Last Updated on November 18, 2025 by Ugurkan Demir
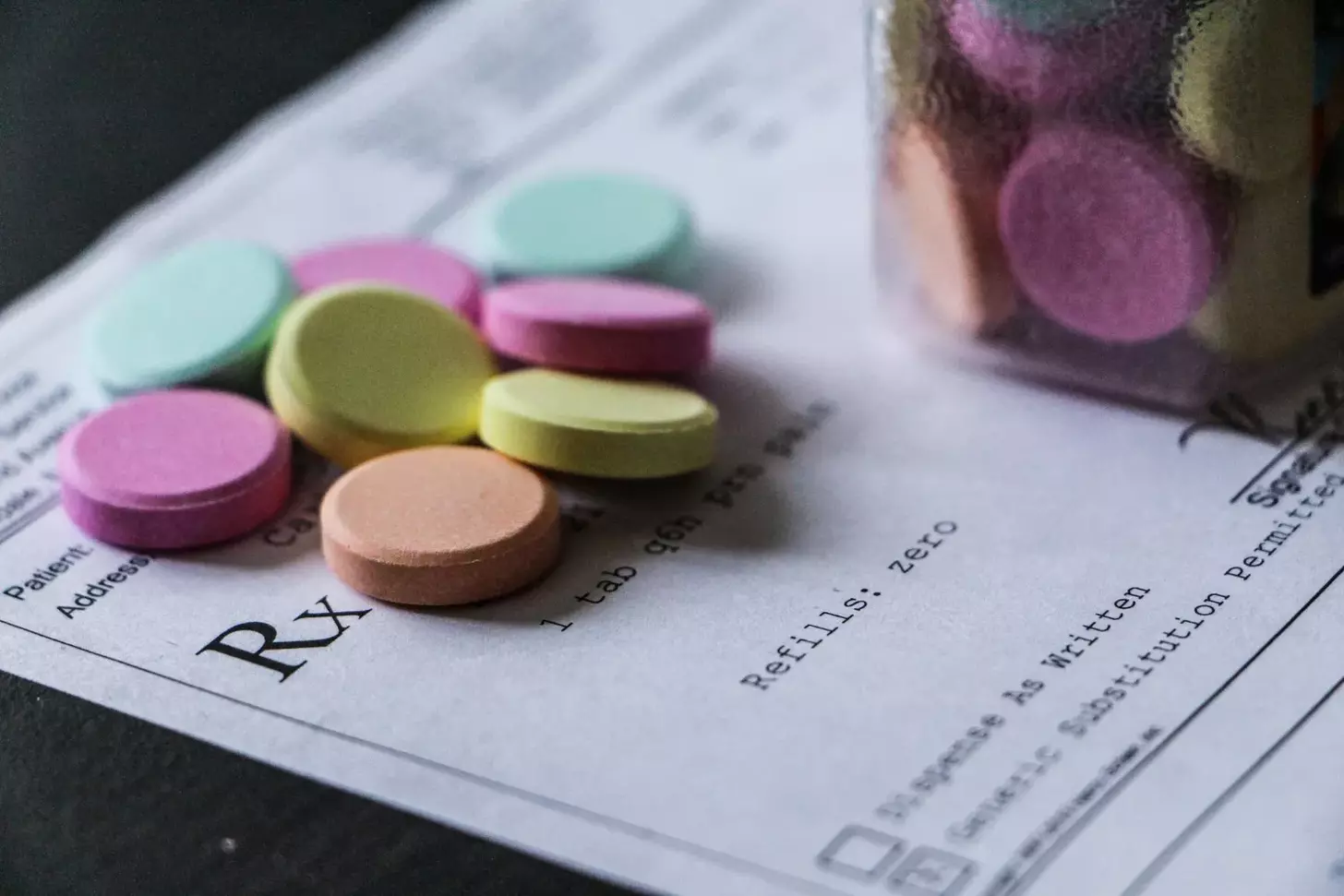
For individuals suffering from debilitating joint pain and stiffness, over-the-counter medications often fall short in providing adequate relief. This is where prescription arthritis pain relievers come into play, offering a more potent solution for managing symptoms.
