Last Updated on November 17, 2025 by Ugurkan Demir

Different types of blood disorders can affect how the body produces and uses blood cells. These conditions influence the key parts and functions of the blood, including red blood cells, white blood cells, platelets, and plasma. Common examples include anemia and thrombocytopenia, while more serious ones include leukemia and lymphoma.
Because the different types of blood disorders impact various parts of the blood, they can cause a range of health problems — from mild fatigue to life-threatening complications. At Liv Hospital, we are dedicated to providing expert care for patients with both common and rare hematologic conditions.
It’s essential to understand the causes, symptoms, and treatments of the different types of blood disorders. With the right knowledge and medical support, patients can manage their condition effectively and improve their overall well-being.
Key Takeaways
- Common hematologic disorders include anemia and thrombocytopenia.
- Deadly blood diseases such as leukemia and disseminated intravascular coagulation require immediate medical attention.
- Blood cell disorders can affect various components of blood.
- Liv Hospital provides advanced care for blood disorders.
- Effective management of blood disorders requires understanding their causes, symptoms, diagnosis, and treatment options.
Understanding Blood and Its Components
Blood is key to our health, carrying oxygen and nutrients to our cells. It’s a complex fluid made of different parts, each with its own role. These roles are vital for our survival.
The Composition of Blood
Blood has four main parts: red blood cells, white blood cells, platelets, and plasma. Red blood cells carry oxygen to our tissues. White blood cells help fight infections. Platelets help stop bleeding when a blood vessel is hurt. Plasma carries these cells and nutrients, and it has proteins, nutrients, and hormones.
How Blood Functions in the Body
Blood does many things in our body. It brings oxygen and nutrients and takes away waste. The heart and circulatory system make sure blood moves around the body. This keeps our tissues and organs healthy.
When Blood Goes Wrong: Diseasemayo Development
Blood disorders happen when blood parts don’t work right. These can include anemia, leukemia, and hemophilia. Knowing how blood works helps us find and treat these problems. When blood problems occur, they can harm our health and quality of life.
Different Types of Blood Disorders: Classification and Overview

Blood disorders can be grouped by the blood part they affect. This helps us understand the different health issues they cause.
The main parts of blood are red cells, white cells, platelets, and plasma. Problems with each part can lead to different health issues.
Red Blood Cell Disorders
Red blood cell disorders affect the cells that carry oxygen. Anemia is when there are not enough red blood cells or they don’t have enough hemoglobin. Polycythemia vera is when the body makes too many red blood cells.
White Blood Cell Disorders
White blood cell disorders affect the immune system. Leukemia is a cancer that affects white blood cells. Lymphoma is cancer of the lymphatic system.
Platelet Disorders
Platelet disorders affect blood clotting. Thrombocytopenia is when there are not enough platelets. Thrombocytosis is when there are too many platelets.
Plasma Disorders
Plasma disorders affect the liquid part of blood. These include bleeding disorders like hemophilia and von Willebrand disease. These conditions make blood clotting difficult.
The table below shows the different blood disorders by the affected part:
| Blood Component | Disorder Examples | Key Characteristics |
| Red Blood Cells | Anemia, Polycythemia Vera | Oxygen transport issues, overproduction of red blood cells |
| White Blood Cells | Leukemia, Lymphoma | Immune system dysfunction, cancerous conditions |
| Platelets | Thrombocytopenia, Thrombocytosis | Bleeding or clotting issues due to abnormal platelet counts |
| Plasma | Hemophilia, Von Willebrand Disease | Bleeding disorders due to clotting factor deficiencies |
Knowing these categories and their conditions is key to diagnosing and treating blood disorders.
Anemia: The Most Common Blood Disorder Worldwide
Anemia is a health issue where the body doesn’t have enough red blood cells or hemoglobin. It’s a big problem worldwide. It can happen for many reasons, like not getting enough nutrients, having chronic diseases, or genetic issues.
