Last Updated on November 4, 2025 by mcelik

Did you know over 10 million Americans have osteoporosis? This condition weakens bone density, making bones more likely to break.
Osteoporosis is often called a “silent disease” because it can go unnoticed until a bone breaks. Yet, some people might feel osteoporosis bone pain, which could signal a problem.
As bones lose strength, the chance of breaking them goes up. This not only affects how well you live but also your overall health. It’s important to know the signs and take steps to prevent it.
Key Takeaways
- Osteoporosis is a condition that weakens bones, making them more susceptible to fractures.
- Osteoporosis bone pain can be a sign of an underlying issue.
- Maintaining good bone health is key to avoiding fractures.
- Osteoporosis symptoms can be subtle, but knowing them is vital for early detection.
- Fractures can greatly reduce the quality of life and overall well-being.
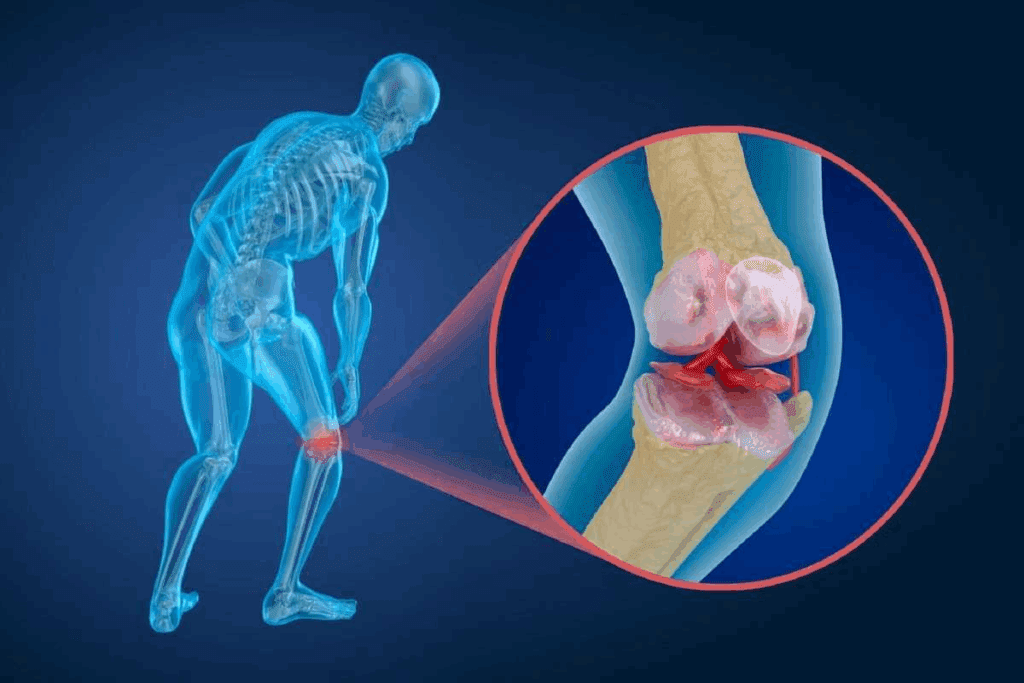
Understanding Osteoporosis and Its Effects on Bone Structure
Osteoporosis changes bone density and structure, causing pain. It weakens bones, making them break easily and causing discomfort.
How Bone Density Decreases Over Time
Bone density drops as bone resorption outpaces formation. This is worse in osteoporosis, leading to bone fragility pain and more fractures. Diabetes can make this worse by harming bone health and raising oxidative stress.
The Relationship Between Bone Microarchitecture and Pain
The bone’s microarchitecture is key to its strength. In osteoporosis, this structure worsens, causing bone weakness discomfort and pain. The type and location of bone damage determine the pain type and duration.
Osteoporosis affects different bones, causing various pains. Knowing how bone structure and pain are linked is vital for managing osteoporosis pain.
Osteoporosis Bone Pain: Characteristics and Common Patterns
Osteoporosis bone pain can show up in different ways. It’s important to know what it looks like. The pain comes from changes in the bones, like less density and damage to the bone structure.
This pain can be hard to handle, being either sudden or ongoing. It’s key to understand the difference. This helps in finding the right treatment.