At Liv Hospital, we understand the importance of effective medication for arthritis pain management. Our team of experts relies on the latest research and medical guidelines to provide top-notch care. Medications such as NSAIDs, DMARDs like methotrexate, biologic agents, and selective COX-2 inhibitors are commonly prescribed to alleviate symptoms.
We recognize that each patient’s needs are unique, and our commitment is to provide personalized care that addresses these needs. By leveraging innovative treatments and a patient-centered approach, we help individuals regain control over their lives.
Key Takeaways
- Prescription medications offer a more potent solution for managing arthritis symptoms.
- Medications like NSAIDs, DMARDs, and biologic agents are commonly prescribed.
- A patient-centered approach is crucial for effective pain management.
- Liv Hospital is committed to providing top-quality, innovative care.
- Our team relies on the latest research and medical guidelines.
Understanding Arthritis Pain and the Need for Prescription Relief

Arthritis pain is a debilitating condition that affects millions of people worldwide, significantly impacting their quality of life. We understand that managing this pain is crucial for maintaining the well-being of individuals suffering from arthritis.
Types of Arthritis and Their Impact on Joint Health
Arthritis encompasses over 100 different conditions that affect the joints, with osteoarthritis and rheumatoid arthritis being the most common forms. Osteoarthritis is characterized by the breakdown of cartilage in joints, leading to pain and stiffness. Rheumatoid arthritis, on the other hand, is an autoimmune disease that causes inflammation and can lead to severe joint damage if not properly managed.
The impact of these conditions on joint health can be significant, resulting in reduced mobility and increased pain. Understanding the specific type of arthritis is essential for developing an effective treatment plan.
When Over-the-Counter Options Are Not Enough
Over-the-counter (OTC) medications such as ibuprofen and acetaminophen are often the first line of defense against arthritis pain. However, for many individuals, these options do not provide sufficient relief, or they may cause undesirable side effects. In such cases, prescription medications become a necessary consideration for achieving adequate pain management.
The Role of Prescription Medications in Arthritis Management
Prescription medications play a critical role in managing arthritis pain for those who do not find relief with OTC options. These medications can include nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs), among others. By targeting the underlying causes of arthritis pain, prescription medications can help improve joint function and overall quality of life.
We recognize the importance of a tailored approach to arthritis pain management, incorporating the most appropriate prescription medications based on the individual’s specific condition and needs.
How Prescription Arthritis Pain Relievers Work

Understanding how prescription medications work is crucial for effective arthritis pain management. Prescription arthritis pain relievers are designed to address the complex nature of arthritis pain, which can involve inflammation, joint damage, and neurological components.
Targeting Inflammation vs. Pain Signals
Different classes of prescription arthritis pain relievers work by targeting either inflammation or pain signals. Nonsteroidal anti-inflammatory drugs (NSAIDs), for example, primarily target inflammation, which is a key driver of pain in many forms of arthritis. On the other hand, some medications focus on interrupting pain signals to the brain, providing relief without directly addressing inflammation.
Short-Term Relief vs. Disease Modification
Prescription arthritis pain relievers can be categorized based on whether they provide short-term relief or modify the disease process. Analgesics and NSAIDs are typically used for short-term pain relief, while Disease-Modifying Antirheumatic Drugs (DMARDs) and biologic agents are designed to slow disease progression and potentially modify the course of arthritis.
Systemic vs. Topical Delivery Methods
The delivery method of prescription arthritis pain relievers can significantly impact their effectiveness and side effect profile. Systemic delivery methods, such as oral tablets or injections, distribute the medication throughout the body, while topical delivery methods, like creams or gels, are applied directly to the affected area, potentially reducing systemic side effects.
By understanding these different approaches, healthcare providers can tailor treatment plans to individual patient needs, optimizing arthritis pain management.
Prescription-Strength NSAIDs for Arthritis Management
When managing arthritis pain, prescription-strength NSAIDs play a crucial role in providing relief for patients who don’t respond adequately to over-the-counter options. These medications are designed to reduce inflammation and alleviate pain, making them a cornerstone in the treatment of various forms of arthritis.