Iron-Deficiency Anemia
Iron-deficiency anemia is the most common type. It happens when the body doesn’t have enough iron to make hemoglobin. This can be because of not eating enough iron, losing blood too much, or needing more iron when pregnant.
Vitamin Deficiency Anemia
Vitamin deficiency anemia is caused by not having enough vitamins like B12 or folate. These vitamins are key for making red blood cells. This anemia can come from not eating enough of these vitamins, not being able to absorb them, or certain health problems.
Symptoms and Treatment Options
Anemia symptoms can vary but often include fatigue, weakness, pale skin, and shortness of breath. Treatment depends on why it’s happening. It might involve changing what you eat, taking supplements, or fixing other health issues.
Treatment options for anemia vary widely. For iron-deficiency anemia, iron supplements are often used. For vitamin deficiency anemia, vitamin B12 injections might be needed.
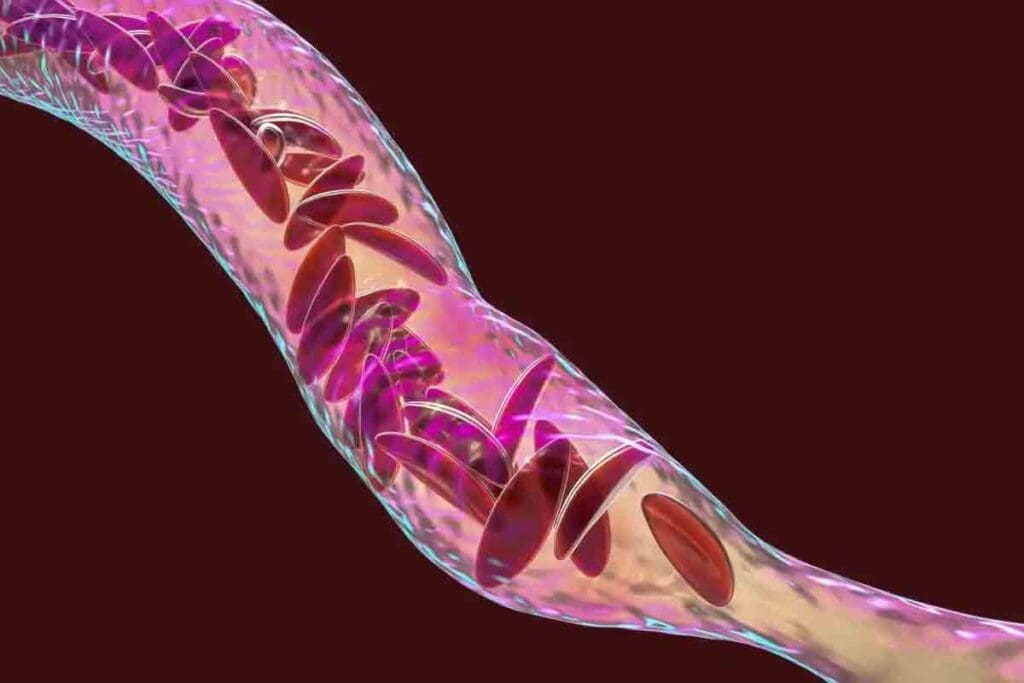
Sickle Cell Disease: A Potentially Fatal Genetic Blood Disorder
Millions worldwide suffer from Sickle Cell Disease, a genetic blood disorder with potentially fatal outcomes. This condition affects hemoglobin production. It makes red blood cells misshapen and prone to breaking down.
Causes and Inheritance Patterns
Sickle Cell Disease is caused by a mutation in the hemoglobin gene. It is inherited, passed down from parents to their offspring through genes. The disease shows up when someone inherits two abnormal hemoglobin genes, one from each parent.
The disease follows an autosomal recessive inheritance pattern. Carriers, who have one normal and one abnormal gene, usually don’t show all symptoms. But they can pass the abnormal gene to their children.