Distinguishing Osteoporosis Pain from Other Musculoskeletal Conditions
Osteoporosis pain can be mistaken for other bone or muscle issues. But, osteoporosis pain is usually severe joint pain and limited mobility pain. Getting the right diagnosis is critical for the right treatment.
Acute vs. Chronic Pain Experiences in Osteoporosis
Osteoporosis can cause both sudden and ongoing pain. Sudden pain often comes from sudden fracture pain. Ongoing pain is from bone wear and tear. Knowing the type of pain helps pick the best treatment.
Managing osteoporosis pain needs a full plan. It must cover physical and emotional needs. By understanding osteoporosis pain, doctors can tailor treatments for better results.
Common Fracture Sites and Their Specific Pain Signatures
Osteoporosis can cause fractures in different parts of the body. Each fracture has its own pain pattern. Knowing these patterns is key to managing pain effectively.
The Most Vulnerable Skeletal Areas in Osteoporosis
The spine, hip, wrist, and ribs are most affected by osteoporosis. These areas are at high risk because of their bone turnover rates and fracture susceptibility.
| Fracture Site | Common Pain Characteristics |
| Spine | Sharp, localized pain, often radiating to the abdomen or legs |
| Hip | Severe pain in the groin or thigh, difficulty walking or standing |
| Wrist | Pain and swelling in the wrist, difficulty rotating or flexing |
| Ribs | Pain when breathing, coughing, or moving the torso |
How Pain Manifests Differently Based on Fracture Location
The location of a fracture greatly affects the pain type and intensity. For example, vertebral fractures can cause sharp pain that spreads to other areas. Rib fractures may make breathing or moving the torso painful.
Diabetes, often found alongside osteoporosis, can worsen bone loss and fracture risk. Managing both conditions is vital to reduce pain and fracture risk.
Spine Fracture Pain: Understanding Vertebral Compression
Vertebral compression fractures are a common problem linked to osteoporosis, causing severe back pain. These fractures happen when the vertebrae in the spine collapse. This can occur suddenly or over time. It’s important to understand the symptoms and long-term effects of these fractures to manage them effectively.
Symptoms of Acute Vertebral Compression Fractures
The symptoms of acute vertebral compression fractures can be sudden and severe. People often feel sharp lower back ache or chronic neck pain, depending on where the fracture is. The pain gets worse with movement and may be seen as a noticeable deformity or height loss.
In some cases, the fracture can cause numbness, tingling, or weakness in the limbs if nerves are compressed.
Long-term Consequences of Multiple Spinal Fractures
Multiple spinal fractures can lead to long-term consequences, including chronic pain and disability. Repeated vertebral collapses can cause a curvature of the spine, known as kyphosis. This leads to a loss of height and a stooped posture.
This condition can also affect breathing and digestion due to the compression of internal organs. Managing the pain from collapsed vertebra pain and spinal compression fractures needs a complete approach. This includes medical treatment, physical therapy, and making lifestyle changes.
Hip Fracture Pain: A Life-Altering Osteoporosis Complication
Hip fractures from osteoporosis can greatly change a person’s life. The pain and recovery challenges are significant. Osteoporosis makes bones weak, leading to fractures. A hip fracture causes severe pain, less mobility, and a lower quality of life.
Recognizing the Warning Signs of Hip Fracture
It’s important to know the signs of a hip fracture early. Look out for sudden, severe hip pain, trouble walking, and a leg that seems shorter. Some people feel pain in their groin or thigh before a fracture, showing bone weakening.
Recovery Timeline and Pain Management After Hip Fracture
Recovering from a hip fracture is long and hard. It usually starts with surgery, followed by physical therapy to build strength and mobility. Managing pain is key, using medicines and other therapies.
| Recovery Stage | Typical Duration | Pain Management Strategies |
| Immediate Post-Surgery | 1-2 weeks | Medications, rest, ice |
| Physical Therapy | 6-12 weeks | Exercise, physical modalities |
| Full Recovery | 3-6 months | Lifestyle adjustments, continued therapy |
Knowing the recovery time and pain management helps prepare for the journey. It allows for better care decisions.
