Last Updated on November 14, 2025 by mcelik

Did you know that by the time we reach our mid-30s, our bone density starts to go down? This natural drop can lead to health problems like osteoporosis and a higher chance of breaking bones.
As we get older, our bones change in ways that affect their strength. Knowing when and why bone health starts to decline is key to staying healthy. We’ll look into what affects bone regeneration age limit and how it impacts our health.
Key Takeaways
- Peak bone density is typically reached in the mid-30s.
- Bone health declines with age, increasing the risk of osteoporosis.
- Understanding bone regeneration is key for overall health.
- Lifestyle changes can help support bone health.
- Early intervention can reduce the risk of fractures.
The Fundamentals of Bone Biology
To understand how bones regenerate, we must first learn about bone biology. This includes its composition and the cells that make up bones. Bone biology is a complex field that studies bone structure and health.
Bone Composition and Structure
Bones are not just static; they are dynamic organs that constantly change. Their composition and structure are key to their function. Bones are mostly made of collagen, a protein that makes them flexible, and hydroxyapatite
The outer layer of bones is called compact bone, and the inner layer is cancellous bone. The compact bone is dense and strong, while the cancellous bone has spaces filled with marrow. Knowing this helps us understand how bones regenerate and adapt to needs.
Types of Bone Cells and Their Functions
Three main types of bone cells are involved in bone remodeling: osteoblasts, osteoclasts, and osteocytes. Osteoblasts form bone by producing a matrix that gets mineralized. Osteoclasts break down bone tissue. Osteocytes are mature osteoblasts that help regulate bone metabolism.
Osteoblasts and osteoclasts work together to keep bones healthy. Osteocytes sense mechanical stress and guide the bone remodeling process.
Understanding the Bone Remodeling Process
Bone remodeling is key to understanding how bones heal and change over time. It’s a complex process that involves many cell types working together. This ensures bones stay healthy and balanced.
The Four Phases of Bone Remodeling
The bone remodeling process has four main phases: activation, resorption, reversal, and formation. Each phase is vital for the process to work right.
- Activation: It starts with the activation of osteoclasts. These cells are in charge of breaking down bone.
- Resorption: In this phase, osteoclasts break down bone tissue. This releases minerals like calcium and phosphorus into the blood.
- Reversal: After resorption, a reversal phase happens. This is when the broken-down bone is replaced by a new bone matrix. It gets ready for new bone formation.
- Formation: Last, osteoblasts, the bone-making cells, create a new bone matrix. This matrix is then mineralized to form new bone tissue.
The Continuous Cycle of Bone Renewal
Bone remodeling is a never-ending cycle that keeps bone tissue fresh throughout our lives. It’s key for keeping bones healthy, fixing small fractures, and adjusting to changes in how we move.
This cycle is influenced by many things, like hormones, how much we move, and what we eat. Knowing these factors helps us see how bone remodeling keeps our skeletons strong.
- Hormones like parathyroid hormone and calcitonin play a big role. They control how osteoclasts and osteoblasts work.
- Exercise and physical activity can boost bone formation and make bones denser.
- Getting enough calcium and vitamin D is important for bone remodeling to happen well.
Bone Development Through Childhood and Adolescence
Bone development starts in the womb and goes through many stages until adulthood. Bones change a lot, influenced by genes, hormones, and the environment.
Prenatal and Infant Bone Formation
Bone formation starts before birth, with the first bone cells forming. By birth, most of the skeleton is there, but it’s mostly cartilage. As infant bone development goes on, this cartilage turns into bone.
“The prenatal period is key for bone development, setting the stage for future health,” say bone biology experts.
Childhood Growth Patterns
In childhood, bones keep growing and changing fast. This is when cartilage turns into bone, making the skeleton strong and healthy.
- Bones grow in length and density.
- The skeleton becomes more ossified.
- Growth patterns can be influenced by nutrition and lifestyle.
The Adolescent Growth Spurt
The adolescent growth spurt is a big time for bone growth. It’s when height and bone density increase quickly. Hormonal changes drive this growth, which is vital for reaching peak bone mass.
A renowned expert in bone health, says, “The adolescent growth spurt is a key time for bone development, setting the stage for long-term bone health.”
