Pregnancy brings many changes to a woman’s body. One risk is the chance of getting blood clots. We’re here to help you understand this risk.
Pregnant women face a higher risk of blood clots than non-pregnant women. Spotting the signs early can save lives. At Liv Hospital, we stress the need to know the warning signs and risks of clots in pregnancy.

Key Takeaways
- Pregnant women are five times more likely to develop blood clots.
- Early recognition of signs can be life-saving.
- Understanding the risks is key for expectant mothers.
- Liv Hospital offers expert care and advice.
- Being informed helps manage clot risks.
Understanding Blood Clot Pregnancy: Why Expectant Mothers Are at Higher Risk
During pregnancy, women go through many changes that can make them more likely to get blood clots. These changes help prepare the body for the blood loss that might happen during childbirth.
The 5x Increased Risk Factor During Pregnancy
Pregnant women are five times more likely to get blood clots than women who are not pregnant. This is because the body changes how it clots blood to help prevent too much bleeding during delivery.
The growing uterus also puts pressure on veins, which can slow down blood flow. This is more common in the legs and pelvis.
How Pregnancy Changes Blood Clotting Mechanisms
Pregnancy makes the blood clotting system more likely to form clots. Some clotting factors increase, while others that prevent clots might decrease.
These changes help prevent too much bleeding during childbirth. But they also increase the risk of blood clots. Knowing about these changes is key to managing the risks of blood clots during pregnancy.
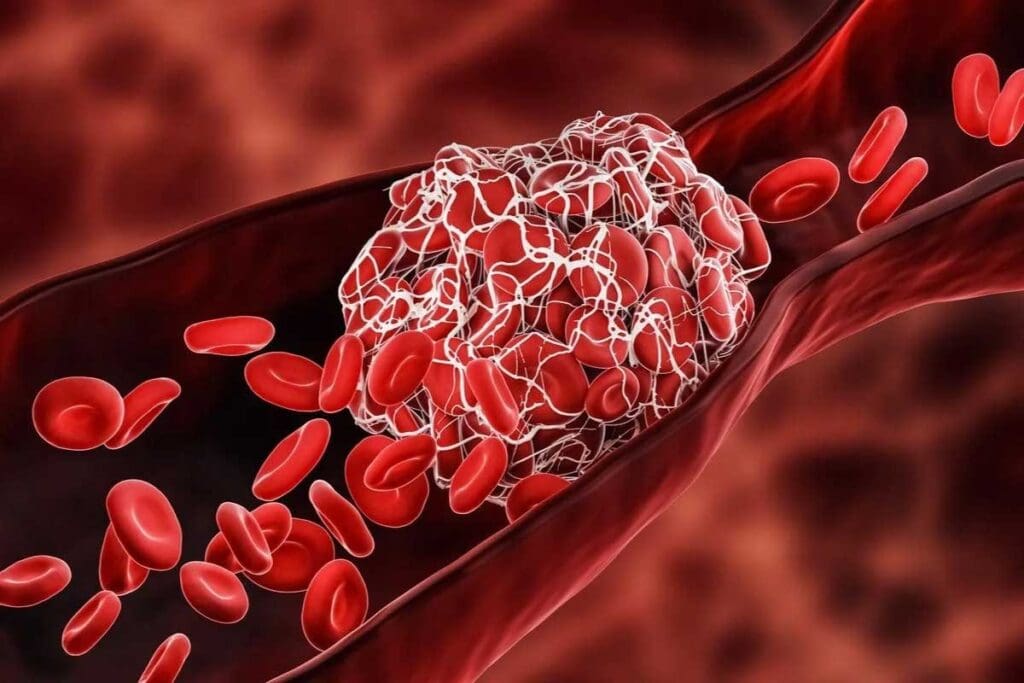
Types of Blood Clots That Can Develop in Pregnant Women
Pregnancy increases the risk of blood clots. Two main types are Deep Vein Thrombosis and Pulmonary Embolism. It’s important for pregnant women to know about these conditions. This way, they can get help quickly if needed.
Deep Vein Thrombosis: Clots in the Legs and Pelvis
Deep Vein Thrombosis (DVT) is a blood clot in the deep veins. It usually happens in the legs or pelvis. Signs and symptoms include swelling, pain, and warm, red skin.
It’s key to spot these signs early. DVT can cause serious problems if not treated.
Pulmonary Embolism: When Clots Travel to the Lungs
A Pulmonary Embolism (PE) happens when a clot goes to the lungs. It can block blood flow. This is a serious condition that needs quick medical help.
Symptoms of PE include sudden breath trouble, chest pain, and coughing up blood.
| Condition | Common Symptoms | Potential Complications |
| Deep Vein Thrombosis (DVT) | Swelling, pain, warm skin, redness | Pulmonary Embolism, post-thrombotic syndrome |
| Pulmonary Embolism (PE) | Shortness of breath, chest pain, coughing up blood | Respiratory failure, cardiac arrest |
Knowing about blood clots in pregnancy is important. Recognizing DVT and PE symptoms helps women get help fast. This can lower the risk of serious issues.