Wrist and Rib Fractures: Common Painful Injuries in Osteoporosis
Osteoporosis can cause wrist and rib fractures, which are very painful. These fractures hurt a lot and can affect bone health for a long time.
Distal Radius Fractures: Impact on Daily Activities
Wrist fractures happen when the forearm bone breaks near the wrist. They are common in people with osteoporosis because of weak bones. The pain from a wrist fracture makes it hard to do everyday tasks like:
- Lifting objects
- Typing or writing
- Doing household chores
To heal from a wrist fracture, you need to rest and then do physical therapy. Managing osteoporosis well helps avoid these fractures.
Rib Fractures: Pain with Breathing and Movement
Rib fractures are also common in osteoporosis patients. The pain from rib fractures is very bad and gets worse when you breathe or move. This can make it hard to:
- Take deep breaths
- Cough or laugh
- Move around because of pain
To ease rib fracture pain, you need to take medicine and rest. It’s important to watch for any serious problems like pneumonia, which is more common in older people.
Keeping bones healthy through diet, exercise, and medicine can lower fracture risk. Good bone health tips include eating foods rich in calcium and vitamin D, doing exercises that make bones stronger, and not smoking or drinking too much alcohol.
Chronic Back Pain: The Long-term Burden of Spinal Osteoporosis
Spinal osteoporosis can lead to chronic back pain and spinal deformities. This makes everyday tasks hard for those affected.
Back pain from spinal osteoporosis comes from vertebral fractures and spinal deformities. Knowing these causes helps in managing the condition.
Kyphosis Development and Postural Pain
Kyphosis, or a forward rounding of the back, is common in spinal osteoporosis. It causes postural pain because of the abnormal stress on the spine and muscles. As kyphosis gets worse, it changes posture, making pain and discomfort worse.
- Kyphosis can make you lose height and change your body shape.
- Postural pain can be managed with the right exercises and posture adjustments.
- Early treatment is important to stop severe kyphosis.
Strategies for Managing Persistent Spinal Discomfort
Managing persistent spinal discomfort needs a variety of approaches. This includes physical therapy, pain management medications, and lifestyle modifications. Strengthening back muscles and improving posture can help reduce pain.
- Do regular exercises to strengthen back muscles.
- Keep a healthy weight to lessen spine stress.
- Use good posture and ergonomic furniture.
By using these strategies, people with spinal osteoporosis can manage their chronic back pain better. This improves their overall quality of life.
Understanding Osteoporosis and Its Effects on Bone Structure
Osteoporosis changes bones in many ways, affecting their density and structure. As osteoporosis gets worse, bones become weaker and more likely to break. This is because bone density goes down, which is key to bone health.
How Bone Density Decreases Over Time
Bone density naturally drops as we age. But for people with osteoporosis, this happens faster. Diabetes can make osteoporosis worse by affecting bone health and causing more damage.
When bone density falls, the chance of breaking bones goes up. This can lead to more pain and other problems.
The Relationship Between Bone Density and Pain
The link between bone density and pain is complex. Less dense bones are more likely to break, causing pain. Changes in bone structure can also cause pain.
It’s important to manage pain well for people with osteoporosis. This can help them live better and avoid more problems.
Reducing the risk of fractures is also key in treating osteoporosis. Knowing how bone density affects bones helps doctors find better ways to help.
Osteoporosis Bone Pain: Characteristics and Common Patterns
It’s important to understand the signs of osteoporosis bone pain to manage it well. This pain can show up in different ways. Knowing how it acts helps us tell it apart from other bone and muscle problems.
Distinguishing Osteoporosis Pain from Other Musculoskeletal Conditions
Osteoporosis pain often feels like chronic back pain or severe joint pain. But it’s different because it feels deep and aching in the bones. People with it might also feel weak or fragile.
Doctors look at a patient’s history, any fractures, and imaging tests to spot osteoporosis pain. For example, a sudden sudden fracture pain from a bone break can be told apart from other back pain through X-rays.
| Condition | Pain Characteristics | Common Locations |
| Osteoporosis | Deep, aching sensation; weakness or fragility | Spine, hips, wrists |
| Arthritis | Joint pain; stiffness; swelling | Joints (hands, knees, hips) |
| Musculoskeletal Strain | Localized pain; stiffness; tenderness | Muscles and tendons (back, neck, shoulders) |
Acute vs. Chronic Pain Experiences in Osteoporosis
Osteoporosis can cause both acute and chronic pain. Acute pain comes on suddenly, like after a bone breaks. Chronic pain lasts longer and might be because of bone loss or shape changes.