When Does Bone Growth Officially Stop?
Knowing when bone growth stops is key to understanding bone health. This process involves many cell types working together. It’s shaped by genetics, hormones, and the environment.
Closure of Growth Plates
Bone growth ends when growth plates close. These plates, or epiphyseal plates, are at the bone ends. They help bones grow longer. When they close, bone growth stops.
This usually happens in late teens or early twenties.
Differences Between Males and Females
Girls and boys grow at different rates. Girls often start puberty and stop growing earlier than boys. Girls usually stop growing at 14 to 15 years old. Boys keep growing until they are 16 to 17.
But, how long it takes can vary a lot. This depends on genetics and hormones.
| Gender | Typical Age Range for Growth Plate Closure | Average Age of Growth Cessation |
| Female | 14-15 years | 14.5 years |
| Male | 16-17 years | 16.5 years |
Peak Bone Mass: The Height of Bone Strength
Peak bone mass is the highest bone density an individual can reach. It’s key to keeping bones strong. Many things, like genes, diet, and lifestyle, affect how much bone mass you can have.
Defining Peak Bone Mass
Peak bone mass is the highest bone tissue amount reached by the early 30s. It’s a big factor in preventing osteoporosis and fractures. A higher peak bone mass means a lower risk of osteoporosis.
Typical Age Range for Achieving Peak Bone Mass
Most people reach peak bone mass in their late 20s to early 30s. But, it can differ due to genetics, diet, and exercise. Knowing how bones change with age helps keep them healthy.
Factors Influencing Maximum Bone Density
Many things affect how much bone density you can have, including:
- Genetics: Your genes play a big part in your bone mass.
- Nutrition: Eating enough calcium and vitamin D is vital for bones.
- Lifestyle: Exercise, like weight-bearing and resistance, helps bones stay strong.
- Hormonal Factors: Hormones like estrogen and testosterone are important for bones.
| Factor | Influence on Peak Bone Mass |
| Genetics | Determines your bone density limit |
| Nutrition | Good calcium and vitamin D intake is essential |
| Physical Activity | Exercises like weight-bearing and resistance boost bone density |
| Hormonal Factors | Estrogen and testosterone are key for bone health |
Knowing what affects peak bone mass helps you take care of your bones. Eat well, exercise, and avoid bad habits like smoking. This way, you can keep your bones strong.
Bone Regeneration Age Limit: Myth vs. Reality
The link between age and bone regeneration is complex. It’s key to keeping our bones healthy. As we age, our bones change, affecting their ability to heal.
Do Bones Ever Completely Stop Regenerating?
Bones keep regenerating throughout our lives, but the speed changes with age. It’s true that bone regeneration slows down with age. Yet, saying bones stop regenerating is not accurate.
Bone regeneration involves many cell types, like osteoblasts and osteoclasts. The speed of bone regeneration depends on hormones, lifestyle, and health.
The Changing Rate of Bone Turnover Across Lifespan
Bone turnover is fastest in kids and teens, then slows in adults. As we age, the balance between bone building and breaking down shifts. This leads to a decrease in bone density.
| Age Group | Bone Turnover Rate | Characteristics |
| Childhood/Adolescence | High | Rapid growth and development |
| Adulthood | Moderate | Stable bone density |
| Old Age | Low | Gradual bone loss |
Knowing these changes helps us find ways to keep bones healthy at all ages. We can’t stop aging, but we can support bone health. A balanced diet, exercise, and medical care are key.
By understanding bone regeneration and its age-related changes, we can tackle aging bone challenges. This helps us maintain the best bone health possible.
Bone Regeneration After Age 30
As we hit our thirties, our bones start to change. The rate at which our bones repair themselves slows down. This means our bone density starts to drop. Knowing about these changes helps us keep our bones strong.
Early Changes in Bone Metabolism
In our thirties, how our bones form and break down changes. Bone remodeling keeps happening, but it’s not as good as before. Bone loss can start in the mid-to-late thirties, mainly if you have a family history of osteoporosis or don’t exercise much.
The number of cells that build bones goes down. But, the cells that break bones down stay active. This imbalance can cause our bones to weaken.
