Last Updated on November 26, 2025 by Bilal Hasdemir

At Liv Hospital, we know how complex Acute Lymphocytic Leukemia (ALL) is. It’s a fast-growing cancer that affects the blood and bone marrow. It’s the most common cancer in kids, making up about 25% of all cancers in children.
ALL is marked by the rapid growth of immature lymphocytes. This disrupts normal blood cell production. It mainly hits kids, but adults can get it too, and they often face tougher challenges. Knowing how ALL works is key to treating it well.
We offer top-notch healthcare and support for patients from around the world. Our team is here to give hope and clear answers during this tough time.
Key Takeaways
- Acute Lymphocytic Leukemia is a fast-growing cancer affecting the blood and bone marrow.
- It is the most prevalent cancer in children, representing about 25% of all pediatric cancers.
- ALL can also affect adults, often with worse prognoses.
- Understanding the unique characteristics of ALL is critical for effective treatment.
- Liv Hospital provides world-class healthcare with complete support for international patients.
Understanding Acute Lymphocytic Leukemia (ALL)

To understand Acute Lymphocytic Leukemia, we need to know its basics. It’s a cancer that affects the blood and bone marrow. It’s caused by the fast growth of immature white blood cells.
Definition and Basic Characteristics
Acute Lymphocytic Leukemia is a serious cancer that grows fast. It’s marked by the overproduction of lymphoblasts. These are young cells that can’t fight infections well.
This makes it hard for the bone marrow to make normal blood cells. It can happen in both kids and adults. Knowing the differences is key for the right treatment.
Terminology: Lymphocytic vs. Lymphoblastic
The terms “lymphocytic” and “lymphoblastic” are often used together. They describe the same disease. “Lymphocytic” talks about lymphocytes, a type of white blood cell. “Lymphoblastic” means these cells are immature, called lymphoblasts.
Both lymphocytic and lymphoblastic describe the same disease. They talk about the role of lymphoid cells in the disease. This double naming can be confusing, but it’s about the same leukemia.
The Biology of Acute Lymphocytic Leukemia

Acute Lymphocytic Leukemia (ALL) involves the growth of immature lymphocytes. These can be B-cell or T-cell types. Knowing the type of ALL is key because it affects treatment and outlook.
Cell Types Affected in ALL
ALL mainly affects lymphocytes, a key part of our immune system. Lymphocytes are split into B-cells and T-cells, each with its own role. In ALL, these cells grow out of control, filling the bone marrow and blood with cancer cells.
B-Cell vs. T-Cell ALL Subtypes
The type of ALL, B-cell or T-cell, depends on the lymphocyte type affected. B-cell ALL is more common in kids and usually has a better outlook. T-cell ALL often has more white blood cells and a higher risk of spreading to other areas, like the brain.
- B-cell ALL: More common in children, generally better prognosis.
- T-cell ALL: Often presents with higher WBC counts, higher risk of CNS involvement.