Prescription-strength NSAIDs are more potent than their over-the-counter counterparts, offering a more significant impact on pain and inflammation. This increased potency is particularly beneficial for patients with moderate to severe arthritis symptoms.
Diclofenac (Voltaren, Cambia)
Diclofenac is a widely used prescription NSAID available in various formulations, including topical gels and oral tablets. It’s effective for managing pain and inflammation associated with osteoarthritis and rheumatoid arthritis. The topical form, Voltaren gel, is particularly useful for localized pain relief, while oral forms like Cambia are used for acute migraine treatment, showcasing its versatility.
Indomethacin (Indocin)
Indomethacin is another potent NSAID often prescribed for moderate to severe arthritis pain. It’s particularly effective for ankylosing spondylitis and gout. However, due to its potential side effects, it’s usually considered when other NSAIDs have failed to provide adequate relief. Monitoring by a healthcare provider is essential when using indomethacin due to its potential for gastrointestinal and other side effects.
Meloxicam (Mobic)
Meloxicam is a preferred NSAID for many patients due to its relatively favorable side effect profile compared to other prescription-strength NSAIDs. It’s used to treat osteoarthritis and rheumatoid arthritis, offering once-daily dosing convenience. Meloxicam’s effectiveness in reducing pain and inflammation while being generally well-tolerated makes it a valuable option in arthritis management.
In conclusion, prescription-strength NSAIDs like diclofenac, indomethacin, and meloxicam are vital in managing arthritis pain. Each medication has its unique characteristics, benefits, and potential side effects. By understanding these differences, healthcare providers can tailor treatment plans to individual patient needs, optimizing arthritis pain management.
Selective COX-2 Inhibitors: Targeted Arthritis Pain Relievers Prescription Options
Selective COX-2 inhibitors represent a significant advancement in the management of arthritis pain, offering targeted relief with potentially fewer side effects. These medications work by specifically inhibiting the COX-2 enzyme, which is involved in the inflammatory process, while sparing the COX-1 enzyme, thereby reducing the risk of gastrointestinal complications.
Celecoxib (Celebrex)
Celecoxib, marketed under the brand name Celebrex, is a widely prescribed selective COX-2 inhibitor. It has been shown to be effective in managing pain and inflammation associated with osteoarthritis and rheumatoid arthritis. The medication is available in capsule form and is typically taken once or twice daily.
Key benefits of celecoxib include:
- Effective pain relief for arthritis patients
- Reduced risk of gastrointestinal ulcers compared to traditional NSAIDs
- Once or twice daily dosing for convenience
Appropriate Candidates for COX-2 Inhibitors
COX-2 inhibitors are particularly beneficial for patients who are at high risk of gastrointestinal complications from traditional NSAIDs. This includes patients with a history of ulcers, those taking anticoagulant medications, and older adults. However, the decision to prescribe COX-2 inhibitors should be made on a case-by-case basis, considering the individual patient’s risk factors and medical history.
Factors to consider when determining candidacy for COX-2 inhibitors include:
- History of gastrointestinal bleeding or ulcers
- Use of anticoagulant or corticosteroid medications
- Age and overall health status
Cardiovascular Considerations
While COX-2 inhibitors offer several benefits, they are not without risks. One of the significant concerns is their potential impact on cardiovascular health. Some studies have suggested that long-term use of COX-2 inhibitors may increase the risk of cardiovascular events, such as heart attacks and strokes.
To mitigate cardiovascular risks:
- Use the lowest effective dose for the shortest duration necessary
- Monitor patients with pre-existing cardiovascular disease closely
- Consider alternative treatments for patients at high cardiovascular risk
Disease-Modifying Antirheumatic Drugs (DMARDs)
In the treatment of arthritis, DMARDs play a vital role in reducing inflammation and preventing joint damage. These medications are particularly important for patients with rheumatoid arthritis and other inflammatory forms of arthritis. We will explore how DMARDs work and discuss some of the most commonly used options.
DMARDs are a class of medications that can slow the progression of arthritis, reducing the risk of long-term damage and improving patient outcomes. Unlike some other arthritis treatments that focus solely on symptom relief, DMARDs target the underlying disease process.
