Last Updated on November 4, 2025 by mcelik

Did you know some medicines can raise your chance of getting tendonitis? Fluoroquinolone antibiotics, like ciprofloxacin, are known to increase this risk.
Tendonitis makes it hard to do everyday things because of tendon pain and swelling. It’s not just from physical strain or injury. Some drugs can also make it worse.
Knowing which medicines can lead to tendonitis is key. It helps doctors and patients make better choices about treatments.
Key Takeaways
- Certain antibiotics, like fluoroquinolones, are linked to an increased risk of tendonitis.
- Understanding drug-induced tendonitis can aid in prevention and management.
- Healthcare providers should consider the risk of tendonitis when prescribing certain medications.
- Patients should be aware of the possible side effects of their medicines.
- Alternative treatments may be considered to lessen the risk of tendonitis.
Understanding Medication-Induced Tendonitis

Medication-induced tendonitis is a big worry for both patients and doctors. Some drugs can make tendons inflamed. Tendons are the tissues that connect muscles to bones.
What is Tendonitis?
Tendonitis means tendons are inflamed. This leads to pain, stiffness, and less mobility. It can happen in any tendon but often affects the shoulders, elbows, wrists, hips, knees, and ankles.
The condition can really hurt a person’s quality of life. It makes it hard to do everyday things.
How Medications Can Affect Tendon Health
Some medicines can cause tendonitis by messing with how tendons work or by causing inflammation. For example, some antibiotics and corticosteroids can harm tendons. The exact ways they do this are not fully known. But it’s thought they might mess up the repair process of tendons.
Prevalence and Impact
The number of cases of medication-induced tendonitis depends on the drug and who takes it. But it’s a big worry because it can cause a lot of pain and disability. Knowing the risks and watching for early signs can help manage and maybe prevent it.
Medications Causing Tendonitis: An Overview

Some drugs can cause tendonitis, a condition that affects a person’s quality of life. It’s important to know which medications can harm tendons. This knowledge helps in preventing and treating tendonitis.
Common Drug Classes Associated with Tendon Damage
Several types of medications can lead to tendonitis. Fluoroquinolone antibiotics, like ciprofloxacin, are often linked to this condition. Corticosteroids, given orally or by injection, can also cause tendon damage. Statins and certain antidepressants have been found to increase the risk of tendonitis.
A study in the Journal of Clinical Rheumatology found a link between fluoroquinolone use and tendonitis. It noted, “Fluoroquinolone-induced tendinopathy is a serious adverse effect that can result in significant morbidity.”
“The risk factors for fluoroquinolone-induced tendinopathy include older age, concomitant corticosteroid use, and a history of tendon disorders.”
Severity Spectrum of Drug-Induced Tendinopathy
The severity of drug-induced tendinopathy varies. Some people might just feel mild pain, while others could face a complete tendon rupture. The severity depends on the drug’s dosage, treatment length, and individual risk factors.
Timeframe for Symptom Development
Symptoms of tendonitis can appear from a few days to weeks after starting a drug. In some cases, symptoms may show up months later. For example, fluoroquinolone-induced tendonitis often happens within the first month, sometimes as soon as 48 hours after the first dose.
Healthcare providers should closely watch patients on these medications, mainly during the first treatment period. Catching symptoms early can help prevent serious tendon damage.
Fluoroquinolone Antibiotics: The Primary Culprits
Fluoroquinolone antibiotics are good at fighting bacteria but can harm tendons. They are used to treat many infections. But, they can cause serious tendon problems.
Ciprofloxacin (Cipro)
Ciprofloxacin, or Cipro, is often given to people with infections. It works well against many bacteria. But, it can lead to tendonitis, mostly in older adults and those with tendon issues.
Levofloxacin (Leva)
Levofloxacin, or Leva, is used for infections like pneumonia and skin issues. It can also cause tendon damage. People over 60 are at a higher risk.