What Science Reveals About Mid-Life Bone Health
Mid-life is key for bone health. What we eat, how we exercise, and our lifestyle affect our bones. Eating foods rich in calcium and vitamin D, and exercising regularly, can help keep bones strong.
Recent studies show it’s important to watch our bones in mid-life. Knowing how our bones change helps doctors give us better care. They can help stop bone loss and lower the chance of osteoporosis later on.
| Factor | Impact on Bone Health | Recommendations |
| Nutrition | A diet lacking calcium and vitamin D can accelerate bone loss. | Ensure adequate intake of calcium and vitamin D through diet and supplements. |
| Exercise | Regular weight-bearing exercise helps maintain bone density. | Engage in activities like walking, running, or weight training. |
| Lifestyle | Smoking and excessive alcohol consumption can negatively impact bone health. | Avoid smoking and limit alcohol intake. |
Understanding bone changes after 30 and taking action can help keep our bones strong. It’s important to work with doctors to create a plan for our bone health.
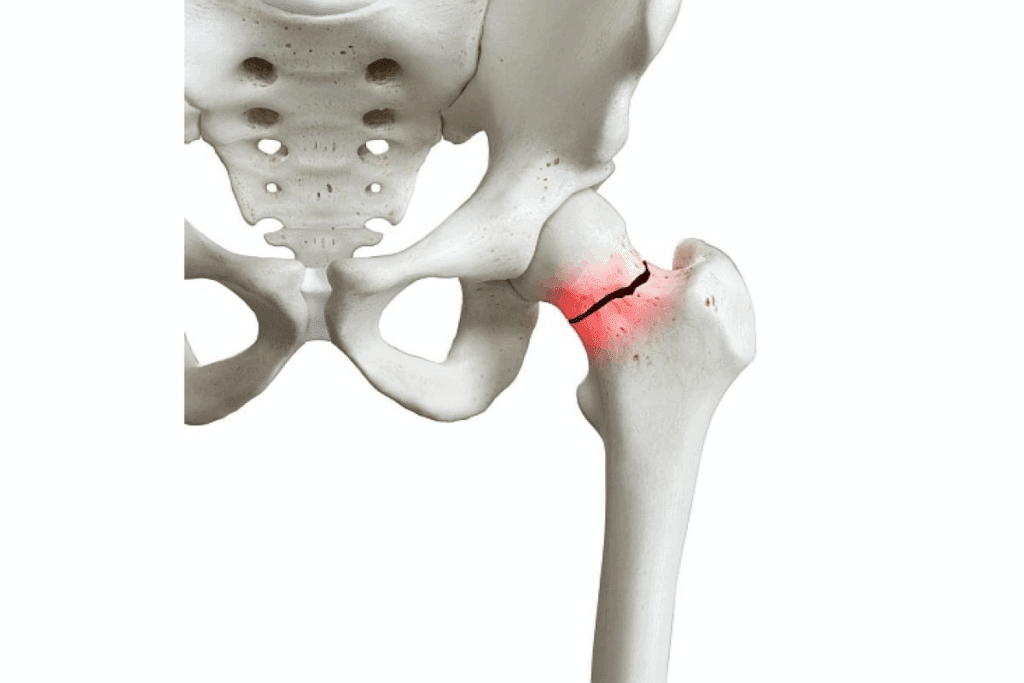
The Decline in Bone Healing Abilities
Aging makes it harder for bones to heal. This affects our health as we get older. Bones don’t repair as well after breaks.
Fracture Healing in Young vs. Older Adults
Young people heal bones faster than older adults. Younger bodies have more cells and a better blood supply. Older adults heal slower because of these changes.
Key differences in fracture healing between young and older adults include:
- Reduced cellular activity: Older adults have fewer cells available for bone repair.
- Decreased growth factor production: Growth factors essential for bone healing are produced at lower levels in older adults.
- Impaired blood supply: Aging can lead to reduced vascularity, affecting the delivery of nutrients and cells necessary for bone repair.
Cellular Changes That Slow Repair
Several cellular changes contribute to the decline in bone healing abilities with age. These include:
- Decline in osteoblast function: Osteoblasts are cells responsible for bone formation. Their activity decreases with age.