Complications and Life Expectancy
People with Sickle Cell Disease face many complications. These include pain crises, increased infection risk, and stroke. These issues can greatly impact their quality of life and life expectancy.
Thanks to medical progress, people with Sickle Cell Disease are living longer. Yet, the disease can be fatal, mainly in areas with poor healthcare access.
Current Treatment Approaches
Treatment for Sickle Cell Disease aims to manage symptoms and prevent complications. This includes managing pain during crises, blood transfusions to lower stroke risk, and medications to reduce pain crises.
New treatments, like gene therapy, are being researched to potentially cure the disease. These developments bring hope for better outcomes for those with Sickle Cell Disease.
Hemophilia: When Blood Fails to Clot
Hemophilia is a genetic disorder that makes it hard for blood to clot. This is a critical process to stop bleeding. People with hemophilia lack clotting factors, proteins needed for blood to coagulate. As a result, they may bleed for a long time, which can be dangerous if not treated right.
Types of Hemophilia
There are two main types of hemophilia: Hemophilia A and Hemophilia B. Hemophilia A is caused by a lack of factor VIII. Hemophilia B is due to a deficiency of factor IX. Both are genetic and mostly affect males, but females can carry the mutated gene.
The severity of hemophilia depends on the blood’s clotting factor level. Mild hemophilia has a factor level of 5% to 40% of normal. Moderate hemophilia has a level of 1% to 5%. Severe hemophilia has less than 1% of the normal factor level.
| Type of Hemophilia | Cause | Severity Levels |
| Hemophilia A | Deficiency in factor VIII | Mild, Moderate, Severe |
| Hemophilia B | Lack of factor IX | Mild, Moderate, Severe |
Global Prevalence and Inheritance
Hemophilia affects about 1 in 5,000 males worldwide. Hemophilia A is more common than Hemophilia B. It is inherited in an X-linked recessive pattern, meaning the genes are on the X chromosome.
“Hemophilia is a genetic disorder that is typically inherited from one’s parents, though spontaneous mutations can also happen.”
Female carriers have a 50% chance of passing the mutated gene to their sons, who will be affected, and to their daughters, who will likely become carriers.
Diagnosis and Management
Diagnosing hemophilia involves blood tests to check clotting factor levels. Treatment includes replacing the missing clotting factor in the blood to help it clot normally.
