
Spotting the warning signs of a blood clot in your leg can be lifesaving. At LivHospital, we focus on your health and use the latest technology. Deep vein thrombosis (DVT) happens when a clot forms in a deep vein, often in the legs.
It’s important to recognize these symptoms early. We know how critical it is to spot these signs quickly. This way, we can help you get the care you need fast.
Would a blood clot cause pain? Yes, it can. Knowing how to tell if you have a blood clot is key to getting help right away. In this article, we’ll cover the seven main signs of a blood clot in the leg.
Key Takeaways
- Recognizing early symptoms of a blood clot can save lives.
- DVT occurs when a clot forms in a deep vein, commonly in the legs.
- Timely medical intervention is critical for treating blood clots.
- Understanding the warning signs can help you seek care quickly.
- LivHospital prioritizes patient well-being and state-of-the-art care.
Understanding Blood Clots in the Leg
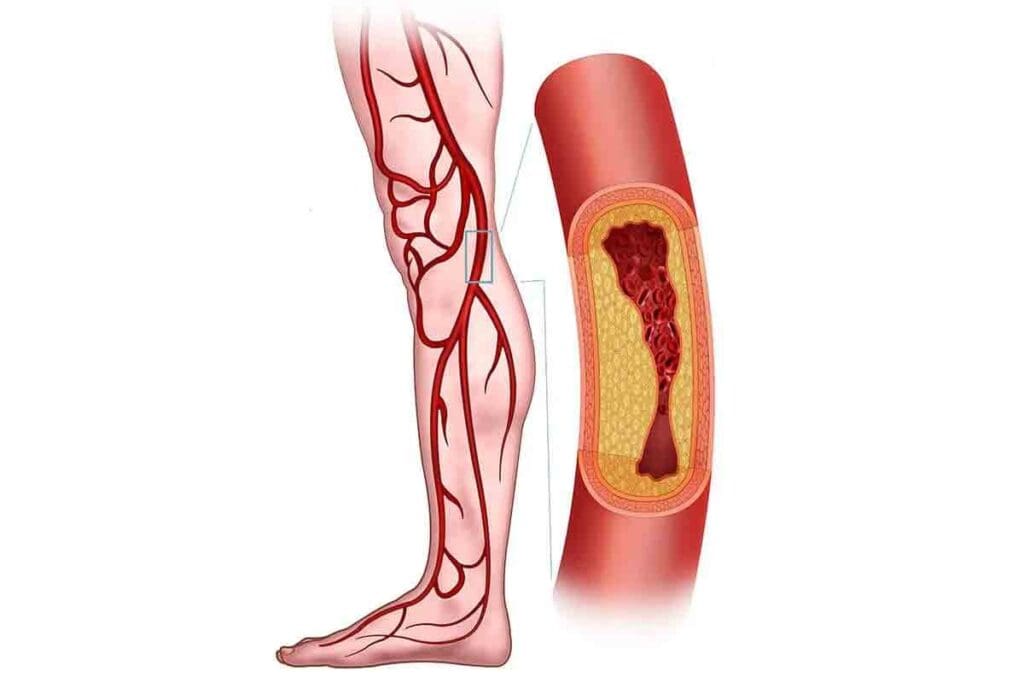
It’s important to know about blood clots in the leg. This knowledge helps spot warning signs early. It also means getting medical help fast. Blood clots in the leg are often linked to a condition called Deep Vein Thrombosis (DVT).
What is Deep Vein Thrombosis (DVT)?
Deep Vein Thrombosis (DVT) happens when a blood clot forms in deep veins. These veins are usually in the lower leg or thigh. This clot can block blood flow, leading to pain, swelling, and more.
The clot might break loose and travel through the blood. This can cause a pulmonary embolism, a serious and dangerous condition. Spotting DVT early is key to avoiding serious problems.
How Blood Clots Form
Blood clots form from several factors. These include:
- Immobility or long periods of bed rest
- Injury to a vein
- Genetic tendency to clot
- Certain medical conditions, like cancer or heart disease
When these factors meet, they can cause a blood clot in the deep veins of the leg.
Why Leg Clots Are Dangerous
Leg clots are dangerous because they can lead to serious and life-threatening issues. The biggest risk is the clot breaking loose and going to the lungs. This causes a pulmonary embolism.
Knowing the risks and symptoms is vital. It helps get medical help quickly. Early treatment can greatly improve outcomes for DVT patients.
