Last Updated on November 26, 2025 by Bilal Hasdemir

When the immune system attacks the body’s own tissues, it can cause serious conditions like rheumatoid arthritis and multiple sclerosis. At Liv Hospital, we know how vital it is to find the right treatment for autoimmune disorders. Our team is committed to providing care that is both innovative and compassionate, based on the latest research.
New treatments, such as antigen-specific immunotherapies, bring hope for managing autoimmune diseases. We will look at the best ways to treat and control these conditions. This includes medical treatments and changes in lifestyle to help you manage your condition and enhance your life quality.
Key Takeaways
- Understanding the immune system’s role in autoimmune disorders is key for effective treatment.
- Liv Hospital offers innovative, patient-focused care for autoimmune diseases.
- Antigen-specific immunotherapies are a promising new treatment approach.
- Combining medical treatments with lifestyle modifications can improve treatment outcomes.
- Personalized care and compassion are at the heart of our treatment approach.
Understanding Autoimmune Disorders: When Your Body Attacks Itself

Autoimmune diseases happen when the immune system can’t tell the difference between self and non-self. This leads to millions of people worldwide being affected. These diseases occur when the immune system attacks the body’s own tissues, causing inflammation and damage to various organs and systems.
What Occurs When the Immune System Attacks the Body
The immune system is meant to protect us from harmful invaders like bacteria and viruses. But in autoimmune disorders, it mistakenly attacks the body’s own cells and tissues. This can cause a range of health problems, depending on which tissues or organs are targeted.
In rheumatoid arthritis, the immune system attacks the lining of the joints. This causes pain, swelling, and can lead to joint damage and deformity. Lupus, on the other hand, can affect multiple organs like the skin, kidneys, and joints, due to a widespread immune system attack.
Common Autoimmune Conditions and Their Prevalence
Autoimmune diseases come in many forms, each with its own characteristics and how common they are. Some of the most common include:
- Rheumatoid arthritis
- Lupus
- Multiple sclerosis
- Type 1 diabetes
- Hashimoto’s thyroiditis
These conditions affect a significant number of people worldwide. It’s estimated that up to 5% of the global population has some form of autoimmune disease. This highlights the need for ongoing research into their causes and treatments.
The Inflammatory Process and Organ Damage
The immune system’s attack on the body’s tissues triggers inflammation. This is marked by redness, heat, swelling, and pain in the affected areas. Chronic inflammation from autoimmune disorders can cause lasting damage to organs over time.
In multiple sclerosis, the immune system attacks the protective covering of nerve fibers. This leads to inflammation and damage to the central nervous system. Symptoms include numbness, weakness, and vision problems. Understanding how inflammation affects different organs is key to developing effective treatments for autoimmune diseases.
Recognizing the Signs: Early Detection of Autoimmune Disorders
Autoimmune disorders can be tricky to spot because their symptoms are often vague. Spotting these signs early is key. It helps in getting the right treatment sooner and can prevent serious damage later.
Common Symptoms Across Different Autoimmune Conditions
Autoimmune diseases vary, but they share some common symptoms. These include persistent fatigue, joint pain, and skin rashes. For example, lupus and rheumatoid arthritis often cause joint pain and swelling. Type 1 diabetes might start with symptoms like thirst and urination.
Other symptoms seen in many autoimmune diseases are:
- Muscle weakness
- Fever
- Hair loss
- Sensitivity to sunlight
Seeing these symptoms doesn’t always mean you have an autoimmune disease. But, if they last a long time or get worse, you should see a doctor.
Distinguishing Between General Illness and Autoimmune Reactions
Telling apart general illness from autoimmune reactions can be hard because symptoms overlap. Yet, certain patterns and how severe symptoms are can hint at an autoimmune disease. For instance, if symptoms keep getting worse, it might be an autoimmune issue. Also, having many symptoms at once is a warning sign.
“Early diagnosis and treatment of autoimmune diseases can significantly improve the quality of life for patients. It’s vital for healthcare providers to be alert and for patients to know when to seek medical help.” – Source
When to Seek Medical Attention
Knowing when to see a doctor is important for managing autoimmune diseases well. If you’re dealing with symptoms that won’t go away or are really bad, you should talk to a healthcare professional. Catching these diseases early can lead to better treatment plans and lower the risk of serious problems later.
| Symptom | Possible Autoimmune Condition | Action |
|---|---|---|
| Joint pain and swelling | Rheumatoid Arthritis | Consult a rheumatologist |
| Skin rashes and sensitivity to sunlight | Lupus | Seek dermatological evaluation |
| Increased thirst and urination | Type 1 Diabetes | Visit an endocrinologist |
Being aware of autoimmune disease symptoms and getting medical help early can greatly improve treatment outcomes. It helps manage these conditions more effectively.