Prophylactic treatment is used to prevent bleeding, mainly in severe cases. This involves regular infusions of clotting factor concentrates. Gene therapy is also being explored as a future treatment for hemophilia.
Key management strategies include:
- Regular infusions of clotting factor concentrates
- Prophylactic treatment to prevent bleeding episodes
- Gene therapy as a future treatment
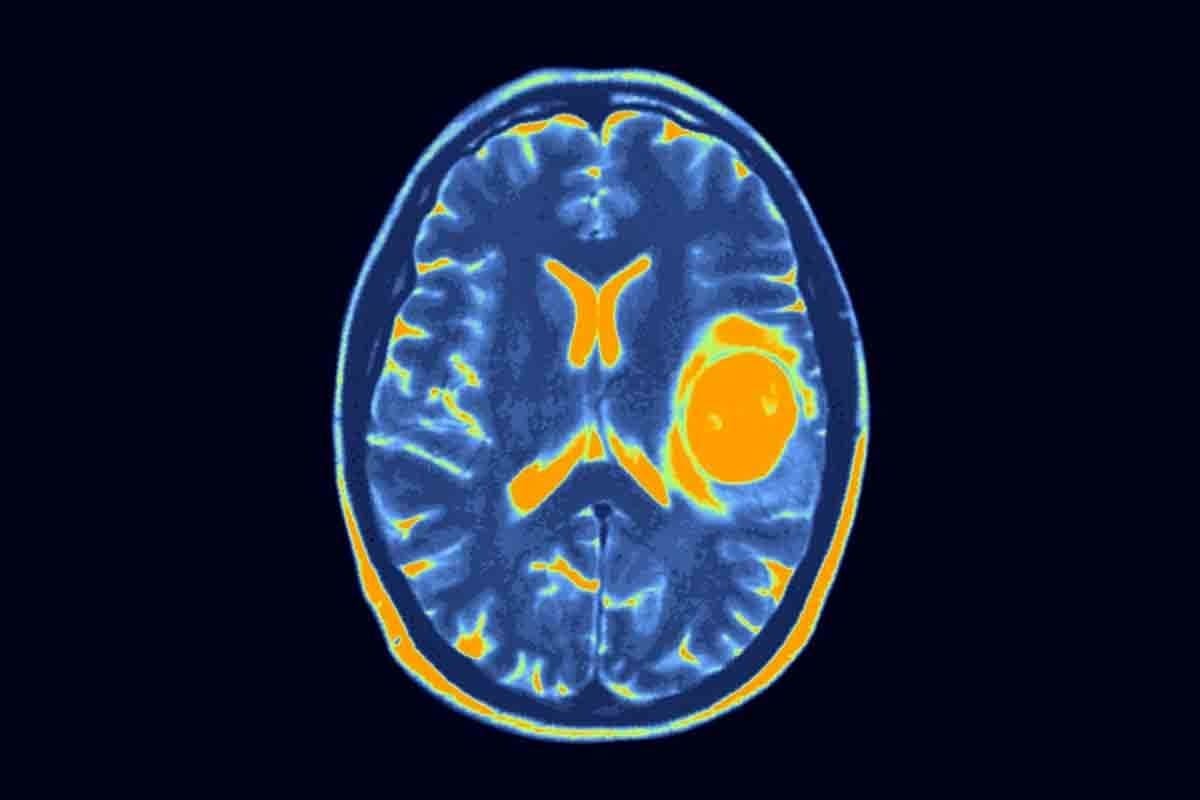
Leukemia: Cancer of the Blood Cells
Leukemia is a blood cancer that makes too many white blood cells. It happens in the bone marrow, where these cells are made. If not treated, it can cause serious health problems.
Leukemia can really affect the body. It messes up how blood cells are made. This can cause symptoms like tiredness, infections, and more serious issues.
Acute vs. Chronic Leukemia
Leukemia is divided into two types: acute and chronic. Acute leukemia makes lots of immature blood cells fast. This can cause serious health problems if not treated quickly.
Chronic leukemia grows slower. It takes longer for symptoms to show up. Knowing the type of leukemia helps doctors choose the right treatment.
Risk Factors and Warning Signs
There are several risk factors for leukemia. These include genes, certain chemicals, and radiation therapy. Spotting early signs like weight loss, infections, and easy bruising is key for early diagnosis.
- Genetic factors
- Exposure to certain chemicals
- Previous radiation therapy
Treatment Modalities and Survival Rates
Treatment for leukemia depends on the type and stage. Options include chemotherapy, targeted therapy, and sometimes bone marrow transplants. Thanks to new technology, more people are surviving leukemia.
It’s important to know the details of a patient’s leukemia for the best treatment. With new research and treatments, the future looks brighter for leukemia patients.
Lymphoma: Cancer of the Lymphatic System
Lymphoma is a serious cancer that affects the lymphatic system. It happens when lymphocytes, a key immune cell, grow abnormally. This cancer can show up in lymph nodes, spleen, and bone marrow.
Lymphoma is split into two main types: Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL). HL has Reed-Sternberg cells, while NHL does not. This difference helps doctors tell them apart.
Hodgkin vs. Non-Hodgkin Lymphoma
Hodgkin lymphoma is rare and moves slowly from one lymph node group to the next. It has Reed-Sternberg cells. Non-Hodgkin lymphoma is more common and can appear anywhere in the lymphatic system. It has many subtypes, each with its own aggressiveness and treatment response.
Treatment for HL and NHL is very different. HL usually responds well to treatment. But NHL’s treatment success depends on the subtype.