People with osteoporosis might feel limited mobility pain because they’re scared of breaking bones or in pain. This makes them move less, which weakens their bones even more. It’s key to manage both kinds of pain to help those with osteoporosis live better.
Common Fracture Sites and Their Specific Pain Signatures
Osteoporosis can cause fractures in many places, each with its own pain pattern. Knowing these sites and their pain signs is key to managing and treating them well.
The Most Vulnerable Skeletal Areas in Osteoporosis
Osteoporosis hits some parts of the skeleton harder than others. The spine, hip, wrist, and ribs are the most common fracture spots. They are more at risk because of bone loss and the chance of falls or stress.
The spine is a top spot for osteoporotic fractures, leading to vertebral compression fractures. These can cause sharp pain that might spread to the abdomen or legs.
Common Fracture Sites and Associated Pain Characteristics:
| Fracture Site | Pain Characteristics |
| Spine | Acute pain, potentially radiating to abdomen or legs |
| Hip | Severe pain in the groin or thigh, difficulty walking |
| Wrist | Pain and swelling in the wrist area, limited mobility |
| Ribs | Pain with breathing or movement, tenderness to touch |
How Pain Manifests Differently Based on Fracture Location
Pain shows up in different ways based on where the fracture is. For example, spine fractures can cause long-term back pain and a curved back. Hip fractures lead to intense pain that makes it hard to move.
Diabetes, which often goes with osteoporosis, makes bone loss worse. It speeds up bone breakdown. Knowing these differences helps doctors create better treatment plans for both the fracture and the pain.
Spine Fracture Pain: Understanding Vertebral Compression
It’s important to understand the pain from vertebral compression. This happens when a vertebra collapses, often because of osteoporosis. This collapse causes a lot of pain and discomfort.
Symptoms of Acute Vertebral Compression Fractures
Acute vertebral compression fractures cause sudden and severe back pain. The pain is usually in the area of the fracture. It can get worse with movement or activity. Sometimes, the pain spreads to the abdomen or legs.
The symptoms can change based on how bad the fracture is and the person’s health. Common symptoms include:
- Severe back pain
- Pain that worsens with movement
- Localized tenderness
- Potential radiating pain
Long-term Consequences of Multiple Spinal Fractures
Having multiple spinal fractures can lead to long-term problems. These include chronic back pain, kyphosis (a spine curve), and a lower quality of life. The pain from multiple fractures can be very hard to deal with. It can make everyday activities hard and affect your overall well-being.
| Consequence | Description | Impact on Quality of Life |
| Chronic Back Pain | Ongoing pain due to multiple fractures | Reduces ability to perform daily activities |
| Kyphosis | Curvature of the spine due to vertebral collapse | Affects posture and can lead to breathing difficulties |
| Decreased Mobility | Reduced ability to move due to pain and structural changes | Impacts overall health and independence |
Knowing these consequences is key to managing the condition well. By tackling the pain and structural changes from vertebral compression fractures, people can live better lives.
Hip Fracture Pain: A Life-Altering Osteoporosis Complication
Hip fractures are a big worry for people with osteoporosis. They can cause a lot of pain and change their life forever. Osteoporosis makes bones weak, so they break easily. A hip fracture can really affect someone’s life.
Recognizing the Warning Signs of Hip Fracture
It’s important to know the signs of a hip fracture early. Look out for:
- Severe hip pain
- Difficulty walking or standing
- Swelling or bruising around the hip
- Shortening or rotation of the leg
Spotting these signs early can help manage pain and avoid more problems.
Recovery Timeline and Pain Management After Hip Fracture
The time it takes to recover from a hip fracture varies. It usually includes:
- Immediate care to manage pain and stabilize the area
- Surgery to fix the fracture, if needed
- Physical therapy to build strength and move better
Managing pain well is key during recovery. This might involve medicine and other methods.