Diagnostic Journey: Confirming an Autoimmune Condition
Getting a diagnosis for an autoimmune condition is complex. It involves many tests and evaluations. Accurate diagnosis is key for a good treatment plan.
Getting a diagnosis can be tough. Our team is here to help you through it. We do it with care and expertise.
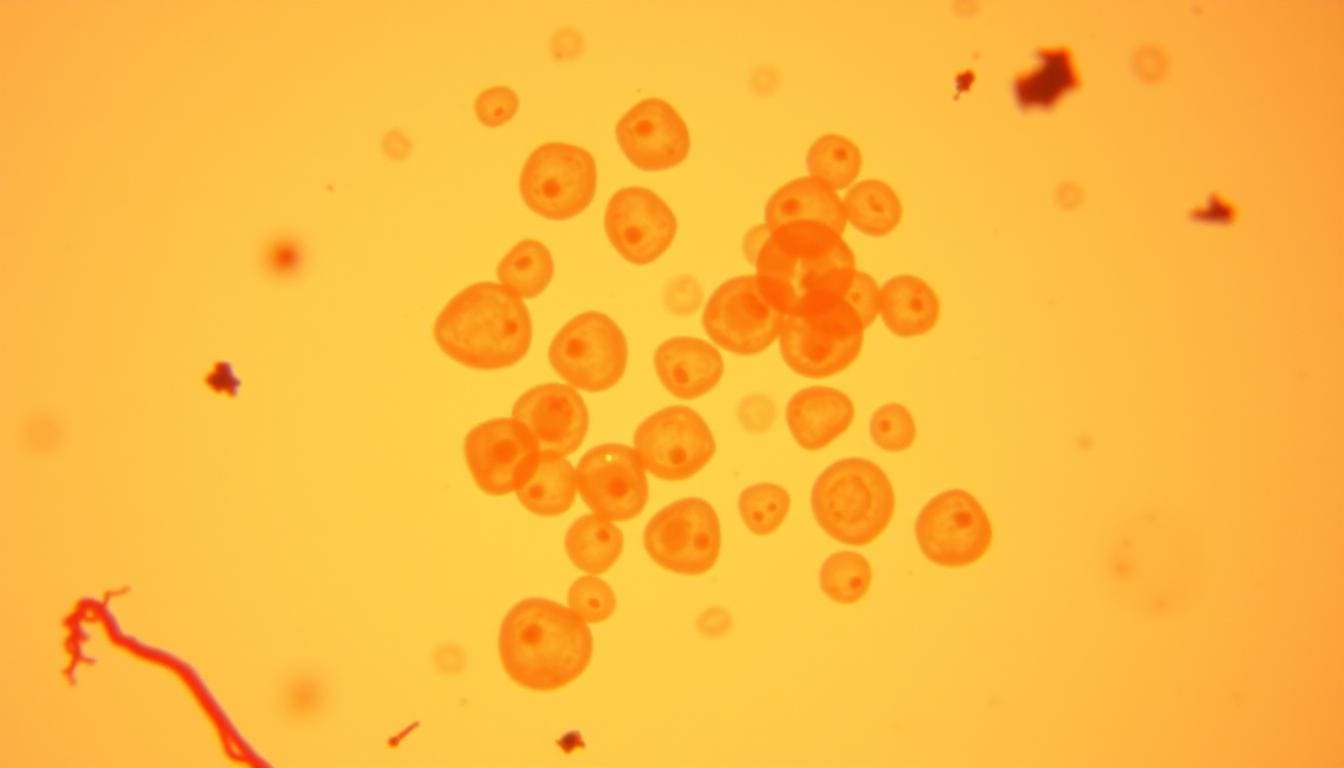
Blood Tests and Biomarkers
Blood tests are vital for diagnosing autoimmune conditions. They look for specific biomarkers. Biomarkers show biological processes or how well treatments work.
For example, certain autoantibodies can signal an autoimmune condition. Tests like the antinuclear antibody (ANA) test are common. They check for autoantibodies related to diseases like rheumatoid arthritis or lupus.