The Importance of Early Detection

Spotting DVT signs early is key to managing and treating it well. Early detection can greatly improve patient outcomes. It also lowers the risk of serious complications.
Ignoring DVT can lead to severe and even life-threatening issues. A major risk is pulmonary embolism. This happens when a clot moves to the lungs, blocking blood flow.
Potential Complications of Untreated Clots
Untreated DVT can cause serious problems. These include:
- Pulmonary embolism
- Post-thrombotic syndrome
- Chronic venous insufficiency
Pulmonary embolism is very dangerous. It has a high death rate if not treated quickly. This shows why finding and treating DVT early is so important.
Pulmonary Embolism Risk
The risk of pulmonary embolism is a big worry for those with untreated DVT. If a clot breaks loose, it can travel to the lungs. There, it can cause a pulmonary embolism.
| Complication | Description | Risk Level |
| Pulmonary Embolism | A blockage of an artery in the lungs | High |
| Post-thrombotic Syndrome | Chronic pain, swelling, and skin discoloration | Moderate |
| Chronic Venous Insufficiency | Long-term damage to the veins | Moderate |
Knowing these risks shows how vital early detection and action are. By catching DVT early, doctors can start the right treatment. This helps avoid these serious problems.
Blood Clot in Leg Symptoms: The 7 Critical Warning Signs
Blood clots in the leg can show up in different ways. It’s important to know the signs early. Some people might have severe symptoms, while others might have mild or vague signs.
Overview of Symptom Patterns
There are seven key signs of a blood clot in the leg. Look out for swelling, pain or tenderness, and skin discoloration. Also, watch for warmth, visible veins, fatigue, and skin changes or ulcers.
| Symptom | Description |
| Swelling | One leg may become swollen due to the clot obstructing blood flow. |
| Pain or Tenderness | Aching or cramping pain in the affected leg, often starting in the calf. |
| Skin Discoloration | The skin may become red, purple, or blue due to inflammation and poor circulation. |
| Warmth | The affected area may feel warmer than the surrounding skin. |
| Visible Surface Veins | Veins near the surface of the skin may become more visible due to the clot. |
| Fatigue or Heaviness | A feeling of heaviness or fatigue in the affected leg. |
| Skin Changes or Ulcers | In severe cases, skin changes or ulcers may develop due to chronic clotting. |
Why Symptoms May Vary Between Individuals
Symptoms can differ a lot between people. This is because of the clot’s location, size, and the person’s health. A medical expert says,
“The presentation of deep vein thrombosis can be quite varied, making it essential to maintain a high index of suspicion in patients with risk factors.”
It’s key for both patients and doctors to understand these differences. This helps in spotting the signs early and starting the right treatment.
Warning Sign #1: Swelling in One Leg
Swelling in one leg can be a sign of a blood clot. This happens when the clot blocks blood flow. It’s different from swelling that affects both legs.
Why Swelling Occurs
When a blood clot blocks veins, fluid builds up. This causes swelling in the affected leg. You might feel pain or tenderness too.
Swelling from a blood clot usually happens on one side. So, if one leg is much bigger than the other, it could be a sign.
How to Measure and Monitor Leg Swelling
To track swelling, measure both legs at the same spot. Use a tape measure around the calf or ankle. Do this at the same time every day.
- Mark the spot where you measure to ensure consistency.
- Compare the measurements of both legs.
- Record your measurements to track any changes over time.
Watching for swelling and knowing why it happens can help spot blood clot signs early. If you see a lot of swelling in one leg, see a doctor right away.
Warning Sign #2: Pain or Tenderness
Leg pain from blood clots can show up in many ways. It’s key to know what to look for. Pain or tenderness in the leg can be a sign of a blood clot.
Characteristics of Blood Clot Pain
Pain from Deep Vein Thrombosis (DVT) often feels like a cramp or soreness in the calf. This pain can get worse over time. It might be constant or only happen when you stand or walk.
Some people might feel only a little discomfort, while others might have very bad pain. It’s important to remember that the pain can vary a lot.
“The pain from DVT can be tricky, as it might seem like muscle strain.” But if the pain keeps coming back and is only in one leg, think about a blood clot.
Differentiating from Other Types of Leg Pain
Telling if pain is from a blood clot or something else can be hard. For example, muscle strain or arthritis can cause similar pain. But DVT pain usually stays in one spot and might come with swelling or redness.
“It’s not just about the pain; it’s about the combination of symptoms that can indicate a serious condition like DVT.”
To figure out why your leg hurts, think about these things:
- Location: Is the pain just in one area, like the calf?