Wrist and Rib Fractures: Common Painful Injuries in Osteoporosis
Osteoporosis can cause painful injuries like wrist and rib fractures. These injuries make daily life hard. They cause immediate pain and affect bone health over time.
Wrist fractures, like distal radius fractures, are common in those with osteoporosis. They happen when someone falls onto an outstretched hand, stressing the wrist too much.
Distal Radius Fractures: Impact on Daily Activities
Distal radius fractures can make everyday tasks hard. Simple actions like cooking or dressing become tough. The pain and limited movement can really lower your quality of life.
Managing distal radius fractures means using pain relief, physical therapy, and making lifestyle changes. It’s important to avoid heavy lifting and bending to avoid more injuries.
Rib Fractures: Pain with Breathing and Movement
Rib fractures are common in osteoporosis patients, causing pain that gets worse with breathing and movement. This can lead to serious issues like pneumonia because of shallow breathing and limited mobility.
“Rib fractures in osteoporosis patients require careful management to alleviate pain and prevent respiratory complications.”
Managing rib fractures includes pain relief meds, rest, and physical therapy. These help keep lungs working well and improve mobility.
Chronic Back Pain: The Long-term Burden of Spinal Osteoporosis
Chronic back pain affects millions globally, hitting hard those with spinal osteoporosis. It’s not just a symptom but a major part of the disease. It greatly impacts one’s life quality.
Kyphosis Development and Postural Pain
Kyphosis, or the spine’s curvature, often comes with spinal osteoporosis. When vertebrae weaken and might fracture, the spine curves. This leads to a hunched posture and postural pain.
Strategies for Managing Persistent Spinal Discomfort
Dealing with chronic back pain from spinal osteoporosis needs a variety of methods. Physical therapy helps strengthen back muscles, improve posture, and boost flexibility. Pain management includes medication, lifestyle changes, and alternative therapies like acupuncture.
| Strategy | Description | Benefits |
| Physical Therapy | Strengthening back muscles, improving posture, and boosting flexibility | Less pain, better mobility |
| Pain Management Medication | Medication to control chronic pain | Lower pain levels, better life quality |
| Lifestyle Modifications | Daily habit changes to lessen spine strain | Less risk of injury, better health |
Understanding chronic back pain in spinal osteoporosis and using these strategies can help manage the condition. This way, individuals can improve their life quality.
Joint and Muscle Pain Associated with Osteoporosis
Osteoporosis weakens bones, leading to joint and muscle pain. This pain makes daily life hard. It affects how well someone can do everyday tasks.
When Osteoporosis Coexists with Arthritis
Arthritis often goes hand in hand with osteoporosis. It causes joint pain due to inflammation. Managing both conditions is key to reduce pain.
Muscle Strain from Compensatory Postures
Osteoporosis can change how we stand or sit. This is because of bone fractures or deformities. The body tries to balance, leading to muscle strain.
Over time, this strain causes chronic muscle pain. It makes managing osteoporosis pain even harder.
It’s important to understand how osteoporosis, joint pain, and muscle pain are connected. Healthcare providers can then offer better care. They can focus on both bone health and muscle pain.
Diagnosing the Source of Pain in Osteoporosis Patients
Diagnosing pain in osteoporosis patients needs a detailed approach. This includes using imaging studies and clinical assessments. Finding the cause of pain is key to managing and treating it effectively.
Imaging Studies: What They Reveal About Pain Sources
Imaging studies are essential in finding the source of osteoporosis pain. X-rays, DXA scans, and MRI scans show fractures, bone loss, and other changes. These can help explain why a patient is in pain.
| Imaging Technique | Information Provided | Clinical Utility |
| X-rays | Reveal fractures and bone deformities | Assess acute injuries and chronic changes |
| DXA Scans | Measure bone mineral density | Diagnose osteoporosis and monitor treatment response |
| MRI Scans | Detail soft tissue and bone marrow changes | Identify occult fractures and assess spinal cord compression |
The American College of Radiology says imaging is key in osteoporosis diagnosis. It helps doctors check fracture risk and track disease progress.