Staging and Prognosis
Staging lymphoma is key for planning treatment and predicting outcomes. The Ann Arbor Staging System divides lymphoma into four stages. Early stages are easier to treat, while advanced stages need stronger treatments.
Outcomes vary a lot based on the type of lymphoma, stage, and patient health. New diagnostic and treatment methods have greatly improved survival rates for many.
Modern Treatment Approaches
Today, lymphoma treatment includes targeted therapies, immunotherapies, and sometimes stem cell transplants. For HL, combined modality therapy with chemotherapy and radiation is common. NHL treatment varies based on the subtype and patient factors.
New treatments like CAR-T cell therapy are showing great promise. They offer hope for patients with hard-to-treat lymphoma.
In summary, lymphoma is a serious cancer but has seen big improvements in treatment. Knowing the differences between HL and NHL, the importance of staging, and modern treatments is key to better patient care.
Thrombocytopenia: When Platelet Counts Drop
Thrombocytopenia is a blood disorder that affects the production or survival of platelets. Platelets are key to preventing excessive bleeding. This condition can be caused by many things, like medication side effects or health issues.
Causes and Risk Factors
Many factors can lead to thrombocytopenia. Medications like heparin, certain antibiotics, and anti-inflammatory drugs can cause it. Autoimmune diseases like lupus or rheumatoid arthritis can also attack platelets.
Bone marrow disorders, where platelet production is affected, are another cause. Conditions like leukemia or lymphoma can also play a role. In some cases, it can be inherited, like congenital thrombocytopenia.
| Cause | Description | Risk Factor |
| Medications | Certain drugs can reduce platelet count. | Patients on heparin or certain antibiotics. |
| Autoimmune Diseases | The immune system attacks platelets. | Patients with lupus or rheumatoid arthritis. |
| Bone Marrow Disorders | Affects platelet production. | Patients with leukemia or lymphoma. |
Symptoms and Complications
The main symptom of thrombocytopenia is bleeding. This can range from mild bruising to severe hemorrhage. Other signs include petechiae (small spots on the skin), nosebleeds, and bleeding gums.
If not treated, thrombocytopenia can lead to serious problems. These include internal bleeding, which can be life-threatening. The severity of symptoms depends on the platelet count level.
Treatment Strategies
Treatment for thrombocytopenia varies based on the cause and severity. For mild cases, monitoring might be enough. If the cause is a medication, stopping it can help.
For more serious cases or those caused by underlying conditions, treatments are needed. These can include corticosteroids to increase platelet count. Or, intravenous immunoglobulin (IVIG) to reduce antibody production. In severe cases, platelet transfusions might be necessary.
Von Willebrand Disease: The Most Common Bleeding Disorder
Von Willebrand disease affects millions worldwide. It’s a genetic disorder that makes blood clotting hard. This leads to bleeding problems. Knowing about it helps manage it better and improve life quality.
Types and Severity Levels
Von Willebrand disease has different types based on how much von Willebrand factor (VWF) is missing. Type 1 is the most common and usually mild. Type 3 is the most severe.
How severe von Willebrand disease is can vary a lot. It depends on how much VWF is present and if there are any gene mutations.
| Type | Description | Severity |
| Type 1 | Partial deficiency of VWF | Mild |
| Type 2 | Qualitative defect in VWF | Moderate to Severe |
| Type 3 | Complete deficiency of VWF | Severe |
Diagnosis Challenges
Diagnosing von Willebrand disease can be tough. Symptoms can look like other bleeding disorders. Doctors need a detailed medical history, physical exam, and lab tests to check VWF levels and function.
“The diagnosis of von Willebrand disease requires a high index of suspicion and a thorough evaluation, including laboratory tests such as VWF antigen and activity assays.”
Treatment Options and Management
Managing von Willebrand disease depends on the type and how severe it is. Treatments include desmopressin, VWF replacement, and other measures to stop bleeding.
Good management also means teaching patients how to handle bleeding episodes. They learn how to prevent bleeding before surgeries or dental work.