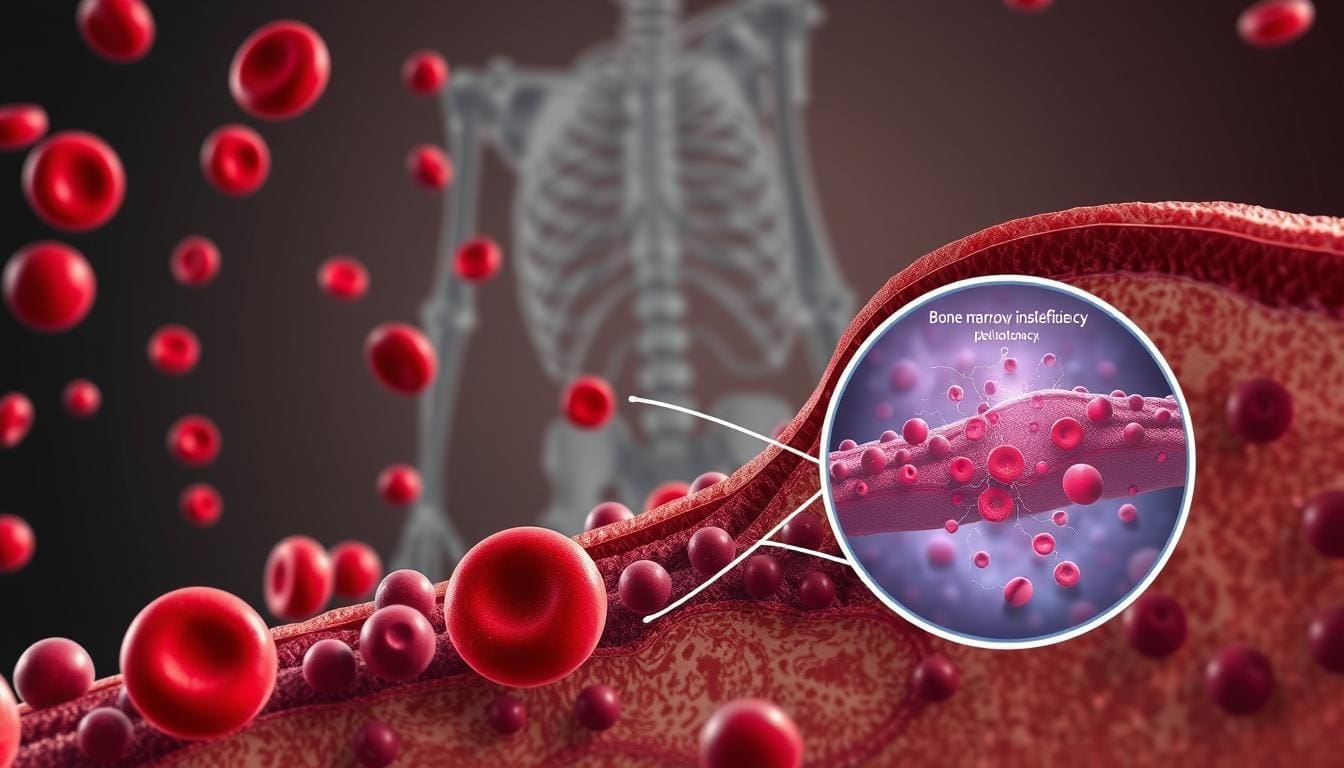
How Leukemic Cells Disrupt Normal Blood Production
Leukemic cells take over the bone marrow, pushing out normal cells. This makes it hard to make enough normal blood cells. Patients with ALL often have anemia, infections, and bleeding problems.
Understanding ALL’s biology is key to grasping its complexity and why certain treatments work. By looking at the cells involved and how they affect blood production, we can see why targeted therapies are so important.
Epidemiology of ALL
Understanding Acute Lymphocytic Leukemia (ALL) is key to finding risk factors and making public health plans. We look at how often ALL happens, who gets it, and where it’s most common. This helps us understand its effects.
Incidence Rates in Children vs. Adults
ALL mostly affects kids under 20. But it also happens in adults, mainly those over 50. The numbers show a peak in young children and another in older adults.
Demographic Patterns and Risk Groups
ALL’s occurrence changes among different ethnic and racial groups. In the U.S., Hispanic kids have a higher risk than non-Hispanic whites or blacks. Also, more boys than girls get it.
Genetic conditions like Down syndrome raise the risk. Exposure to certain radiation and chemicals also increases it.
Global Distribution
ALL’s spread varies worldwide. Richer countries often see more cases than poorer ones. This might be because of better testing in richer areas.
| Region | Incidence Rate (per million) |
|---|---|
| North America | 40-50 |
| Europe | 35-45 |
| Asia | 20-30 |
| Africa | 10-20 |
These patterns show we need more research on ALL’s causes. We also need specific health plans for different groups.
Causes and Risk Factors for Acute Lymphocytic Leukemia
The exact cause of ALL is not known. But, research has found several risk factors that can increase its chance. Knowing these risk factors is key for early detection and prevention.