Imaging and Specialized Testing
Imaging studies like X-rays, ultrasound, or MRI help see organ damage or inflammation. Special tests, including biopsies, give more details about the condition.
Working with Specialists for Accurate Diagnosis
It’s important to work with healthcare specialists like rheumatologists or immunologists. They know how to read test results. They can spot patterns of specific autoimmune conditions and create a treatment plan.
By using clinical evaluation and advanced diagnostic tools, we make sure patients get the right diagnosis. Then, they can get the right treatment for their autoimmune condition.
How to Correct Autoimmune Disorder: Medical Treatment Approaches
Medical treatment for autoimmune disorders is not a one-size-fits-all solution. It needs a personalized approach. We will look at different medical ways to manage these conditions. The goal is to stop the immune system from attacking the body’s tissues.
Immunosuppressant Medications
Immunosuppressant medications are key in treating autoimmune disorders. They calm down the immune system’s overactive response. This reduces inflammation and damage to tissues. Drugs like azathioprine, cyclophosphamide, and mycophenolate mofetil are often used.
While they work well, it’s important to watch for side effects. These can include a higher risk of infections.
Corticosteroids and Their Role
Corticosteroids, such as prednisone, are used to quickly reduce inflammation. They help control symptoms during flare-ups. But, they should be used for short periods because of possible side effects.
Side effects can include osteoporosis, weight gain, and mood changes. Long-term use needs careful thought and monitoring.
Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs are important for treating autoimmune disorders, like rheumatoid arthritis. They slow down disease progression and protect joints and other body parts. Common DMARDs include methotrexate, hydroxychloroquine, and sulfasalazine.
DMARDs can be used alone or with other treatments. They are a vital part of managing autoimmune disorders.
Working closely with healthcare providers is key when managing autoimmune disorders. They help find the best treatment plan. This might include different treatments, lifestyle changes, and regular check-ups to adjust the treatment as needed.
Targeted Biologic Therapies: Precision Treatment Options
Biologic therapies are precise treatments for autoimmune diseases. They work by targeting specific immune responses. This approach has changed how we manage autoimmune conditions by focusing on the root causes of inflammation and tissue damage.
Modulating Immune Responses
Biologic therapies target specific molecules in the immune response. This targeted approach is better than traditional treatments because it doesn’t suppress the immune system too much. For example, biologics can block cytokines, which are proteins that cause inflammation.
Types of Biologic Treatments
There are several biologic treatments for autoimmune diseases, including:
- Tumor Necrosis Factor (TNF) inhibitors
- Interleukin inhibitors
- B cell-targeting therapies
Each type targets a different part of the immune response. This gives patients different treatment options.
| Biologic Type | Mechanism of Action | Common Uses |
|---|---|---|
| TNF inhibitors | Inhibit TNF, reducing inflammation | Rheumatoid arthritis, Crohn’s disease |
| Interleukin inhibitors | Block specific interleukins involved in inflammation | Psoriasis, rheumatoid arthritis |
| B cell-targeting therapies | Deplete B cells, reducing autoimmune responses | Multiple sclerosis, lupus |
Candidates for Biologic Therapy
Biologic therapy is for patients who haven’t gotten better with usual treatments or have very active disease. Identifying suitable candidates means looking at disease severity, past treatment results, and overall health.
Monitoring Effectiveness and Side Effects
It’s important to keep an eye on how well the therapy works and any side effects. Regular checks include looking at disease activity, watching for side effects, and adjusting treatment plans if needed.
Are Autoimmune Diseases Curable? Understanding Treatment Goals
Understanding autoimmune diseases is complex. These diseases happen when the body’s immune system attacks itself. Finding a “cure” is hard because of this complexity.
The Difference Between Cure and Remission
It’s key to know the difference between a “cure” and “remission.” A cure means the disease is gone forever. Remission means symptoms are less or gone, but the disease is not fully gone. For many, getting to remission is a good goal.
Remission is not the same as a cure, but it can make life better. Doctors aim to keep patients in remission.
Conditions with Higher Remission Rates
Some autoimmune diseases are easier to manage than others. For example, vasculitis and rheumatoid arthritis can be controlled well with treatment.
- Rheumatoid Arthritis: Modern treatments help many patients reach remission.
- Type 1 Diabetes: Though not curable, good management can feel like remission.
- Lupus: Some patients can go into remission, but treatment needs to keep changing.
Setting Realistic Expectations for Treatment Outcomes
It’s important for patients to know what to expect from treatment. While a cure might not be possible, managing the disease well can greatly improve life.