Methotrexate: The Gold Standard for Rheumatoid Arthritis
Methotrexate is often considered the gold standard for treating rheumatoid arthritis due to its effectiveness in reducing disease activity and slowing disease progression. It works by suppressing the immune system, thereby reducing inflammation and joint damage.
We typically start with a low dose of methotrexate and gradually increase it as needed and as tolerated by the patient. Regular monitoring is essential to minimize potential side effects, such as liver toxicity and bone marrow suppression.
Hydroxychloroquine (Plaquenil)
Hydroxychloroquine, commonly known by its brand name Plaquenil, is another DMARD used in the treatment of rheumatoid arthritis and lupus. It is often used in combination with other DMARDs, such as methotrexate, to enhance its effectiveness.
While hydroxychloroquine can be beneficial, it requires regular eye exams to monitor for potential retinal toxicity, a rare but serious side effect.
Sulfasalazine (Azulfidine)
Sulfasalazine, known by its brand name Azulfidine, is used to treat rheumatoid arthritis and sometimes ulcerative colitis. It works by reducing inflammation in the body and is often used in combination with other DMARDs.
Common side effects of sulfasalazine include gastrointestinal issues and headaches. We monitor patients closely to manage these effects and adjust the treatment plan as necessary.
Biologic Agents for Severe Arthritis Pain
Biologic agents have revolutionized the treatment of severe arthritis pain by targeting specific molecules involved in the inflammatory process. These medications are often prescribed for patients who have not responded adequately to conventional treatments, offering a new avenue of relief.
Biologic agents are a class of medications that are designed to target specific proteins or cells involved in the inflammation process. Unlike traditional DMARDs, biologics are made from living cells and are more targeted in their approach, which can lead to fewer side effects for some patients.
TNF Inhibitors (Adalimumab, Etanercept)
TNF inhibitors are a type of biologic agent that blocks the action of tumor necrosis factor-alpha (TNF-alpha), a protein that promotes inflammation. By inhibiting TNF-alpha, these medications reduce inflammation and slow down disease progression. Adalimumab and etanercept are examples of TNF inhibitors commonly used in the treatment of rheumatoid arthritis and other inflammatory conditions.
IL-6 Inhibitors (Tocilizumab)
IL-6 inhibitors target interleukin-6 (IL-6), another protein involved in the inflammatory process. Tocilizumab is an example of an IL-6 inhibitor that has been shown to be effective in reducing inflammation and improving symptoms in patients with rheumatoid arthritis. By blocking IL-6, tocilizumab can help reduce joint damage and improve quality of life.
T-Cell Activation Inhibitors (Abatacept)
T-cell activation inhibitors, such as abatacept, work by modulating the immune system’s response. They prevent the activation of T-cells, which are a type of immune cell involved in the inflammatory process. By inhibiting T-cell activation, abatacept can help reduce inflammation and slow disease progression in patients with rheumatoid arthritis.
The use of biologic agents represents a significant advancement in the treatment of severe arthritis pain. By targeting specific molecules involved in inflammation, these medications offer a more targeted approach to managing arthritis, potentially leading to better outcomes for patients.
Corticosteroids for Acute Arthritis Flares
Acute arthritis flares can be debilitating, but corticosteroids offer a powerful tool to quickly reduce inflammation and improve quality of life. These potent anti-inflammatory medications are often prescribed to manage severe arthritis symptoms that are not adequately controlled with other treatments.
Oral Prednisone Regimens
Oral corticosteroids, such as prednisone, are commonly used to treat acute arthritis flares. Prednisone is typically administered in a tapering dose to minimize side effects while effectively reducing inflammation. The initial dose is usually higher to quickly bring the inflammation under control, followed by a gradual reduction in dosage over several days or weeks.
The tapering schedule is crucial to avoid withdrawal symptoms and allow the body to adjust to the decrease in corticosteroid levels. The duration of treatment varies depending on the severity of the flare and the patient’s response to the medication.