Moxifloxacin (Avelox)
Moxifloxacin, or Avelox, treats infections in the respiratory and skin areas. It’s effective but can also cause tendonitis. Doctors must think carefully before prescribing it.
FDA Black Box Warning
The FDA warns about fluoroquinolone antibiotics. They can cause serious tendon problems like tendonitis and rupture. Doctors must consider these risks when prescribing them, mainly for those at higher risk.
Corticosteroids and Tendon Damage
Corticosteroids help reduce inflammation but can harm tendons. They are used to treat many inflammatory conditions. But, their effect on tendons worries doctors and patients.
Oral Corticosteroids
Oral steroids like prednisone are used for their anti-inflammatory effects. But, they can increase the risk of tendonitis and rupture. The risk is higher in older adults and those with tendon problems.
“The use of oral corticosteroids can lead to a significant increase in the risk of tendon rupture, specially in weight-bearing tendons like the Achilles tendon.”
Injectable Corticosteroids
Injectable steroids, like cortisone, target inflamed areas. They are effective but can weaken tendons with repeated use. The risk of tendon damage depends on how often and how much is injected.
Mechanism of Tendon Weakening
Corticosteroids reduce collagen synthesis, which is key for tendon strength. This weakening increases the risk of tendonitis and rupture, more so with long-term or high-dose use.
| Corticosteroid Type | Common Use | Tendon Risk |
| Oral Corticosteroids (e.g., Prednisone) | Systemic inflammation | High risk with prolonged use |
| Injectable Corticosteroids (e.g., Cortisone) | Localized inflammation | Risk with repeated injections |
Dosage Considerations
The dosage and duration of corticosteroid treatment are key to avoid tendon damage. Doctors should weigh the benefits against the risks and look for alternatives when possible. It’s important to monitor for tendonitis signs and educate patients about the risks.
In conclusion, corticosteroids are good for inflammation but can harm tendons. It’s important to understand the risks of oral and injectable steroids. This way, doctors can better care for patients and reduce these risks.
Statins and Their Impact on Tendons
Statins are drugs used to manage high cholesterol. They might harm tendon health. Doctors worry about this because statins are common for heart disease prevention.
Common Statin Medications
Here are some well-known statins:
- Atorvastatin (Lipitor): Known for its effectiveness in lowering LDL cholesterol.
- Simvastatin (Zocor): Often prescribed for patients at risk of heart disease.
- Rosuvastatin (Crestor): Used to lower cholesterol and triglycerides.
- Pravastatin (Pravachol): Prescribed to reduce the risk of cardiovascular events.
Pathophysiology of Statin-Induced Tendinopathy
The exact way statins harm tendons is not clear. But, research shows they might damage tendon cells. This could be because statins affect cholesterol and coenzyme Q10 production, which are key for tendon health.
Risk Assessment for Statin Users
While tendon damage from statins is rare, some factors raise the risk. These include:
- Age: Older adults are more likely to have tendon issues.
- Pre-existing Tendon Conditions: Those with tendonitis or ruptures are at higher risk.
- Intensity of Statin Therapy: Taking higher doses of statins can increase tendon problems.
Doctors should weigh these risks when prescribing statins. They should also watch for any tendon damage signs in patients.
Antidepressants Associated with Tendonitis
Antidepressants are key for mental health, but some may harm tendons. The link between antidepressants and tendonitis is a big worry. We need to look closely at the drugs and how they affect tendons.
SSRIs and Tendon Health
SSRIs are a common type of antidepressant. Studies show they might raise the risk of tendonitis, mainly in older people. It’s not clear how, but SSRIs might mess with how tendons work.
Other Antidepressant Classes
Other antidepressants, like tricyclics and SNRIs, also link to tendon issues. The risk differs with each drug. This shows the importance of checking each person’s situation carefully.