Patients should talk to their doctors to set realistic goals. A good plan might include medicine, lifestyle changes, and regular check-ups.
By understanding the difference between cure and remission, patients can manage their disease better. This leads to a better quality of life.
Lifestyle Modifications to Combat Autoimmune Disease
Making lifestyle changes can help manage autoimmune diseases. By choosing the right diet, exercise, and stress management, you can control symptoms and live better.
Anti-Inflammatory Diet Approaches
An anti-inflammatory diet is key for autoimmune disease management. It means eating foods that fight inflammation and avoiding those that make it worse. Foods to focus on include:
- Omega-3 rich foods: Fatty fish like salmon and sardines.
- Antioxidant-rich foods: Berries, leafy greens, and other fruits and vegetables.
- Whole grains: Brown rice, quinoa, and whole wheat.
- Healthy fats: Olive oil and avocados.
It’s also important to avoid foods that cause inflammation. This includes processed meats, sugary drinks, and refined carbs. Talking to a nutritionist can help create a diet plan that’s right for you.
Exercise and Physical Activity Guidelines
Exercise is essential for health and managing autoimmune symptoms. It’s important to balance activity with rest. Good exercises include:
- Low-impact aerobics: Walking, swimming, and cycling.
- Strength training: Resistance exercises to keep muscle mass.
- Flexibility exercises: Yoga and Pilates to improve flexibility and reduce stress.
| Exercise Type | Benefits | Frequency |
|---|---|---|
| Low-impact aerobics | Improves cardiovascular health | 3-4 times a week |
| Strength training | Maintains muscle mass | 2-3 times a week |
| Flexibility exercises | Reduces stress and improves flexibility | 2-3 times a week |
Stress Management Techniques
Stress can make autoimmune symptoms worse. Good ways to manage stress include:
- Meditation and mindfulness: Practices that reduce stress and anxiety.
- Yoga and tai chi: Exercises that combine physical movement with mindfulness.
- Cognitive-behavioral therapy (CBT): A therapy to manage stress and negative thoughts.
By making these lifestyle changes, people with autoimmune diseases can better manage their conditions and improve their well-being.
Nutritional Interventions: How Diet Affects Autoimmune Conditions
Understanding how nutrition affects autoimmune diseases is vital for effective treatment. Autoimmune conditions happen when the body’s immune system attacks its own tissues. This leads to inflammation and damage. Nutritional interventions can help by reducing inflammation, boosting immune function, and improving overall health.
Elimination Diets and Food Sensitivities
Elimination diets are a key nutritional intervention for autoimmune diseases. They help find out which foods cause sensitivities. Many people with autoimmune conditions have unknown sensitivities to certain foods, making symptoms worse.
- Common Trigger Foods: Gluten, dairy, soy, and nightshades are often trigger foods that can cause bad reactions in some people.
- Elimination Diet Process: This means removing suspected trigger foods from your diet for 2-4 weeks. Then, you reintroduce them one at a time to see if you react.
By avoiding trigger foods, people can lessen their symptoms and live better lives.
Supplements That May Help Fight Autoimmune Responses
Along with diet changes, some supplements can help manage autoimmune diseases. These supplements can lower inflammation and balance the immune system.
- Omega-3 Fatty Acids: These have anti-inflammatory properties and can lessen the severity of autoimmune responses.
- Probiotics: Good bacteria that support gut health, probiotics are key for immune system regulation.
- Vitamin D: Many with autoimmune diseases have low vitamin D levels. Taking supplements can boost immune function.
Working with a Nutritionist for Personalized Plans
Creating a personalized nutritional plan with a registered dietitian or nutritionist is very helpful. They can tailor dietary advice based on your condition, health, and lifestyle.
A personalized plan might include specific dietary changes, supplement advice, and other nutritional strategies. This helps manage autoimmune diseases effectively.
Managing Flare-Ups: Strategies to Stop Autoimmune Disease Progression
Learning how to handle flare-ups is key to slowing down autoimmune diseases. Flare-ups happen when symptoms get worse. They can be caused by many things, like changes in the environment, stress, or some medicines. It’s important to manage these episodes well to keep a good quality of life and avoid lasting harm.
Identifying and Avoiding Triggers
One important way to manage flare-ups is to find and stay away from triggers. What triggers someone can vary a lot. It might be certain foods, things in the environment, or stress. Keeping a diary of symptoms can help figure out what triggers a person.
