Last Updated on November 20, 2025 by Ugurkan Demir

Aplastic crisis in sickle cell disease is a serious problem. It can be very dangerous if not caught early. We know how critical it is to manage it well and fast.
At Liv Hospital, we aim to give top-notch healthcare. We support international patients fully. Our team works hard to find the best crisis management plans.
Knowing how aplastic crisis works is key to handling it right. Our article will share important facts. We’ll talk about what causes it, its signs, and how to treat it.
Key Takeaways
- Understanding the severity of aplastic crisis in sickle cell disease
- Importance of timely recognition and management
- Overview of the pathophysiology of the condition
- Effective crisis management strategies
- Comprehensive support for international patients
The Fundamentals of Sickle Cell Anemia
To understand sickle cell anemia, we must look at its genetic roots and how it affects red blood cells. It’s a complex genetic disorder that messes with hemoglobin production. This leads to several health issues.
Genetic Basis and Inheritance Patterns
Sickle cell anemia comes from a specific mutation in the beta-globin chain of hemoglobin. This mutation creates abnormal hemoglobin S (HbS). It’s inherited in an autosomal recessive pattern. This means you need two copies of the mutated gene, one from each parent, to have the disease.
Carriers have one normal and one mutated gene. They usually don’t show all the disease symptoms. But they can pass the mutated gene to their children.
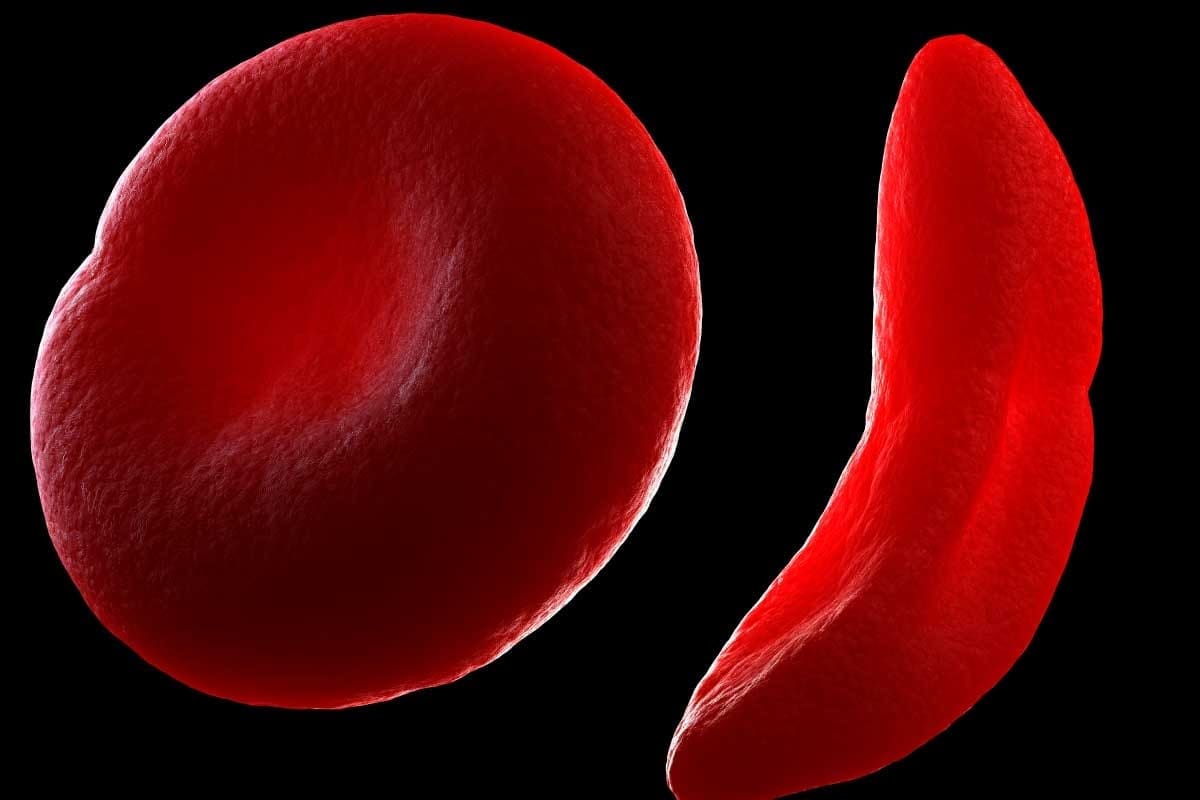
Abnormal Hemoglobin and Red Blood Cell Sickling
The HbS causes red blood cells to take on a sickle shape under low oxygen conditions. At first, this shape can change back. But repeated changes lead to cell damage over time.
