagnosis of deficiencies?
High levels of B12 and folate can happen in liver disease or after taking supplements. These findings need to be looked at with the patient’s symptoms and other lab results in mind.
What is the role of folate and B12 in DNA synthesis?
Both folate and B12 are key for DNA making. Without enough of either, DNA synthesis fails, leading to megaloblastic anemia.
References
- Allen, L. H. (2017). Vitamin B12 Deficiency: Recognition and Management. American Family Physician, 96(6), 384-389. Retrieved from https://www.aafp.org/pubs/afp/issues/2017/0915/p384.html
- StatPearls. (2024). Vitamin B12 Deficiency. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved September 10, 2024, from https://www.ncbi.nlm.nih.gov/books/NBK441923/