- Increased oxidative stress: Higher levels of oxidative stress can damage cells involved in bone healing.
- Accumulation of advanced glycosylation end-products (AGEs): AGEs can alter the structure and function of bone proteins, impairing bone repair.
Understanding these changes is key to helping older adults heal bones better. By focusing on the cellular and molecular reasons for slower healing, we can improve their quality of life.
Bone Remodeling After 50: What to Expect
After 50, our bodies change how they remake bones. This process is key to keeping bones strong. But, these changes can affect how well our bones stay healthy.
Hormonal Influences on Older Bone
Hormones play a big role in bone health after 50. Women see a drop in estrogen when they hit menopause. This can make bones lose mass faster. Men also see a drop in testosterone, which affects bone density.
These hormonal shifts can lead to more bone loss than gain. This is because they change how bones are broken down and built up.
Some key hormonal influences include:
- Estrogen decline in women: Leads to increased bone resorption and decreased bone formation.
- Testosterone decline in men: Contributes to reduced bone density and increased risk of osteoporosis.
- Changes in parathyroid hormone and vitamin D levels: Can affect calcium metabolism and bone health.
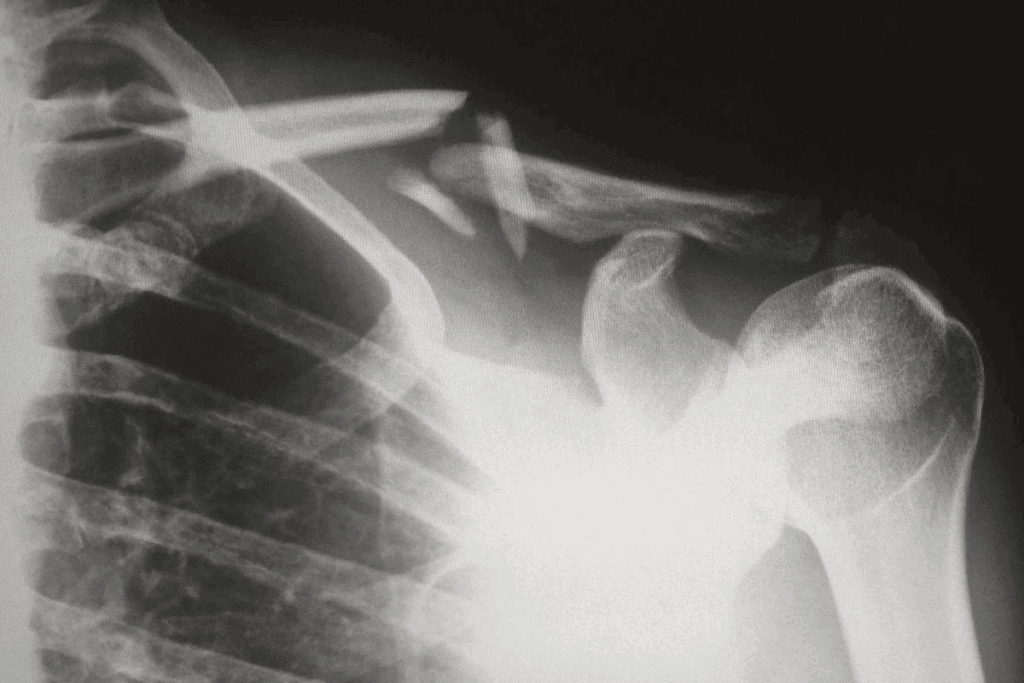
Common Bone Density Changes
Bones change a lot after 50. Trabecular bone, which is more active, loses density faster. This makes bones more likely to break, often in the spine, hips, and wrists.
Some common changes include:
- Loss of trabecular bone density: Increasing the risk of vertebral fractures.
- Cortical bone thinning: Leading to a higher risk of fractures in the hips and long bones.
- Changes in bone geometry: Affecting the overall strength and stability of the skeleton.
Knowing about these changes helps manage bone health after 50. By understanding how hormones and bones interact, we can take steps to keep our bones strong.