“Imaging plays a critical role in the diagnosis and management of osteoporosis…”
American College of Radiology
Clinical Assessment and Pain Evaluation Tools
Clinical assessment looks at the patient’s history, symptoms, and physical exam. Pain scales and questionnaires help measure pain levels and track changes.
Managing pain in osteoporosis needs a team effort. It combines insights from imaging and clinical assessments for a tailored treatment plan.
Medical Treatments for Managing Osteoporosis-Related Pain
Osteoporosis-related pain can be very hard to deal with. But, there are many medical treatments to help manage it. Finding the right pain management is key to improving life for those with osteoporosis.
Pharmacological Approaches to Acute Pain Relief
Medicines are a big help in managing pain from osteoporotic fractures. Nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids are often used for quick pain relief. But, opioids are used with caution because of the risk of addiction.
Bone-Strengthening Medications That Address Pain Indirectly
Medicines like bisphosphonates and denosumab are mainly for treating osteoporosis. They help by stopping bone loss. Even though they’re not for pain, they can help by preventing fractures and reducing pain.
| Medication | Mechanism of Action | Effect on Pain |
| Bisphosphonates | Inhibit bone resorption | Indirect pain relief by preventing fractures |
| Denosumab | Inhibits RANKL, reducing bone resorption | Indirect pain relief by preventing fractures |
Interventional Procedures for Severe or Refractory Pain
For those with very bad or hard-to-treat pain, there are special procedures. Vertebroplasty and kyphoplasty involve putting bone cement into broken vertebrae. This helps stabilize the vertebrae and can lessen pain.
Knowing about these treatments helps doctors create a pain management plan. This plan is made just for the needs of each osteoporosis patient.
Non-Pharmacological Approaches to Osteoporosis Pain Relief
Non-pharmacological strategies are key in easing osteoporosis pain. They work alongside traditional treatments to better manage pain.
Physical Therapy Modalities and Their Benefits
Physical therapy is vital for osteoporosis pain relief. It includes therapeutic exercises, manual therapy, and modalities like heat or cold therapy. These methods help lessen pain and boost function.
A physical therapist can create an exercise plan. This plan strengthens muscles around weak bones, lowering fracture risk.
A study published in the Journal of Osteoporosis showed physical therapy cuts pain and boosts life quality in osteoporotic vertebral fracture patients.
Complementary Therapies with Evidence for Pain Reduction
Several complementary therapies help reduce osteoporosis pain. Acupuncture has been shown to lessen pain in chronic pain conditions, including osteoporosis. Massage therapy also helps by easing muscle tension and promoting relaxation.
“Acupuncture and massage therapy can be valuable adjuncts to conventional treatments for managing osteoporosis pain.”
– Expert in Pain Management
Lifestyle Modifications and Their Impact on Pain
Lifestyle changes can greatly affect osteoporosis pain. Maintaining a healthy weight eases bone burden. Quitting smoking and limiting alcohol improve bone health.
Fall prevention strategies like removing hazards and improving lighting also help. These steps reduce fracture risk.
By adding these non-pharmacological methods to their treatment, people with osteoporosis can see a big drop in pain. They also enjoy a better quality of life.
Exercise and Movement: Safe Pain Management Strategies
Osteoporosis pain can be managed with the right exercise and movement. Exercise helps build bone density and improves balance. It also lowers the risk of falls, which is key for those with osteoporosis.
Weight-Bearing Exercises That Build Bone Without Increasing Pain
Weight-bearing exercises are vital for strengthening bones. They can be adjusted based on how severe osteoporosis is. Examples include brisk walking, dancing, and low-impact aerobics. Always do these exercises with a healthcare professional’s guidance to ensure safety.
Benefits of Weight-Bearing Exercises:
- Improves bone density
- Enhances balance and coordination
- Reduces risk of fractures
Activities to Avoid During Acute Pain Episodes
When you’re in pain, avoid activities that could make it worse. High-impact exercises, bending, or twisting should be skipped. Instead, try gentle stretching and relaxation to help manage pain.
Adapting Exercise Programs During Recovery
After a fracture or pain episode, start slowly with exercise. Begin with low-intensity exercises that don’t strain the affected area too much. As you get better, you can gradually add more intense and varied exercises with professional help.