Once you know what triggers you, it’s important to avoid them. This could mean changing what you eat, like cutting out certain foods or eating an anti-inflammatory diet. It could also mean finding ways to handle stress, like through meditation or yoga.
Emergency Treatment Protocols
Having a plan for emergency treatment is very important for dealing with bad flare-ups. This plan should be made with a doctor and might include medicines to quickly reduce swelling and help with symptoms.
It’s also key for patients to know when to get help right away. If you have severe symptoms, like trouble breathing, a lot of pain, or big changes in how you see things, you need to get medical help fast.
| Symptom Severity | Recommended Action |
|---|---|
| Mild | Adjust medication as directed, monitor symptoms |
| Moderate | Contact healthcare provider for guidance, consider additional treatment |
| Severe | Seek immediate medical attention |
Recovery and Returning to Baseline
After a flare-up, the goal is to get back to a normal state of health. This means not just managing symptoms but also figuring out what caused the flare-up to prevent it from happening again.
Recovery might include rest, getting back into activities, and changing treatment plans. It’s also important to check in with your doctor to see if the treatment is working and make any needed changes.
For those who have had stem cell treatment, following the post-treatment advice is key for a good recovery and to lower the chance of flare-ups.
Emerging Treatments: The Future of Autoimmune Disease Management
The field of treating autoimmune diseases is changing fast. New treatments are being made to tackle the root causes of these conditions. This is thanks to ongoing research into autoimmune disorders.
mRNA Vaccine Technology
mRNA vaccine technology is getting a lot of attention. It has the power to treat many diseases, including autoimmune ones. These vaccines work with the body’s immune system to help it fight off diseases.
Key benefits of mRNA vaccine technology include:
- Flexibility in targeting specific antigens
- Potential for rapid development and adaptation
- Ability to induce immune responses without using live pathogens
Regulatory T Cell Therapies
Regulatory T cell (Treg) therapies are also showing promise. Treg cells help keep the immune system in balance. They prevent it from attacking the body’s own cells.
The power of Treg therapies lies in their ability to:
- Specifically target and modulate the immune response
- Provide long-term or even lifelong tolerance to self-antigens
- Offer a more personalized approach to treatment
Antigen-Specific Immunotherapies for Restoring Tolerance
Antigen-specific immunotherapies aim to teach the immune system to accept certain self-antigens. This helps correct the immune system’s mistakes that cause autoimmune diseases.
The benefits of these therapies include:
- Targeted treatment with potentially fewer side effects
- Potential for long-lasting or curative effects
- Ability to address the root cause of autoimmune diseases
Promising Research Directions
Research into autoimmune disease management is moving forward. New areas of study include combination therapies and gene editing. The role of the microbiome in autoimmunity is also being explored.
Healthcare providers are now at the forefront of these new treatments. This gives hope to those with autoimmune diseases. As these treatments improve, they could change how we manage autoimmune diseases and help patients live better lives.
Conclusion: Living Well While Managing Autoimmune Disorders
Managing autoimmune diseases needs a mix of medical care, lifestyle changes, and keeping up with new treatments. Knowing your condition, spotting early signs, and using treatments can help control the disease.
Living with autoimmune disorders means having a solid plan. It’s important to work with your doctor to create a treatment plan that fits you. This plan should include healthy eating, stress reduction, and specific treatments. Keeping current with new research and treatments is also key.
Handling autoimmune diseases is a journey that takes time. With the right medical care and lifestyle changes, you can live a full and happy life. We urge patients to be active in their care, seek help when needed, and stay informed about the latest in managing autoimmune diseases.
FAQ
What occurs when the immune system attacks the body?
When the immune system attacks the body, it mistakenly targets the body’s own tissues. This leads to inflammation and organ damage. It results in autoimmune disorders.
How to cure an autoimmune disease?
Autoimmune diseases are not curable. But, treatment aims to achieve remission. This means symptoms are significantly reduced or absent. Medical treatments and lifestyle modifications help achieve this.
What is it called when your body attacks itself?
When your body attacks itself, it is called an autoimmune disorder. The immune system mistakenly targets the body’s own tissues.
How to combat autoimmune disease?
Fighting autoimmune disease requires a full approach. This includes medical treatments like immunosuppressants and biologics. Lifestyle changes, such as anti-inflammatory diets and stress management, are also key.
What are the common symptoms of autoimmune disorders?
Symptoms of autoimmune disorders vary. But common ones include fatigue, joint pain, and skin rashes.