Factors That Accelerate Bone Regeneration Decline
Bone regeneration slows down with age. But, lifestyle and health factors can make it worse. As we get older, our bones change, losing density and strength. Certain factors can speed up this loss, harming our bone health.
Lifestyle Factors
Lifestyle choices greatly affect bone health. Smoking and excessive alcohol consumption hurt bone density. Smoking, in particular, reduces bone mass and raises fracture risk. A diet without calcium and vitamin D also weakens bones.
A sedentary lifestyle is another big factor. Regular exercise, like weight-bearing and resistance exercises, is key for strong bones. Without it, bones lose density and strength quickly.
Medical Conditions
Some medical conditions harm bone regeneration. Osteoporosis, a condition of weak bones, is a major concern. Other conditions, like hyperthyroidism and chronic kidney disease, affect bone health by changing calcium and vitamin D levels.
Hormonal changes, like those in women during menopause, cause rapid bone density loss. The drop in estrogen directly links to bone loss.
Medications That Impact Bone Health
Some medications harm bone health. Corticosteroids can cause bone loss with long-term use. Other drugs, like certain antidepressants and proton pump inhibitors, increase osteoporosis risk.
People on long-term medication should talk to their doctor about bone health. Monitoring bone density and adjusting lifestyle can help counteract these medications’ effects.
Osteoporosis and Compromised Bone Regeneration
Bone regeneration slows down as we age. Conditions like osteoporosis make it worse. Osteoporosis is a big worry for many, as it affects bone density and health.
The Connection Between Age and Osteoporosis Risk
Osteoporosis risk goes up with age. Hormonal changes, less activity, and bone density decline play a part. As we get older, bone loss happens faster than bone growth.
Key factors that contribute to the increased risk of osteoporosis with age include:
- Decreased levels of sex hormones, such as estrogen and testosterone
- Reduced calcium and vitamin D absorption
- Less physical activity or exercise
- Age-related changes in bone metabolism
| Age Group | Osteoporosis Risk Factors | Prevention Strategies |
| 50-60 years | Hormonal changes, reduced bone density | Calcium and vitamin D supplements, weight-bearing exercises |
| 60-70 years | Increased bone resorption, less physical activity | Resistance training, balance exercises, fall prevention |
| 70+ years | Significant bone loss, higher risk of fractures | Medication (if prescribed), lifestyle modifications, regular bone density monitoring |
Can Bone Regeneration Be Stimulated in Osteoporotic Patients?
Osteoporosis makes bone regeneration tough, but research shows ways to help. Lifestyle changes, supplements, and medical treatments can improve bone health. These methods aim to boost bone density and lower fracture risk.
Current approaches to stimulate bone regeneration in osteoporotic patients involve:
- Nutritional interventions, such as increased calcium and vitamin D intake
- Exercise programs tailored to improve bone health and muscle strength
- Pharmacological treatments, including bisphosphonates and other anti-resorptive agents
It’s key to understand how age, osteoporosis, and bone regeneration link. By tackling osteoporosis factors and finding ways to boost bone growth, we can improve life for those with this condition.
Maintaining Bone Strength After 40
Keeping bones strong after 40 is possible with the right mix of nutrition, exercise, and sometimes supplements or meds. As we get older, our bones change, which can make them weaker. But, with the right steps, we can help keep our bones healthy during this important time.
Nutrition for Aging Bones
Eating a balanced diet full of key nutrients is key for bone health. Calcium and Vitamin D are very important because they help keep bones strong and absorb nutrients. Other nutrients like protein, magnesium, and Vitamin K also play a big role.
Eating foods like dairy, leafy greens, nuts, and fish can help get these nutrients. Here’s a table showing how much of each nutrient you should aim for daily:
| Nutrient | Daily Recommendation |
| Calcium | 1,000 – 1,200 mg |
| Vitamin D | 600 – 800 IU |
| Protein | 0.8 – 1.0 g/kg body weight |
Exercise Protocols for Bone Health
Exercise is also vital for keeping bones strong. Weight-bearing and resistance exercises are best because they help bones grow and get denser. Some good exercises include:
- Brisk walking
- Jogging or running
- Weight training
- High-impact aerobics
Supplements and Medications
Sometimes, we might need supplements or medications to help our bones. Bisphosphonates are often used to treat osteoporosis by slowing bone loss. Other options include:
- Denosumab: a monoclonal antibody that targets bone resorption
- Teriparatide: a form of parathyroid hormone that stimulates bone formation
Always talk to a doctor before starting any new supplement or medication. They can make sure it’s right for you.