Key Considerations for Adapting Exercise Programs:
- Start with low-intensity exercises
- Gradually increase exercise intensity and duration
- Monitor pain levels and adjust the program as needed
Nutritional Approaches to Reduce Pain and Support Healing
Nutrition is key in reducing pain and healing for those with osteoporosis. A balanced diet helps manage pain and supports bone health. This reduces the risk of fractures and other issues.
Essential Nutrients for Bone Repair and Pain Reduction
Adequate nutrition is vital for bone health and pain management in osteoporosis. Key nutrients include:
- Calcium: Essential for bone repair and density maintenance.
- Vitamin D: Crucial for calcium absorption and bone health.
- Protein: Important for bone matrix formation and overall health.
- Magnesium: Involved in bone mineralization and muscle function.
- Omega-3 fatty acids: May help reduce inflammation and pain.
| Nutrient | Role in Bone Health | Food Sources |
| Calcium | Bone repair and density | Dairy, leafy greens, fortified foods |
| Vitamin D | Calcium absorption | Fatty fish, fortified dairy, sunlight exposure |
| Protein | Bone matrix formation | Meat, poultry, fish, eggs, dairy |
Dietary Patterns That Support Overall Bone Health
Overall dietary patterns also impact bone health. A diet rich in fruits, vegetables, whole grains, and lean proteins supports bone health and reduces pain.
A balanced diet, along with lifestyle changes, is key in managing osteoporosis pain. It also supports overall bone health.
Preventing New Fractures and Additional Pain
Stopping fractures is key for people with osteoporosis to live well. Good prevention can lower fracture and pain risks. This makes life better overall.
Fall Prevention Strategies for Home and Community
Stopping falls is vital to prevent fractures. Making home safer can greatly lower fall risks. Here are some tips:
- Remove tripping hazards like loose rugs and cords
- Make sure lights are bright, in stairs and halls
- Put handrails on both sides of stairs
- Use non-slip mats in the bathroom
Outside, knowing about fall dangers is also key. Watch for uneven sidewalks, icy paths, and other hazards.
Lifestyle Factors That Influence Fracture Risk
Many lifestyle choices affect fracture risk. These include:
- Diet: Eating foods high in calcium and vitamin D is important for bones.
- Exercise: Doing exercises that make bones stronger is helpful.
- Smoking and Alcohol: Not smoking and drinking less can lower fracture risk.
- Body Weight: Keeping a healthy weight helps avoid osteoporosis and fractures.
Monitoring Bone Health to Prevent Pain Progression
Keeping an eye on bone health is essential to stop pain from getting worse. This means:
- Bone Density Tests: Regular tests can spot changes in bone health.
- Medication Adherence: Taking osteoporosis meds as directed can slow disease.
- Regular Check-ups: Seeing doctors often helps track bone health and adjust treatments.
By using these methods, people with osteoporosis can lower their risk of new fractures and pain. This improves their life quality.
When to Seek Immediate Medical Attention for Osteoporosis Pain
It’s important to know the difference between normal osteoporosis pain and a serious issue. People with osteoporosis often have chronic pain. But, some symptoms mean you need to see a doctor right away.
Red Flags That Indicate a New Fracture
A sudden increase in pain or a change in how it feels can be a red flag for a new fracture. For example, if the pain gets sharper or moves to a different spot, it might mean you’ve broken a bone. Also, pain that spreads or gets worse with movement is a sign of trouble.
Some specific red flags include:
- Severe pain that doesn’t improve with rest
- Pain accompanied by numbness, tingling, or weakness
- Visible deformity or bruising
- Difficulty walking or standing
Distinguishing Between Expected Discomfort and Serious Problems
While some pain is normal with osteoporosis, other symptoms need quick medical attention. If the pain is very bad, lasts a long time, or stops you from doing daily things, get help.
Doctors use tests like imaging studies to figure out the cause of pain. They then create a treatment plan. Knowing the red flags and when to get help can help manage osteoporosis better and avoid more problems.
Living with Chronic Osteoporosis Pain: Psychological and Social Aspects
Living with chronic osteoporosis pain is complex. It involves physical pain and mental distress. People with osteoporosis face many challenges that affect their mental health and how they interact with others.