Monitoring Guidelines
People on antidepressants, with a history of tendon problems or other risks, need regular checks. Doctors should teach patients about tendonitis signs like pain or swelling. They should tell patients to get help if they notice these symptoms.
Knowing the risks of antidepressant-related tendonitis is vital for doctors and patients. Being alert to signs and taking steps to prevent them can help. This way, people can enjoy the benefits of antidepressants while keeping their tendons safe.
Chemotherapy Drugs and Tendon Complications
Chemotherapy drugs and tendon damage are linked in oncology. These drugs are key in cancer treatment but can harm tendons.
Taxanes
Taxanes, like Paclitaxel (Taxol) and Docetaxel (Taxotere), treat many cancers. But they can also damage tendons, causing pain or even rupture.
Platinum Compounds
Platinum drugs, like Cisplatin and Oxaliplatin, are used for various cancers. They can lead to tendon issues, affecting health.
Vinca Alkaloids
Vinca alkaloids, including Vincristine and Vinblastine, are linked to tendon problems. They’re mainly for lymphomas and leukemias.
Balancing Cancer Treatment and Tendon Health
Healthcare providers face a challenge in treating cancer without harming tendons. Watching for tendon damage early and adjusting treatment can help.
| Chemotherapy Drug Class | Examples | Tendon-Related Risks |
| Taxanes | Paclitaxel (Taxol), Docetaxel (Taxotere) | Tendonitis, Tendon Rupture |
| Platinum Compounds | Cisplatin, Oxaliplatin | Tendon Damage, Tendonitis |
| Vinca Alkaloids | Vincristine, Vinblastine | Tendon Damage, Neuropathy |
It’s important for patients and doctors to know about tendon risks from chemotherapy. This knowledge helps in taking steps to avoid tendon problems.
Other Medications Linked to Tendonitis
Many medications can increase the risk of tendonitis, not just the well-known ones. Fluoroquinolone antibiotics and corticosteroids are often blamed for tendon damage. But other drugs can also harm tendons and need attention.
Diuretics
Diuretics help with high blood pressure and swelling. But they can also damage tendons. This happens because they change the balance of electrolytes in the body, affecting tendons.
Studies show that long-term diuretic use can lead to tendonitis. Knowing how medications affect tendons is important for keeping them healthy.
| Diuretic Type | Examples | Potential Tendon Risk |
| Loop Diuretics | Furosemide, Bumetanide | Electrolyte imbalance, dehydration |
| Thiazide Diuretics | Hydrochlorothiazide, Chlorthalidone | Less commonly associated, but long-term use can be risky |
Hormonal Medications
Hormonal drugs, like those in hormone replacement therapy and birth control, can affect tendons. The impact varies based on the hormone and the person’s health.
“Hormonal contraceptives can change tendon elasticity and strength, raising the risk of tendonitis.”
Retinoids
Retinoids, from vitamin A, treat skin issues like acne and psoriasis. They’re good for the skin but can harm muscles and tendons. The exact reason is not clear, but it might be related to how retinoids affect collagen and tendons.
Aromatase Inhibitors
Aromatase inhibitors treat certain breast cancers by lowering estrogen levels. This can weaken tendons and ligaments. People taking these drugs should watch for tendonitis signs and talk to their doctor.
In summary, many drugs can cause tendonitis, not just the well-known ones. Diuretics, hormonal drugs, retinoids, and aromatase inhibitors are among them. Being aware and monitoring is essential to prevent and manage tendon problems in patients on these medications.
The Paradox of NSAIDs and Tendon Health
NSAIDs and tendon health have a complex relationship. They offer short-term benefits but also carry long-term risks. NSAIDs, or Nonsteroidal Anti-Inflammatory Drugs, are used to manage pain and reduce inflammation. Yet, their effect on tendons is both beneficial and harmful.
Short-Term Benefits vs. Long-Term Risks
NSAIDs can quickly ease pain and inflammation. They are often used for acute injuries and conditions. But, long-term use can weaken tendons and increase the risk of rupture.