Medical Interventions for Late-Stage Bone Regeneration
For those with late-stage bone regeneration issues, medical help is key. As we get older, our bones don’t repair as well. This can lead to weaker bones and a higher chance of breaking them. Luckily, new medical discoveries offer hope for better bone health.
Current Treatments to Enhance Bone Formation
There are many ways to help bones in late-stage regeneration. These include:
- Pharmacological Interventions: Medicines like bisphosphonates and teriparatide help make bones stronger and less likely to break.
- Bone Grafting: This surgery uses healthy bone to help the damaged area heal.
- Stem Cell Therapy: This new research uses stem cells to help bones heal and grow.
How well these treatments work depends on many things. Your health, how bad your bone issues are, and more all play a part. Always talk to a doctor to find the best treatment for you.
Emerging Therapies and Research
New research is bringing us closer to better bone healing. Some promising new treatments include:
| Therapy | Description | Potential Benefits |
| Gene Therapy | Introduces genes that help bones grow into the body. | Could greatly improve bone healing. |
| Tissue Engineering | Creates new tissue from biomaterials and cells to fix or replace damaged bone. | Looks promising for fixing complex bone problems. |
| Low-Level Laser Therapy | A non-invasive treatment that uses lasers to help cells heal. | May help bones heal faster and reduce pain. |
These new therapies are exciting steps forward in bone healing. As research keeps growing, we’ll see even more innovative ways to help with late-stage bone regeneration.
Conclusion
It’s important to know about the bone regeneration age limit and how it affects bone health. This knowledge helps us keep our bones strong as we age. Bone regeneration changes a lot as we get older.
Bones are usually at their strongest in early adulthood. After that, they start to lose strength more slowly. By focusing on bone health, we can lower the risk of bone problems and stay healthy.
To keep bones healthy, we need to eat right, exercise regularly, and live a healthy lifestyle. Knowing what affects bone regeneration helps us make better choices for our bones. This includes our lifestyle and any health conditions we might have.
FAQ
At what age do bones stop growing?
Bone growth usually stops when the growth plates close. This happens at the end of adolescence or early adulthood.
What is peak bone mass, and when is it achieved?
Peak bone mass is the highest bone density an individual can reach. It usually happens in the late 20s to early 30s.
Do bones completely stop regenerating after a certain age?
Bones keep regenerating throughout life. But, the rate of bone turnover slows down after a certain age.
How does bone regeneration change after age 30?
After 30, small changes in bone metabolism start. These changes affect bone regeneration and lead to a gradual decrease in bone density.
What happens to bone healing abilities as we age?
The ability to heal bones after fractures gets worse with age. Older adults heal fractures slower than younger people.
How do hormonal changes after age 50 impact bone health?
Hormonal changes after 50 can greatly affect bone remodeling. This leads to changes in bone density.
What factors can accelerate the decline in bone regeneration?
Lifestyle choices, certain medical conditions, and medications can make bone regeneration decline faster.
Is it possible to stimulate bone regeneration in osteoporotic patients?
Yes, research shows that bone regeneration can be stimulated in osteoporotic patients through various treatments.
How can bone strength be maintained after age 40?
To keep bone strength after 40, a mix of good nutrition, exercise, and sometimes supplements or medications is needed.
What medical interventions are available for late-stage bone regeneration?
Treatments to boost bone formation are available. New therapies and research also offer hope for those with weak bones.
How does bone density decline with age?
Bone density goes down with age because bone regeneration slows and bone metabolism changes.
What is the role of osteoblasts, osteoclasts, and osteocytes in bone health?
Osteoblasts, osteoclasts, and osteocytes are key in bone remodeling. Osteoblasts make new bone, osteoclasts break down old bone, and osteocytes control bone metabolism.
Reference
- National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) – Bone Health and Regeneration
https://www.niams.nih.gov/health-topics/bone-health