Genetic Predispositions
Some genetic conditions raise the risk of getting ALL. For example, people with Down syndrome are at higher risk. Other genetic syndromes like Li-Fraumeni syndrome and ataxia-telangiectasia also increase the risk.
Genetic testing can spot these risks early. This allows for early monitoring and possible prevention.
Environmental Factors
Some environmental factors can also raise the risk of ALL. Ionizing radiation is a known risk. People exposed to high levels of radiation, like those working with radioactive materials, have a higher risk.
Also, exposure to certain chemicals, like benzene, has been linked to a higher risk of ALL.
Previous Cancer Treatments
Previous cancer treatments, like chemotherapy and radiation therapy, can increase the risk of secondary ALL. This is a big concern for cancer survivors.
For example, those who have had allogeneic stem cell transplant may face a higher risk due to the intense treatments.
Immune System Disorders
Some immune system disorders can also raise the risk of ALL. For instance, people with immunodeficiency diseases are more susceptible to ALL because their immune systems are weak.
In summary, while the exact cause of ALL is unknown, knowing the risk factors helps. These include genetic predispositions, environmental exposures, previous cancer treatments, and immune system disorders. This knowledge aids in early detection and can help in preventing the disease.
Signs and Symptoms of Acute Lymphocytic Leukemia
It’s important to know the signs of ALL to get help early. The first signs can be different for everyone. Doctors need to watch closely for these signs.
Common Initial Symptoms
The first signs of ALL can look like a cold or other minor illnesses. People might feel fatigue, fever, and get sick often. They might also notice easy bruising or bleeding, petechiae (small spots on the skin), and bone or joint pain.
Advanced Disease Manifestations
As ALL gets worse, symptoms can get much harder to handle. Signs can include significant weight loss, swollen lymph nodes, liver or spleen enlargement, and neurological symptoms like headaches or seizures.
Differences in Symptom Presentation Between Children and Adults
Children and adults with ALL show different symptoms. Kids often have more pronounced lymphadenopathy and hepatosplenomegaly. Adults might have more severe anemia and thrombocytopenia, leading to bleeding issues.
When to Seek Medical Attention
If you have symptoms that last or get worse, see a doctor. Early treatment can make a big difference. Look for help if you have unexplained fatigue, recurring infections, or unusual bleeding.
Diagnostic Process for ALL
To diagnose Acute Lymphocytic Leukemia (ALL), doctors use blood tests and bone marrow biopsies. These steps are key to finding the disease and planning treatment.
Blood Tests and Initial Findings
Blood tests are the first step in diagnosing ALL. They show if there are too many white blood cells, red blood cells, or platelets. But, more tests are needed to confirm the disease.
We use blood tests to:
- Check for abnormal white blood cell counts
- Evaluate red blood cell and platelet counts
- Identify any abnormal cells in the blood
Bone Marrow Biopsy and Aspiration
A bone marrow biopsy and aspiration are key for diagnosing ALL. They remove bone marrow for examination. Finding leukemic cells in the bone marrow confirms the diagnosis.
Bone marrow examination shows how far the disease has spread and its effect on blood cell production.
Cytogenetic and Molecular Testing
Cytogenetic and molecular testing find specific genetic changes in ALL. These tests help predict the disease’s course and guide treatment.
We use cytogenetic testing to:
- Identify chromosomal abnormalities
- Detect genetic mutations that may affect treatment
Imaging Studies
Imaging studies like X-rays, CT scans, or MRI scans check how far the disease has spread. They help see if other organs or systems are affected.
| Diagnostic Test | Purpose | Information Provided |
|---|---|---|
| Blood Tests | Initial screening for ALL | Abnormal cell counts, presence of leukemic cells |
| Bone Marrow Biopsy | Confirm diagnosis, assess disease extent | Presence of leukemic cells, impact on blood cell production |
| Cytogenetic Testing | Identify genetic abnormalities | Chromosomal abnormalities, prognostic information |
| Imaging Studies | Assess disease extent, identify complications | Involvement of other organs or systems |
Classification and Staging of Acute Lymphocytic Leukemia
Knowing how to classify and stage Acute Lymphocytic Leukemia (ALL) is key. It helps doctors predict how the disease will progress and choose the best treatment. The type of ALL a person has affects their treatment plan.