“The use of NSAIDs for extended periods can mask pain, potentially leading to overuse injuries,” notes a study published in a leading orthopedic journal. “This can create a vicious cycle where the tendon is subjected to continued stress without adequate recovery time.”
Specific NSAIDs of Concern
While all NSAIDs carry some risk, certain types are more linked to tendon problems. These include:
- Ibuprofen: Commonly found in over-the-counter medications like Advil and Motrin.
- Naproxen: Found in medications like Aleve.
- Diclofenac: Available in both oral and topical forms, including Voltaren.
It’s important to know the specific NSAID being used and its risks.
Appropriate Usage Guidelines
To reduce risks from NSAIDs and tendon health, follow these guidelines:
- Use NSAIDs only as directed and for the shortest duration necessary.
- Monitor tendon health and report any unusual pain or swelling to your healthcare provider.
- Consider alternative pain management strategies, such as physical therapy or corticosteroid injections, under the guidance of a healthcare professional.
Understanding the complex relationship between NSAIDs and tendon health helps make better pain management choices. This way, individuals can reduce risks.
Risk Factors for Drug-Induced Tendonitis
Several factors can increase the risk of drug-induced tendonitis. These include patient-specific and medication-related factors. Knowing these risks helps reduce the chance of tendon damage in patients taking certain medications.
Age-Related Sensitivity
Age is a big risk factor for drug-induced tendonitis. Older adults face a higher risk due to decreased tendon elasticity and more health issues. Studies show that fluoroquinolone use significantly raises the risk of tendon rupture in those over 60.
Pre-existing Tendon Conditions
Those with existing tendon problems, like tendinosis or tendonitis, are at greater risk. These conditions weaken tendons, making them more prone to damage from certain drugs.
Drug Interactions
Drug interactions can also increase the risk of tendonitis. Mixing certain drugs, like corticosteroids with fluoroquinolones, can greatly raise the risk of tendon damage. Healthcare providers must check for these interactions to avoid tendonitis.
Genetic Predisposition
Genetics can also play a role in the risk of drug-induced tendonitis. Some genetic variations can affect tendon health, making it more vulnerable to damage from specific medications.
The following table summarizes the key risk factors for drug-induced tendonitis:
| Risk Factor | Description | Impact on Tendon Health |
| Age-Related Sensitivity | Older adults are more susceptible due to decreased tendon elasticity. | Increased risk of tendon rupture |
| Pre-existing Tendon Conditions | Conditions like tendinosis compromise tendon integrity. | Higher risk of developing tendonitis |
| Drug Interactions | Combining certain medications increases the risk of tendon damage. | Significant increase in tendon damage risk |
| Genetic Predisposition | Genetic variations can affect tendon health. | Increased susceptibility to tendon damage |
Recognizing and Monitoring for Symptoms
Spotting the early signs of tendonitis is key to managing it well and avoiding more harm. Being alert to body changes, when taking drugs that can harm tendons, is very important.
Early Warning Signs
The first signs of tendonitis from drugs include pain, stiffness, and trouble moving the tendons. These signs can start slowly or come on fast, based on the drug and your body.
- Pain or tenderness, mainly when moving the affected joint
- Swelling or redness around the tendon
- A grating sensation when moving the tendon (crepitus)
- Weakness in the affected limb
Watching these signs closely is key. Catching it early can stop more serious tendon damage.
When to Contact a Healthcare Provider
If you notice any of these signs, reach out to your doctor right away. They can check how serious the symptoms are and tell you what to do next.