- Duration: Has the pain been there for a long time or getting worse?
- Associated symptoms: Are there other signs like swelling, redness, or warmth?
Knowing these details can help you tell if the pain is from a blood clot or something else.
Warning Sign #3: Skin Discoloration
Skin discoloration is a clear warning sign for blood clots. A blood clot in the leg can change the skin’s look. This might be an early sign of a serious issue.
Color Changes to Watch For
The skin over the clot may turn reddish or bluish. This is because blood is building up under the skin. Sometimes, the color change can get worse and spread out.
Location and Patterns of Discoloration
The spot and pattern of discoloration can tell us a lot. Clot-related discoloration usually happens in one leg. It might also come with swelling or warmth.
| Characteristic | Description |
| Color Change | Reddish or bluish hue |
| Location | Typically one leg, area around the clot |
| Pattern | Localized, may spread |
Knowing these signs can help catch problems early. If you see unusual skin discoloration, along with pain or swelling, see a doctor right away.
Warning Sign #4: Warmth in the Affected Area
Warmth in the affected area is a subtle but important sign of a blood clot in the leg. This happens because the clot causes inflammation. This inflammation makes the surrounding tissue warmer.
Why Temperature Changes Occur
A blood clot can cause inflammation in the leg. This inflammation is the body’s way of reacting to the clot. It leads to more blood flow to the area, making the skin warmer than usual.
The warmth is a natural response by the body to heal and protect the area.
How to Check for Warmth
To check for warmth, gently touch the affected area with the back of your hand. Compare it to the same area on the other leg. If the affected area feels warmer, it could be a sign of a blood clot.
It’s essential to be aware of any unusual temperature differences between the two legs.
When checking for warmth, make sure both legs are in similar conditions. For example, if you’ve been sitting with one leg crossed over the other, wait a few minutes before comparing. Consistency in checking can help identify any issues early on.
Warning Sign #5: Visible Surface Veins
Visible surface veins can be a sign of a blood clot in the leg. This is something to pay close attention to. A clot can change how veins look near the skin’s surface.
Changes in Vein Appearance
A blood clot can make veins more visible. They might look bigger, twisted, or different in color. The affected leg’s veins could be more noticeable than usual.
Look out for these signs:
- Veins that appear larger or more pronounced
- Veins with a twisted or tortuous appearance
- Discoloration around the veins, such as redness or a bluish tint
Distinguishing from Varicose Veins
It’s important to tell the difference between a blood clot and varicose veins. Both can change how veins look. Varicose veins are big, twisted, and usually in the legs. They can be uncomfortable but are not as dangerous as a blood clot.
To tell them apart, consider these points:
| Characteristics | Blood Clot-Related Changes | Varicose Veins |
| Appearance | Veins may become more visible or discolored due to the clot | Enlarged, twisted veins |
| Location | Can occur anywhere in the leg | Typically found in the lower legs |
| Symptoms | May be accompanied by pain, swelling, or warmth | Can cause discomfort, aching, or heaviness |
Warning Sign #6: Fatigue or Heaviness in the Leg
Feeling tired or heavy in the leg is a sign of a blood clot. It’s not always easy to spot, but it’s very important. We’ll look into why leg fatigue is a big deal and when it means trouble.
Understanding Leg Fatigue
Leg fatigue is when your leg feels tired or weak. It can happen all the time or after you’ve been active. A blood clot in a deep vein can block blood flow, causing this feeling.
It’s key to tell the difference between regular leg fatigue and the kind caused by a blood clot. Normal fatigue goes away with rest, but DVT fatigue gets worse over time.
When Heaviness Signals a Problem
Leg heaviness is a worry if it comes with other DVT signs or if it stops you from doing daily things. If your leg fatigue is constant or very bad, and you also have swelling, pain, or color changes, see a doctor right away.
“Early recognition of the signs of DVT, including less obvious symptoms like leg fatigue, is critical for timely intervention and prevention of complications.”
Knowing why your leg feels tired is important for what to do next. If it’s because of a blood clot, getting medical help quickly can make a big difference.
Warning Sign #7: Skin Changes and Ulcers
Skin changes and ulcers are signs of late-stage DVT that need quick medical help. As DVT gets worse, it can change the skin a lot, mainly in the leg.
Late-Stage Symptoms
In late stages, DVT can badly harm the skin because of poor blood flow. This can make the skin turn colors, get thicker, and form ulcers.
Characteristics of Late-Stage Skin Changes:
- Discoloration: The skin may turn red, purple, or brown because of blood buildup.