Cognitive-Behavioral Approaches to Pain Management
Cognitive-behavioral therapy (CBT) is a helpful tool for managing chronic pain from osteoporosis. It helps people deal with the mental side of pain. Techniques like changing thoughts, relaxation, and meditation can lessen the emotional pain.
CBT also makes other pain management plans work better. It helps people stick to their treatment plans and take a more active role in managing their pain. Healthcare providers should include CBT in care plans for those with chronic osteoporosis pain.
Support Resources and Community Programs
Support groups and community programs are key for coping with the social side of chronic osteoporosis pain. They offer a place to share experiences, get emotional support, and learn pain management tips. These groups help reduce feelings of loneliness and improve well-being.
Community programs with educational workshops, exercise classes for osteoporosis, and other activities help manage pain better. They create a sense of community and provide valuable resources. This improves the quality of life for those with chronic osteoporosis pain.
Maintaining Social Connections Despite Pain Limitations
Keeping social connections is important for those with chronic osteoporosis pain. Social isolation can make loneliness and depression worse. But, there are ways to stay connected despite pain.
Using technology like video calls and social media can help bridge the gap. Adapting social activities to fit physical limitations also helps. Whether it’s hosting gatherings at home or joining low-impact group activities, staying socially active is key for emotional well-being.
Conclusion: Building a Comprehensive Pain Management Strategy for Osteoporosis
Managing pain is key for those with osteoporosis. A good plan that uses many methods can help lessen pain and make life better.
A treatment plan that includes medicine, non-medical ways, exercise, and diet changes is best. Knowing how pain from osteoporosis works helps people make a plan with doctors.
Keeping bones strong with the right food, exercise, and avoiding falls is vital. This helps prevent fractures and pain. A full pain management plan helps people with osteoporosis feel better and live without pain.
FAQ
What is osteoporosis and how does it affect bone health?
Osteoporosis is a condition where bones lose density and strength. This makes bones brittle and more likely to break. It’s a big risk for fractures.
What are the common symptoms of osteoporosis bone pain?
Symptoms include back, hip, wrist, and rib pain. These pains often come from fractures or compression in the spine. The pain can be sharp or constant and vary in intensity.
How can osteoporosis pain be distinguished from other musculoskeletal conditions?
Doctors use medical history, physical exams, and imaging to tell osteoporosis pain apart. They look for fractures or compression in the spine and low bone density.
What are the most vulnerable skeletal areas in osteoporosis?
The spine, hip, wrist, and ribs are most at risk. These areas are more likely to fracture because of osteoporosis’s effect on bone density and strength.
How can hip fracture pain be managed after a hip fracture?
Pain management includes medicine and physical therapy. Recovery and pain relief plans vary based on the individual.
What are the long-term consequences of multiple spinal fractures?
Long-term effects include chronic back pain and kyphosis. These can greatly affect your quality of life and need ongoing care.
How can exercise and movement help manage osteoporosis-related pain?
Exercise keeps bones strong, improves mobility, and reduces pain. Walking is good, but avoid activities that make pain worse.
What nutritional approaches can help reduce pain and support healing in osteoporosis?
Eating enough calcium and vitamin D is key. Also, eat a balanced diet and avoid foods that harm bone health.
When should I seek immediate medical attention for osteoporosis pain?
Get medical help for sudden, severe pain or if you think you’ve had a new fracture. Look out for intense pain, swelling, or trouble moving.
How can cognitive-behavioral approaches help manage chronic osteoporosis pain?
These approaches teach coping and pain management skills. They can improve your overall well-being and quality of life.
What lifestyle modifications can help prevent new fractures and additional pain?
To prevent fractures and pain, prevent falls, stay healthy, don’t smoke, and limit alcohol.
How can bone health be monitored to prevent pain progression?
Use bone density tests like DEXA scans to track bone health. This helps doctors adjust treatment to stop pain from getting worse.
References
- Choi, Y. J., Kim, K. M., Oh, H. J., Kwak, W. J., Kim, S. W., Min, H. J., & Choi, J. S. (2025). Prevalence and risk factors of osteoporosis: A cross-sectional study in a tertiary center. Journal of Clinical Medicine, 14(3), 856. https://pmc.ncbi.nlm.nih.gov/articles/PMC11677826/