“Patients on medications associated with tendonitis should be aware of the risks and report any unusual symptoms to their healthcare provider without delay.”
| Symptom Severity | Recommended Action |
| Mild pain or stiffness | Monitor symptoms; consider alternative medications |
| Moderate to severe pain or swelling | Consult healthcare provider; potentially discontinue medication |
| Sudden severe pain or tendon rupture | Seek immediate medical attention |
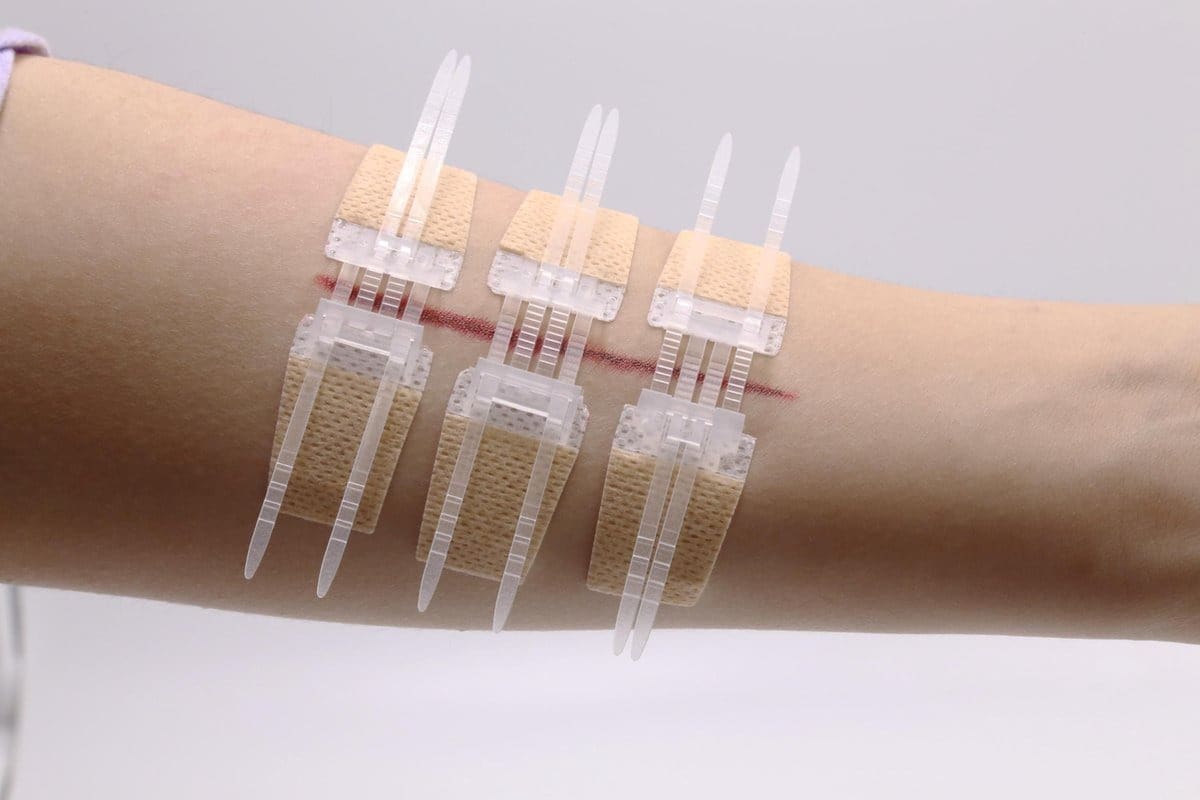
Diagnostic Approaches
Figuring out if tendonitis is caused by drugs usually involves a few steps. Doctors look at your symptoms, medical history, and might use:
- Ultrasound to see tendon damage
- MRI for detailed tendon and tissue images
- X-rays to check for other pain causes, like fractures
Getting the right diagnosis is vital. It helps create a treatment plan that balances the need for the drug against the risk of tendon harm.
Prevention and Alternative Treatment Options
Keeping tendons healthy is key. There are ways to prevent tendonitis and choose better treatments. If you must take certain medicines, there are steps to lower the risk.