- Thickening: The skin can get thick and hard, a condition called lipodermatosclerosis.
- Ulcers: Open sores or ulcers can form, often around the ankle.
Chronic DVT Effects on Skin
Chronic DVT can cause lasting skin problems, like post-thrombotic syndrome (PTS). PTS can lead to ongoing pain, swelling, and skin changes, really affecting life quality.
| Symptoms | Description | Impact on Quality of Life |
| Skin Discoloration | Changes in skin color due to blood accumulation | Aesthetic concerns, possible social withdrawal |
| Skin Thickening | Hardening of the skin, possibly limiting movement | Discomfort, reduced mobility |
| Ulcers | Development of open sores, prone to infection | Pain, risk of infection, possible hospital stay |
It’s key to spot these late-stage signs to manage complications and better outcomes. If you or someone you know shows these symptoms, getting medical help fast is vital.
Risk Factors for Developing Blood Clots
It’s important to know the risk factors for blood clots to prevent and detect them early. Many things can raise your risk, like certain health conditions, lifestyle choices, and genetics.
Medical Conditions That Increase Risk
Some health conditions can greatly increase your risk of blood clots. These include:
- Cancer and its treatment
- Heart disease and heart failure
- Diabetes
- Inflammatory bowel disease
- Previous history of deep vein thrombosis (DVT) or pulmonary embolism (PE)
These conditions can mess with blood clotting and flow, making clots more likely.
Lifestyle Factors
Lifestyle choices also affect your risk of blood clots. Some of these include:
- Prolonged immobility, such as during long flights or bed rest
- Smoking
- Obesity
- Surgery or trauma
Changing these lifestyle choices can lower your risk of clotting.
Genetic Predisposition
Genetics can also play a part in blood clotting disorders. Some inherited conditions that raise the risk include:
- Factor V Leiden
- Prothrombin gene mutation
- Antithrombin deficiency
Knowing these risk factors helps us and healthcare providers take steps to prevent them.
| Risk Factor Category | Examples | Preventive Measures |
| Medical Conditions | Cancer, heart disease, diabetes | Manage underlying conditions, regular check-ups |
| Lifestyle Factors | Smoking, obesity, prolonged immobility | Quit smoking, maintain healthy weight, regular exercise |
| Genetic Predisposition | Factor V Leiden, prothrombin gene mutation | Genetic testing, anticoagulant therapy if necessary |
By understanding and tackling these risk factors, we can prevent blood clots and lower the risk of serious problems.
Diagnosis and Treatment Options
Addressing blood clots requires quick diagnosis and the right treatment. We know it’s a complex process. But with the right steps, patients get the care they need.
Diagnostic Approaches
Imaging tests are key in diagnosing blood clots. Ultrasound is often used because it’s non-invasive and works well for leg clots. Sometimes, venography or CT scans are needed to confirm the diagnosis or check the clot’s size.
Finding out what’s wrong is the first step to treating it. We look at medical history, physical exams, and tests to make sure we get it right.
Treatment Options and Medications
Treatment for blood clots usually means anticoagulant medications. These stop the clot from getting bigger and prevent new ones. Sometimes, thrombolytic therapy is used to break down the clot. The treatment depends on the clot’s size, location, and the patient’s health.
- Anticoagulant medications (e.g., warfarin, rivaroxaban)
- Thrombolytic therapy for severe cases
- Compression stockings to reduce swelling
In some cases, thrombectomy is needed to remove the clot. We choose the best treatment based on each patient’s needs.
Recovery Timeline and Expectations
How long it takes to recover from blood clots varies. It depends on the clot’s size and the patient’s health. Patients usually start feeling better in a few weeks. But, it can take months to fully recover.
- Initial treatment phase: 0-3 months
- Continued anticoagulation therapy: 3-6 months or longer
- Follow-up care to monitor clot resolution and prevent recurrence
It’s important to follow the treatment plan and go to follow-up appointments. This helps ensure a smooth recovery.
Prevention Strategies
We can lower the risk of blood clots by using certain prevention strategies. It’s just as important to prevent blood clots as it is to treat them. There are many effective ways to do this.
Lifestyle Changes to Reduce Risk
Making lifestyle changes can greatly help prevent blood clots. Regular physical activity is a key way to reduce risk. Exercise improves blood flow, which helps prevent clots.
It’s also important to maintain a healthy weight. Being overweight can strain your veins.