7 Warning Signs of Blood Clots While Pregnant You Shouldn’t Ignore
It’s important to know the signs of blood clots when you’re pregnant. Blood clots can be dangerous for pregnant women. Spotting the symptoms early is key for getting the right help.
Leg Symptoms: Pain, Swelling, Redness, and Warmth
Deep Vein Thrombosis (DVT) often shows up in the legs. Look out for:
- Pain or tenderness in the leg
- Swelling in one leg
- Redness or discoloration
- Warmth to the touch
Respiratory Symptoms: Shortness of Breath and Chest Pain
A blood clot in the lungs is called a Pulmonary Embolism (PE). Watch for:
- Sudden shortness of breath
- Chest pain that gets worse with deep breathing
- Rapid heart rate
These symptoms are serious and need quick medical care.
“The risk of venous thromboembolism is significantly increased during pregnancy and the postpartum period. Prompt recognition and treatment of deep vein thrombosis and pulmonary embolism are critical to prevent serious complications.”
Coughing Up Blood and Other Critical Warning Signs
In serious cases, a pulmonary embolism can lead to:
- Coughing up blood
- Lightheadedness or dizziness
- Collapse or loss of consciousness
These are emergencies. Call emergency services right away.
| Symptom | Possible Condition | Action Required |
| Leg pain, swelling | Deep Vein Thrombosis (DVT) | Seek medical attention |
| Shortness of breath, chest pain | Pulmonary Embolism (PE) | Immediate medical attention |
| Coughing up blood | Severe Pulmonary Embolism | Call emergency services |
Knowing these signs can help you act fast if you or someone you know is pregnant. Always talk to your healthcare provider if you’re worried about symptoms.
What Causes Blood Clots During Pregnancy and Who’s at Risk?
Many things can make pregnant women more likely to get blood clots. The body changes a lot during pregnancy, affecting how blood clots and moves.
Hormonal Changes and Their Impact on Clotting Factors
Hormonal shifts in pregnancy can change how blood clots. The rise in estrogen is key in this process.
Higher estrogen levels make blood more likely to clot. This helps prevent too much bleeding during childbirth. But it also raises the risk of harmful clots.
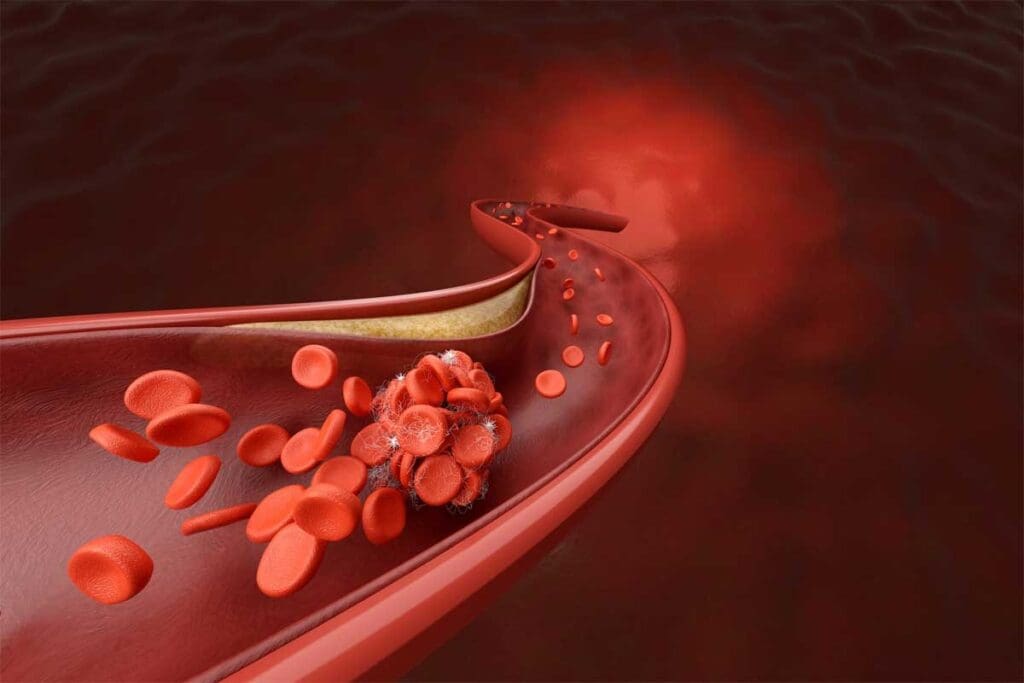
Physical Changes: How the Growing Uterus Affects Blood Flow
The growing uterus presses on veins in the pelvis, slowing blood flow in the legs. This reduced circulation can cause clots, mainly in the deep veins of the legs.
Also, the extra blood volume during pregnancy strains veins more. This increases the chance of clotting.
Genetic Predispositions and Pre-existing Conditions
Women with a family history of blood clots or certain genetic conditions are at higher risk. Conditions like Factor V Leiden greatly raise the risk of blood clots during pregnancy.