How to diagnose an autoimmune disorder?
Diagnosing an autoimmune disorder is complex. It involves blood tests for biomarkers, imaging studies for organ damage, and specialized tests to rule out other conditions.
What are the treatment options for autoimmune disorders?
Treatment options include immunosuppressant medications, corticosteroids, DMARDs, and targeted biologic therapies. These help manage symptoms, prevent flare-ups, and reduce organ damage.
Can autoimmune diseases be treated with lifestyle modifications alone?
Lifestyle modifications, like anti-inflammatory diets and stress management, are important. But, they are often used with medical treatments for the best results.
What is the role of nutritional interventions in managing autoimmune conditions?
Nutritional interventions, such as elimination diets and supplements, are vital. They reduce inflammation and improve immune responses in autoimmune conditions.
How to manage flare-ups and prevent autoimmune disease progression?
Managing flare-ups means identifying and avoiding triggers. Having emergency treatment plans and recovery strategies helps prevent disease progression.
What are the emerging treatments for autoimmune diseases?
New treatments include mRNA vaccine technology, regulatory T cell therapies, and antigen-specific immunotherapies. These aim to restore immune tolerance and reduce disease activity.
Are autoimmune diseases curable with emerging treatments?
Emerging treatments offer hope for managing autoimmune diseases. But, they are not yet proven to be curative. They aim to improve treatment outcomes and quality of life.
What occurs when the immune system attacks the body?
When the immune system attacks the body, it mistakenly targets the body’s own tissues. This leads to inflammation and organ damage. It results in autoimmune disorders.
How to cure an autoimmune disease?
Autoimmune diseases are not curable. But, treatment aims to achieve remission. This means symptoms are significantly reduced or absent. Medical treatments and lifestyle modifications help achieve this.
What is it called when your body attacks itself?
When your body attacks itself, it is called an autoimmune disorder. The immune system mistakenly targets the body’s own tissues.
How to combat autoimmune disease?
Fighting autoimmune disease requires a full approach. This includes medical treatments like immunosuppressants and biologics. Lifestyle changes, such as anti-inflammatory diets and stress management, are also key.
What are the common symptoms of autoimmune disorders?
Symptoms of autoimmune disorders vary. But common ones include fatigue, joint pain, and skin rashes.
How to diagnose an autoimmune disorder?
Diagnosing an autoimmune disorder is complex. It involves blood tests for biomarkers, imaging studies for organ damage, and specialized tests to rule out other conditions.
What are the treatment options for autoimmune disorders?
Treatment options include immunosuppressant medications, corticosteroids, DMARDs, and targeted biologic therapies. These help manage symptoms, prevent flare-ups, and reduce organ damage.
Can autoimmune diseases be treated with lifestyle modifications alone?
Lifestyle modifications, like anti-inflammatory diets and stress management, are important. But, they are often used with medical treatments for the best results.
What is the role of nutritional interventions in managing autoimmune conditions?
Nutritional interventions, such as elimination diets and supplements, are vital. They reduce inflammation and improve immune responses in autoimmune conditions.
How to manage flare-ups and prevent autoimmune disease progression?
Managing flare-ups means identifying and avoiding triggers. Having emergency treatment plans and recovery strategies helps prevent disease progression.
What are the emerging treatments for autoimmune diseases?
New treatments include mRNA vaccine technology, regulatory T cell therapies, and antigen-specific immunotherapies. These aim to restore immune tolerance and reduce disease activity.
Are autoimmune diseases curable with emerging treatments?
Emerging treatments offer hope for managing autoimmune diseases. But, they are not yet proven to be curative. They aim to improve treatment outcomes and quality of life.
References
Nature. Evolving understanding of autoimmune mechanisms and new therapeutic strategies of autoimmune disorders. https://www.nature.com/articles/s41392‑024‑01952‑8
National Center for Biotechnology Information (NCBI). Treating Human Autoimmunity: Current Practice and Future Prospects. https://pmc.ncbi.nlm.nih.gov/articles/PMC4061980/
Autoimmune Institute. The spectrum of autoimmune disease treatments. https://www.autoimmuneinstitute.org/the-spectrum-of-autoimmune-disease-treatments/
American Academy of Allergy, Asthma & Immunology (AAAAI). Immunosuppressive Medication for the Treatment of Autoimmune Disease. https://www.aaaai.org/conditions-treatments/related-conditions/immunosuppressive