WHO Classification System
The World Health Organization (WHO) has a system to sort ALL into different types. It looks at the cell type and genetic traits. This system helps doctors understand the disease better and plan treatment.
Risk Stratification Approaches
Risk stratification is important in treating ALL. It helps doctors guess how likely a patient is to have a relapse. The National Cancer Institute (NCI) criteria are often used. They consider age, white blood cell count, and how well the patient responds to treatment. By knowing the risk, doctors can adjust treatment to fit the patient’s needs.
Prognostic Factors
Many things can affect how well a patient with ALL will do. These include age, white blood cell count, genetic traits, and how well the patient responds to treatment. For example, some genetic changes, like the Philadelphia chromosome, change the outlook. Knowing these factors helps doctors make better treatment plans.
“The presence of minimal residual disease (MRD) after initial treatment is a powerful prognostic indicator in ALL, with MRD-positive patients having a higher risk of relapse.”
Genetic Markers and Their Significance
Genetic markers are very important in ALL. Some genetic changes, like the BCR-ABL1 gene, affect how the disease is treated. Identifying these markers helps doctors choose the right treatments and check how well they’re working.
In summary, classifying and staging ALL is a detailed process. It involves looking at many things like WHO classification, risk stratification, prognostic factors, and genetic markers. By understanding these, doctors can give patients with ALL the best care possible.
How ALL Differs from Other Acute Leukemias
Acute Lymphocytic Leukemia (ALL) is different from other acute leukemias like Acute Myeloid Leukemia (AML) and Acute Promyelocytic Leukemia (APL). These differences are key for correct diagnosis and treatment.
ALL vs. Acute Myeloid Leukemia (AML)
ALL and AML are both aggressive leukemias but affect different cells. ALL targets lymphoid cells, while AML affects myeloid cells. This cell difference affects how the disease presents and how it’s treated.
For example, AML is more aggressive and common in adults. ALL, on the other hand, is more common in children. We’ll explore chemotherapy for leukemia later, but it’s important to note that treatment varies between ALL and AML.
ALL vs. Acute Promyelocytic Leukemia (APL)
APL is a subtype of AML with abnormal promyelocytes. Its treatment is different from ALL. APL is treated with all-trans retinoic acid (ATRA) and arsenic trioxide, not used in ALL.
Knowing the difference between ALL and APL is critical. APL needs specific treatments not used in ALL.
Differences in Cell Origin and Presentation
ALL comes from lymphoid progenitor cells, which grow into lymphocytes. AML and APL come from myeloid progenitor cells. This cell origin affects symptoms and clinical findings.
For example, ALL often shows lymphadenopathy and hepatosplenomegaly. AML and APL may show symptoms like anemia and thrombocytopenia due to bone marrow failure.
Variations in Treatment Approaches
ALL treatment mainly uses chemotherapy, with phases for induction, consolidation, and maintenance. AML and APL treatments include chemotherapy, targeted therapy, and sometimes stem cell transplantation.
The treatment choice depends on the leukemia’s genetic and molecular characteristics. Understanding these differences is key for the right treatment strategy.
Treatment Approaches for ALL
Acute Lymphocytic Leukemia (ALL) treatment combines old and new methods. We’ve made big strides in understanding the disease. This has led to better treatment plans.
Chemotherapy Protocols
Chemotherapy is key in fighting ALL. It uses drugs to kill cancer cells. We give chemotherapy in three parts: induction, consolidation, and maintenance.
The goal of the first part is to get the patient into remission. The next two parts aim to get rid of any cancer cells left.