Pre-existing medical conditions, such as antiphospholipid syndrome, also increase clot risk.
Lifestyle Factors That Increase Blood Clot Risk
Lifestyle choices, like limited mobility and obesity, raise blood clot risk during pregnancy. Women who don’t move much, like during long trips or bed rest, are at higher risk.
Other factors, like smoking and having a cesarean section, also increase clot risk.
Blood Clots During Labor and Postpartum: Prevention and Treatment
It’s important to know about blood clot risks for new moms. Pregnancy can increase these risks due to body changes. But, these risks don’t stop after labor or delivery; they can even get worse.
Risks During Labor and Delivery
Labor and delivery are stressful and can lead to blood clots. The body’s strain and possible long labor can cause blood to slow down. This makes clotting more likely. Also, things like cesarean sections can raise the risk even more.
Healthcare providers need to watch patients closely during labor. This is true, even more so for those at higher risk, like those with a history of blood clots or genetic issues.
The Critical Postpartum Period
The time after giving birth is also risky for blood clots. The body changes a lot as it goes back to normal. The risk is highest in the first few weeks but stays a concern for weeks after.
Things that make postpartum blood clot risk higher include:
- Prolonged bed rest or immobility
- Recent surgery, such as a cesarean section
- History of blood clots or clotting disorders
- Obesity or other health conditions that may affect blood clotting
Treatment Options and Preventive Measures
Preventing blood clots during and after labor involves different strategies for each person. For some, anticoagulant meds might be used after birth to lower clot risk.
Other ways to prevent blood clots include:
- Early mobilization after delivery
- Use of compression stockings
- Adequate hydration
- Monitoring for signs and symptoms of blood clots
Women at higher risk might need closer monitoring or more treatments. It’s a team effort between healthcare and patients to ensure a safe recovery after birth.
Conclusion: Protecting Yourself from Pregnancy Blood Clots
It’s key for pregnant women to know about blood clot risks and signs. We’ve talked about how pregnancy ups the risk of blood clots. We’ve also covered the different types of clots and important warning signs.
Knowing the signs of a blood clot, like leg pain and swelling, is vital. It helps you get medical help fast. We stress the need to be careful, more so during labor and after giving birth. Knowing you can get blood clots and being aware of the signs can protect you and your baby.
By staying informed and proactive, you can lower your risk of blood clots during pregnancy. We urge pregnant women to talk to their healthcare provider about their risk. Following their advice on prevention and treatment is important for a healthy pregnancy.
FAQ
What are the signs and symptoms of blood clots during pregnancy?
Pregnant women might feel leg pain, swelling, and redness. They could also have shortness of breath and chest pain. Coughing up blood is another warning sign.
Why are pregnant women at a higher risk of developing blood clots?
Pregnancy raises the risk of blood clots due to hormonal and physical changes. The growing uterus can also affect blood flow, leading to clotting.
What is deep vein thrombosis (DVT) and how does it relate to pregnancy?
DVT is a blood clot in the deep veins, often in the legs and pelvis. Pregnant women are more at risk due to clotting factors and physical changes.
Can blood clots during pregnancy lead to complications?
Yes, blood clots can cause serious issues like pulmonary embolism (PE). This happens when a clot goes to the lungs. Quick medical help is key to avoid damage.
How can I reduce my risk of developing blood clots during pregnancy?
To lower your risk, stay healthy, drink plenty of water, and follow your doctor’s advice. This includes wearing compression stockings and taking anticoagulant medication.
Are there any specific risk factors that increase the likelihood of blood clots during pregnancy?
Yes, women with a history of blood clots or clotting disorders in their family are at higher risk. Being overweight or having twins also increases the risk.
What are the treatment options for blood clots during pregnancy?
Treatment usually involves medication to stop clotting. Sometimes, hospital care is needed to monitor and support the condition.
Can blood clots occur during labor and delivery?
Yes, the risk of blood clots is higher during labor and delivery. Doctors use precautions like compression stockings and medication to reduce this risk.
How can I protect myself from blood clots during the postpartum period?
Stay hydrated, move often, and follow your doctor’s postpartum care advice. Watch for signs of blood clots and seek help if you notice them.
Are there any long-term effects of having a blood clot during pregnancy?
Having a blood clot during pregnancy may raise your risk for future clots. Talk to your doctor about your individual risk factors.
References
- Higashi, Y., Kiuchi, T., & Furuta, K. (2010). Efficacy and safety profile of a topical methyl salicylate and menthol patch in adult patients with mild to moderate muscle strain. Clinical Therapeutics, 32(1), 34–43.
- Behm, D. G., Herat, N., Power, G. M. J., Brosky, J. A., Page, P., & Alizadeh, S. (2022). Menthol-based topical analgesic induces similar upper and lower body pain pressure threshold values: A randomized trial. Journal of Sport Rehabilitation, 31(1), 24–30.


