Medication Alternatives for High-Risk Patients
If you’re at risk for tendonitis, looking at other medicines is wise. High-risk patients include older people, those with tendon issues before, and those on certain antibiotics or steroids. Talk to your doctor about safer options.
- For infections, pick antibiotics from other classes that are safer for tendons.
- For inflammation, try treatments like NSAIDs or biologic agents instead of steroids.
Preventive Measures During Necessary Treatment
Even if you must take medicines that might harm tendons, you can take steps to protect them. Regular stretching and strengthening helps keep tendons strong. Watch for tendonitis signs early and tell your doctor right away.
- Stay active to keep tendons flexible and strong.
- Avoid too much strain on your tendons.
- Keep a healthy weight to lessen tendon stress.
Nutritional Support for Tendon Health
Eating well is important for tendon health. Some nutrients are super helpful, like:
- Vitamin C: It’s key for making collagen.
- Omega-3 fatty acids: They help fight inflammation.
- Magnesium: It’s vital for muscle and tendon work.
Physical Therapy Approaches
Physical therapy is vital for tendonitis prevention and care. A physical therapist can create a workout plan to strengthen muscles and improve flexibility.
Important parts of physical therapy include:
- Eccentric strengthening exercises.
- Exercises for flexibility and range of motion.
- Correct warm-up and cool-down routines.
Conclusion: Balancing Medication Benefits and Tendon Health
It’s important to understand how medicines affect tendon health to avoid tendonitis. Certain drugs like fluoroquinolone antibiotics, corticosteroids, and some antidepressants can harm tendons.
Doctors need to consider both the good and bad sides of these medicines. For those at risk, steps like regular check-ups, eating right, and physical therapy can help. These actions can lower the chance of tendonitis.
Knowing the risks and taking action can help avoid tendonitis. It’s key for both doctors and patients to work together. This way, we can manage the risks of tendon damage from medicines.
FAQ
What medications are most commonly associated with tendonitis?
Medications like fluoroquinolone antibiotics, corticosteroids, and statins can cause tendonitis. Also, antidepressants, chemotherapy drugs, diuretics, hormonal medications, and NSAIDs are linked to it.
How do fluoroquinolone antibiotics cause tendonitis?
Fluoroquinolone antibiotics, like ciprofloxacin and levofloxacin, can harm tendons. They disrupt tendon function, leading to inflammation and damage.
What is the risk of tendonitis with corticosteroid use?
Corticosteroids can weaken tendons, increasing the risk of tendonitis. This risk grows with prolonged or high-dose use.
Can statins cause tendonitis?
Yes, statins like atorvastatin can cause tendonitis. They affect tendon function, and older adults are at higher risk.
How do antidepressants contribute to tendonitis?
Antidepressants, including SSRIs, can lead to tendonitis. They alter tendon function. Monitoring is key to reduce risk.
What is the impact of chemotherapy on tendon health?
Chemotherapy drugs can harm tendons. They disrupt tendon function. Balancing cancer treatment with tendon health is vital.
Can NSAIDs cause tendonitis?
Yes, NSAIDs like ibuprofen can cause tendonitis. They affect tendon function. Long-term or high-dose use increases risk.
What are the risk factors for drug-induced tendonitis?
Age, pre-existing tendon conditions, drug interactions, and genetic predisposition increase tendonitis risk.
How can tendonitis be prevented or minimized?
Preventive measures like stretching and nutrition can reduce tendonitis risk. Physical therapy and medication alternatives are also options for high-risk patients.
What are the early warning signs of tendonitis?
Pain, stiffness, and limited mobility are early signs of tendonitis. Seeking medical help is essential for timely diagnosis and treatment.
How is tendonitis diagnosed?
Imaging studies help identify tendon damage. They confirm tendonitis diagnosis.
References
- van der Linden, P. D., et al. (2002). Fluoroquinolones and Achilles tendon rupture. New England Journal of Medicine, 346, 440-445. https://pubmed.ncbi.nlm.nih.gov/11856798/