Injectable Corticosteroids for Joint-Specific Relief
For patients with localized arthritis symptoms, injectable corticosteroids can provide targeted relief. Corticosteroid injections directly into the affected joint can rapidly reduce inflammation and pain, improving joint function and mobility. This method is particularly useful for patients with monoarticular or oligoarticular arthritis.
Balancing Benefits Against Long-Term Risks
While corticosteroids are effective in managing acute arthritis flares, their long-term use is associated with several potential risks. Prolonged corticosteroid use can lead to osteoporosis, cataracts, and increased risk of infections. Therefore, it is essential to carefully weigh the benefits against the risks and consider alternative treatments for long-term management.
| Benefits of Corticosteroids | Risks of Long-Term Use |
|---|---|
| Rapid reduction in inflammation | Osteoporosis |
| Effective pain relief | Cataracts |
| Improved joint function | Increased risk of infections |
By understanding the benefits and risks of corticosteroids, healthcare providers can develop effective treatment plans that balance short-term relief with long-term safety. This approach enables patients to manage their arthritis symptoms effectively while minimizing potential complications.
Prescription Analgesics for Severe Arthritis Pain
For patients suffering from severe arthritis pain, prescription analgesics offer a crucial line of defense when over-the-counter options are insufficient. These medications are designed to provide more potent pain relief, helping patients manage their condition more effectively.
Tramadol: A Middle-Ground Option
Tramadol is a prescription analgesic that is often considered for patients with moderate to severe arthritis pain. It works by binding to opioid receptors in the brain, altering the perception of pain. Unlike stronger opioids, tramadol is generally considered to have a lower risk of dependence, making it a middle-ground option for some patients.
Key benefits of tramadol include:
- Effective for moderate to severe pain
- Lower risk of dependence compared to stronger opioids
- Available in various formulations, including immediate and extended release
Opioid Medications and Their Limited Role
Opioid medications are powerful analgesics that may be considered for patients with severe arthritis pain that is not responsive to other treatments. However, due to their high potential for dependence and side effects, their use is generally limited to short-term periods or specific circumstances.
| Opioid Medication | Common Use | Notable Side Effects |
|---|---|---|
| Oxycodone | Severe pain management | Constipation, drowsiness, dependence |
| Hydrocodone | Moderate to severe pain | Nausea, dizziness, dependence |
Combination Therapies with Acetaminophen
Some prescription analgesics are formulated in combination with acetaminophen to enhance pain relief. These combination therapies can be effective for managing severe arthritis pain while potentially reducing the required dose of each individual medication.
Example of combination therapy: Tramadol/Acetaminophen (Ultracet) combines the opioid-like effects of tramadol with the pain-relieving properties of acetaminophen, offering a synergistic effect for pain management.
By understanding the different types of prescription analgesics available, healthcare providers can tailor treatment plans to meet the specific needs of their patients, balancing efficacy with safety considerations.
Special Considerations for Arthritis Pain Medication for Elderly Patients
Arthritis pain management in older adults involves special considerations to ensure safe and effective treatment. As people age, their physiological responses to medications can change significantly, making it crucial to tailor treatment plans to individual needs.
Adjusted Dosing Requirements
Elderly patients often require adjusted dosing of arthritis pain medications due to decreased renal function and changes in body composition. For instance, prescription-strength NSAIDs like diclofenac may need to be started at lower doses to avoid adverse effects. We must carefully assess each patient’s renal function and other health factors to determine the most appropriate dosing regimen.
Medication Interactions and Polypharmacy
Many elderly patients take multiple medications for various health conditions, increasing the risk of drug interactions. When managing arthritis pain, we need to consider potential interactions between pain relievers and other medications, such as anticoagulants or certain antidepressants. For example, combining NSAIDs with certain other drugs can increase the risk of gastrointestinal bleeding. A thorough medication review is essential to minimize these risks.
Monitoring Kidney and Liver Function
Regular monitoring of kidney and liver function is critical when prescribing arthritis pain medications, especially NSAIDs and certain DMARDs. Age-related declines in organ function can affect drug metabolism and excretion, potentially leading to toxic levels. We recommend regular blood tests to assess kidney and liver function in elderly patients on long-term arthritis pain medication.