Key Chemotherapy Agents:
- Vincristine
- Prednisone
- Doxorubicin
- Asparaginase
Targeted Therapies
Targeted therapies are a big part of ALL treatment now. They focus on specific molecules that help cancer cells grow. These therapies work with chemotherapy to make it more effective.
Examples of Targeted Therapies:
- TKI (Tyrosine Kinase Inhibitors) for Philadelphia chromosome-positive ALL
- Monoclonal antibodies targeting CD19 or CD22
Stem Cell Transplantation
Stem cell transplantation can cure ALL in some cases. It’s used for high-risk patients or those who have had a relapse. We use stem cells from a donor or the patient to replace bad marrow with good.
| Type of Transplant | Donor Source | Indications |
|---|---|---|
| Allogenic | Matched related or unrelated donor | High-risk ALL, Relapsed ALL |
| Autologous | Patient’s own cells | Selected cases, often in clinical trials |
Immunotherapy Options
Immunotherapy is a new hope in fighting ALL. It uses the immune system to attack cancer. CAR-T cell therapy is a big step forward, making T cells attack cancer cells.
We keep working to improve ALL treatment. Our goal is to give the best care to our patients.
Childhood vs. Adult ALL: Key Differences
Acute Lymphocytic Leukemia (ALL) shows different signs in kids and adults. This affects how they are treated and their chances of getting better. We’ll look at how ALL is different in each age group and how it changes care for patients.
Treatment Protocols
Children and adults with ALL get different treatments. Children usually get stronger chemotherapy to help them get better more often. Adults often get milder treatments because they face more risks from strong medicines.
For example, kids get more asparaginase and better protection for their brains. Adults get treatments that are less harsh but are getting better with new medicines.
Response Rates
How well treatments work also varies by age. Kids often get better very quickly, with success rates over 90%. Adults usually see success rates between 70% and 85%.
There are many reasons for these differences. These include how the leukemia works, health problems, and how well the body can handle strong medicines.
Long-term Outcomes
Long-term results for ALL patients also differ by age. Kids have a much better chance of being cured, with survival rates over 80% in many cases. Adults face a tougher road, with survival rates between 30% and 50%.
These differences come from how well kids and adults can handle strong treatments, health issues, and the type of leukemia they have.
Unique Challenges in Each Age Group
Both kids and adults with ALL face special challenges. Kids might grow slower or have a higher risk of getting other cancers because of strong treatments. Adults may have health problems that make treatment harder and increase the risk of side effects.
It’s important to know these age-specific challenges. This helps in creating better care plans and improving how well patients do overall.
Prognosis and Survival Rates for Acute Lymphocytic Leukemia
Knowing about the prognosis and survival rates for Acute Lymphocytic Leukemia (ALL) is key for patients and their families. Prognosis is about the disease’s likely outcome. It depends on several important factors.
Factors Affecting Prognosis
Many things can affect ALL’s prognosis. These include the patient’s age, how well they respond to treatment, and the leukemia’s genetic makeup. Age is a big factor, with kids usually doing better than adults. Certain genetic traits, like the Philadelphia chromosome, can also change the outlook.
Patients who do well at first tend to have a better chance. Early response to treatment is a good sign. It means the disease might be easier to control.
| Factor | Impact on Prognosis |
|---|---|
| Age | Children have better prognosis than adults |
| Response to Treatment | Early response is a positive indicator |
| Genetic Characteristics | Presence of Philadelphia chromosome can worsen prognosis |
Five-Year Survival Statistics
Survival rates for ALL have gone up, thanks to better treatments. Kids with ALL now have a five-year survival rate over 90%. Adults have a rate between 40% and 50%.
Pediatric vs. Adult Outcomes
Kids and adults with ALL face different challenges. Kids usually do better because they respond better to treatment and have fewer health problems. Adults often have more health issues and face tougher treatment.
Managing Relapse
Dealing with relapse in ALL needs a detailed plan. This includes using specific treatments and sometimes stem cell transplants. Watching for relapse signs is key. Early detection can lead to better results. We help patients create a plan to manage relapse effectively.