Another key change is to avoid prolonged periods of immobility. Whether you’re on a long flight or working at a desk, moving regularly is important. Simple actions like stretching or standing up can help a lot.
Preventive Measures During High-Risk Periods
Certain situations, like after surgery or during long travel, increase blood clot risk. Preventive measures during these times are key. Wearing compression stockings can improve blood flow and lower clot risk.
On long flights or car rides, staying hydrated and avoiding crossing your legs is wise. In some cases, healthcare providers may suggest anticoagulant medications for high-risk individuals.
Medications for Prevention
For some, medications are vital for prevention. Anticoagulants are often given to those at high risk. These medications thin the blood, preventing clots.
As
“Prevention is always better than cure, specially when it comes to blood clots.”
This is very true for those with clot history or certain medical conditions. It’s important to follow your healthcare provider’s advice on preventive medications.
By understanding and using these prevention strategies, we can greatly lower blood clot risk and its serious complications.
When to Seek Medical Help
Knowing when to get medical help is key to avoiding serious problems from blood clots. Some symptoms need quick attention. Knowing these signs can save lives.
Emergency Warning Signs
There are clear signs that mean you need to see a doctor right away. Look out for severe swelling in one leg, intense pain or tenderness, and trouble breathing or chest pain. Also, watch for skin discoloration or redness, and warmth or tenderness in the leg.
- Severe swelling in one leg
- Intense pain or tenderness in the leg
- Difficulty breathing or chest pain, which could indicate a pulmonary embolism
- Discoloration or redness of the skin
- Warmth or tenderness in the affected leg
These symptoms can signal a potentially life-threatening condition.
Making the Call: Doctor or Emergency Room?
Deciding whether to see your doctor or go to the emergency room can be tough. If you’re experiencing any emergency warning signs, go straight to the emergency room.
“Time is of the essence when dealing with possible blood clots. Don’t hesitate to seek help if you’re unsure.”
If you have milder symptoms but are worried, make an appointment with your doctor instead.
It’s always safer to be cautious with your health. If you’re unsure, getting medical help can give you peace of mind and might even save your life.
Conclusion: Taking Action Against Blood Clots
It’s key to know the warning signs and risk factors for blood clots in the leg. This helps catch them early and treat them right. Look out for swelling, pain, and skin color changes. If you see these, get medical help fast.
It’s vital to fight against blood clots by preventing them and knowing the risks. Making small changes in your life can help a lot. For example, exercising regularly and keeping a healthy weight can lower your risk.
There are ways to prevent and treat blood clots. Using medicines that stop blood clotting and wearing compression stockings can help. Taking action early can keep you healthy and avoid serious problems.
We want to help people know how to fight against blood clots. Being informed and watching out for signs can lower your risk. This way, you can get help quickly if you need it.
FAQ
What are the common symptoms of a blood clot in the leg?
Symptoms include swelling and pain or tenderness. You might also see skin discoloration and warmth. Other signs are visible surface veins, fatigue, and skin changes or ulcers.
How do you know if you have a blood clot in your leg?
Look out for swelling, pain, or skin discoloration. If you notice these signs, get medical help right away. A doctor will check you with a physical exam, ask about your health history, and use tests to confirm.
Can a blood clot cause pain?
Yes, a blood clot can make your leg hurt. The pain might be there all the time or get worse when you move.
What does a blood clot in the leg look like?
A blood clot can make the skin look red, blue, or purple. The area might also feel warm.
What are the risk factors for developing blood clots?
Risk factors include certain medical conditions and lifestyle choices. These include cancer, heart disease, long periods of sitting, or being bedridden. Genetics also play a role.
How are blood clots diagnosed?
Doctors use a physical exam, your health history, and tests like ultrasound or venography to diagnose blood clots.
What are the treatment options for blood clots?
Treatment options include medicines to prevent clotting, drugs to dissolve clots, and sometimes surgery.
How can I prevent blood clots?
Preventing blood clots involves lifestyle changes. This includes regular exercise, staying at a healthy weight, and taking preventive measures during high-risk times. Medicines can also help prevent blood clots.
When should I seek medical help for a suspected blood clot?
If you have severe pain, trouble breathing, or chest pain, get help right away. These are emergency signs.
Can blood clots be treated at home?
No, blood clots need medical care. While you can take some steps at home, treatment should always be under a doctor’s guidance.
Reference
- MedlinePlus. (2020). Blood Clots – Symptoms.https://medlineplus.gov/bloodclots.html



