Balancing Pain Relief with Safety Concerns
Effective arthritis pain management in elderly patients requires balancing the need for pain relief against potential safety concerns. While it’s crucial to control pain to maintain quality of life, we must also be mindful of the risks associated with certain medications. For instance, the use of opioid medications carries risks of dependency and falls. We need to weigh these risks against the benefits of pain relief when developing treatment plans.
By carefully considering these factors, we can create effective and safe arthritis pain management plans for elderly patients, improving their quality of life while minimizing potential risks.
Conclusion: Creating an Effective Arthritis Pain Management Plan
Effective arthritis pain management requires a multi-faceted approach that incorporates various treatment options. We have discussed the different types of prescription arthritis pain relievers, including NSAIDs, COX-2 inhibitors, DMARDs, biologic agents, and corticosteroids.
A comprehensive management plan should include a combination of medications, lifestyle modifications, and alternative therapies to achieve optimal joint pain relief. By working with their healthcare providers, patients can develop a personalized plan that addresses their specific needs and health status.
Medication for arthritis pain management is just one aspect of a broader treatment strategy. We emphasize the importance of a collaborative approach between patients and healthcare providers to create a tailored plan that incorporates the most effective pain relievers for arthritis.
By adopting a comprehensive arthritis pain management plan, individuals can experience improved joint health, reduced pain, and enhanced overall well-being. Effective management enables patients to maintain their independence and quality of life.
FAQ
What are the most common types of arthritis that require prescription pain relievers?
The most common types of arthritis that require prescription pain relievers are rheumatoid arthritis, osteoarthritis, and psoriatic arthritis. These conditions can cause significant joint pain and inflammation, often necessitating stronger medications than over-the-counter options.
How do prescription-strength NSAIDs differ from over-the-counter NSAIDs?
Prescription-strength NSAIDs have higher dosages and are often more potent than their over-the-counter counterparts. They are used when over-the-counter options are not sufficient to manage arthritis pain. Examples include diclofenac (Voltaren, Cambia) and meloxicam (Mobic).
What are the benefits and risks of using selective COX-2 inhibitors for arthritis pain?
Selective COX-2 inhibitors, such as celecoxib (Celebrex), target inflammation while reducing the risk of gastrointestinal side effects compared to traditional NSAIDs. However, they may increase cardiovascular risks, so their use should be carefully considered, especially for patients with heart conditions.
How do DMARDs work in managing arthritis, and what are some examples?
DMARDs (Disease-Modifying Antirheumatic Drugs) work by modifying the disease process, slowing down disease progression, and reducing joint damage. Examples include methotrexate, hydroxychloroquine (Plaquenil), and sulfasalazine (Azulfidine). They are often used in treating rheumatoid arthritis and other inflammatory arthritides.
What is the role of corticosteroids in managing acute arthritis flares?
Corticosteroids are potent anti-inflammatory medications used to manage acute arthritis flares. They can be administered orally or via injection directly into the affected joint. While effective for short-term relief, long-term use carries risks such as osteoporosis and increased infection risk.
Are opioid medications commonly prescribed for arthritis pain?
Opioid medications are generally not recommended as a first-line treatment for arthritis pain due to their potential for addiction and side effects. However, in some cases, they may be considered for short-term use in severe cases where other treatments have failed.
What special considerations are there for elderly patients taking arthritis pain medication?
Elderly patients require adjusted dosing, careful monitoring for medication interactions, and regular checks on kidney and liver function due to decreased physiological reserve and potential polypharmacy. Balancing pain relief with safety concerns is crucial.
Can arthritis pain management plans include a combination of different medications?
Yes, arthritis pain management plans often involve a combination of different medications, including NSAIDs, DMARDs, biologics, and analgesics, tailored to the individual’s specific condition, severity, and response to treatment. This multi-faceted approach aims to optimize pain relief and minimize side effects.
How often should patients on prescription arthritis pain relievers be monitored by their healthcare provider?
Patients on prescription arthritis pain relievers should be regularly monitored by their healthcare provider to assess the effectiveness of the treatment, check for potential side effects, and adjust the treatment plan as necessary. The frequency of monitoring depends on the medication and the patient’s condition.