By knowing what affects prognosis and keeping up with new treatments, patients with ALL can improve their chances. This helps them better manage their disease.
Conclusion
Acute Lymphocytic Leukemia (ALL) is a complex disease. It needs a deep understanding of its biology, diagnosis, and treatment. We’ve looked at the main points of ALL, like its differences from other leukemias, how it’s diagnosed, and the treatments available.
New treatments have made a big difference for many patients. Targeted therapies and immunotherapy are showing great promise. We’ve also seen how ALL affects different age groups, with unique challenges and responses in children and adults.
As we wrap up our look at ALL, it’s clear more research and awareness are needed. We aim to summarize what we know and the treatment options. Our goal is to help patients, families, and healthcare workers in their fight against this disease.
FAQ
What is Acute Lymphocytic Leukemia (ALL)?
Acute Lymphocytic Leukemia (ALL) is a blood cancer. It happens when the bone marrow makes too many immature white blood cells, called lymphoblasts.
What is the difference between lymphocytic and lymphoblastic leukemia?
“Lymphocytic” and “lymphoblastic” both mean the same thing in ALL. “Lymphoblastic” talks about the cells being immature. “Lymphocytic” refers to the type of cell. They both describe the same condition.
What are the symptoms of Acute Lymphocytic Leukemia?
Symptoms of ALL include feeling very tired, looking pale, and getting sick often. You might also bruise easily, have swollen lymph nodes, or pain in bones or joints.
How is Acute Lymphocytic Leukemia diagnosed?
Doctors use blood tests, bone marrow biopsies, and special tests to find and study leukemic cells. This helps confirm the diagnosis.
What are the treatment options for Acute Lymphocytic Leukemia?
Treatments for ALL include chemotherapy, targeted therapy, and sometimes stem cell transplants. The choice depends on the patient’s risk and how well they respond to treatment.
How does Acute Lymphocytic Leukemia differ from Acute Myeloid Leukemia (AML)?
ALL and AML affect different blood cells. ALL targets lymphoid cells, while AML affects myeloid cells. Their treatments and outcomes also differ.
What is the prognosis for patients with Acute Lymphocytic Leukemia?
The outlook for ALL depends on age, how well the treatment works, and the leukemia’s genetic makeup. Kids usually do better than adults.
What are the survival rates for Acute Lymphocytic Leukemia?
Children with ALL have a much better chance of survival than adults. Thanks to better treatments, kids’ survival rates have improved a lot.
Can Acute Lymphocytic Leukemia be cured?
Many people with ALL can go into complete remission, and some are cured, mainly kids. But, the chance of a cure depends on age and the leukemia’s genetics.
What are the risk factors for developing Acute Lymphocytic Leukemia?
Risk factors for ALL include genetic conditions, exposure to harmful chemicals or radiation, past cancer treatments, and certain immune system problems.
How does the treatment for ALL differ between children and adults?
Kids with ALL often get more intense chemotherapy. Adults might have more treatment choices, like targeted therapies and stem cell transplants.
What is the role of stem cell transplantation in treating Acute Lymphocytic Leukemia?
Stem cell transplants are an option for ALL, mainly for those with high-risk disease or who have relapsed. It replaces the bone marrow with healthy stem cells.
References
- National Center for Biotechnology Information (NCBI): “Acute Lymphoblastic Leukemia.”
- Source: https://www.ncbi.nlm.nih.gov/books/NBK459149/
- National Cancer Institute (NCI): “Adult Acute Lymphoblastic Leukemia Treatment (PDQ®).”
- Source: https://www.cancer.gov/types/leukemia/patient/adult-all-treatment-pdq
- MedlinePlus: “Acute Lymphocytic Leukemia.”
- Source: https://medlineplus.gov/acutelymphocyticleukemia.html
- UCHealth: “Acute Lymphocytic Leukemia.”
- Source: https://www.uchealth.com/en/conditions/acute-lymphocytic-leukemia