Disseminated Intravascular Coagulation: A Life-Threatening Blood Disorder
When the body’s blood clotting goes wrong, it can cause disseminated intravascular coagulation. This is a serious condition. It leads to both widespread clotting and bleeding in the blood vessels.
Causes and Risk Factors
DIC can start from many things, like severe infections, trauma, cancer, and pregnancy problems. Knowing these risks helps find and treat it early.
- Severe infections (sepsis)
- Trauma or major surgery
- Cancer (particular leukemia)
- Complications during pregnancy (e.g., placental abruption)
Knowing what causes it helps manage it better.
Acute vs. Chronic DIC
DIC can be either acute or chronic. Acute DIC happens fast and is linked to severe problems. Chronic DIC grows slowly over time.
| Characteristics | Acute DIC | Chronic DIC |
| Onset | Rapid | Slow |
| Underlying Conditions | Severe infections, trauma | Cancer, chronic inflammation |
| Clinical Presentation | Severe bleeding, organ failure | Mild bleeding, often asymptomatic |
Emergency Treatment Approaches
Treating DIC means fixing the cause and managing symptoms. Emergency care might include replacing blood, using anticoagulants, and supportive care to avoid organ damage.
- Replacement therapy with platelets, fresh frozen plasma, or cryoprecipitate
- Anticoagulant therapy to prevent further clotting
- Supportive care to manage symptoms and prevent complications
Quick and effective treatment is key to managing DIC and better patient outcomes.
Conclusion: Advances in Blood Disorder Treatments and Future Outlook
Recent years have brought big changes in treating blood disorders. We now understand blood diseases better, leading to new treatments. These advancements have greatly improved survival rates and the quality of life for patients.
The future looks bright for blood disorder treatment. Research is ongoing in gene therapy, targeted treatments, and personalized medicine. These new methods aim to tackle the tough challenges of blood diseases, giving patients and their families new hope.
As medical science keeps growing, we can expect even more progress in treating blood diseases. The use of advanced technologies and teamwork among healthcare experts will be key. They will help us achieve better results for those dealing with blood disorders.
FAQ
What are the most common types of blood disorders?
Common blood disorders include anemia, leukemia, lymphoma, hemophilia, and thrombocytopenia. These conditions affect different parts of blood, like red and white cells, and platelets.
What is the difference between a blood disease and a blood disorder?
“Blood disease” and “blood disorder” are often used the same way. But, they can mean different things. A blood disease is a specific condition, like leukemia. A blood disorder is a broader term for many conditions that affect blood.
What are the symptoms of a blood disorder?
Symptoms vary by condition. Common ones are fatigue, weakness, and shortness of breath. Some disorders, like sickle cell disease, cause pain crises.
How are blood disorders diagnosed?
Doctors use tests like complete blood counts (CBCs) and blood smears to diagnose. Bone marrow biopsies and imaging tests like X-rays are also used.
What are the treatment options for blood disorders?
Treatment depends on the condition and its severity. Options include medications, transfusions, and bone marrow transplants. Some, like hemophilia, need ongoing replacement therapy.
Can blood disorders be cured?
Some can be cured, while others need ongoing management. For example, some leukemia and lymphoma can be cured. Hemophilia requires lifelong therapy.
What are the latest advancements in blood disorder treatments?
New treatments include gene therapy, targeted therapies, and immunotherapies. These have improved survival and quality of life for many patients.
What is disseminated intravascular coagulation (DIC)?
DIC is a serious blood disorder with abnormal clotting and bleeding. It can be caused by sepsis, trauma, and cancer.
What is von Willebrand disease?
Von Willebrand disease is a genetic disorder that affects bleeding. It leads to heavy menstrual bleeding and bruising.
What is polycythemia vera?
Polycythemia vera is a rare disorder with too many red blood cells. It increases the risk of blood clots and complications.
References
- Medical News Today. (2018). Blood disorders: Types, symptoms, and causes.