This abnormal hemoglobin changes the shape and function of red blood cells. It also shortens their lifespan. This contributes to the many problems seen in sickle cell anemia, like vaso-occlusive crises.
Aplastic Crisis in Sickle Cell Anaemia: Definition and Mechanism

Aplastic crisis in sickle cell anemia is a serious issue. It happens when the bone marrow stops making new red blood cells. This leads to a big drop in red blood cell production.
Temporary Bone Marrow Suppression
The bone marrow stops working well in an aplastic crisis. This makes it hard for the body to make new blood cells. The red blood cell count drops fast, making anemia worse and leading to serious problems.
Parvovirus B19 as the Primary Trigger
Parvovirus B19 is the main cause of aplastic crisis in sickle cell anemia. It attacks the bone marrow, stopping it from making red blood cells. This can cause a sudden and severe anemia, needing quick medical help.
Rapid Decline in Red Blood Cell Production
The fast drop in red blood cells during an aplastic crisis is very dangerous. It can cause tiredness, pale skin, and shortness of breath. Quick diagnosis and treatment are key to managing this condition.
| Characteristics | Aplastic Crisis | Vaso-Occlusive Crisis |
| Cause | Parvovirus B19 Infection | Sickling of Red Blood Cells |
| Primary Effect | Temporary Bone Marrow Suppression | Blood Vessel Blockage |
| Clinical Presentation | Severe Anemia, Fatigue | Acute Pain Episodes |
Vaso-Occlusive Crisis: The Most Common Sickle Cell Emergency
Vaso-occlusive crisis is a major problem in sickle cell disease. It happens when sickled red blood cells block blood vessels. This leads to pain and tissue damage because of reduced blood flow.
We will look into how this blockage happens. We’ll also talk about the symptoms and what can trigger these crises.
Mechanism of Blood Vessel Blockage
The crisis starts when sickled red blood cells block blood vessels. This cuts off blood flow to the area. It can cause tissue damage and pain.
The cells become rigid and stick to blood vessel walls. This is because of a change in hemoglobin S. It makes the cells stiff and causes blockages.
Clinical Presentation of Acute Pain Episodes
Pain crises are the main sign of vaso-occlusive crises. The pain is often severe and in specific areas like the back, chest, or limbs.
Patients might also have fever, swelling, and tenderness. These symptoms are in the affected area.
Common Triggers and Risk Factors
Several things can set off a vaso-occlusive crisis. These include dehydration, infections, cold weather, and stress. Knowing and managing these can help prevent crises.
| Trigger/Risk Factor | Description |
| Dehydration | Reduces blood volume, increasing blood viscosity and the likelihood of vaso-occlusion |
| Infection | Can cause inflammation and increase the risk of vaso-occlusive crisis |
| Cold Weather | Causes vasoconstriction, which can trigger a vaso-occlusive crisis |
| Stress | Can exacerbate the condition by potentially causing dehydration and other physiological changes |
Knowing about these triggers and risk factors helps manage and prevent vaso-occlusive crises. This is important for patients with sickle cell disease.
Comparing Different Types of Sickle Cell Crises
It’s important to know the different types of sickle cell crises to manage them well. Sickle cell disease has many acute crises that can really affect a patient’s life.
We’ll look at the sequestration crisis, hemolytic crisis, and acute chest syndrome. We’ll see what makes each one unique and why it’s key to know the difference for the right treatment.
Sequestration Crisis Characteristics
A sequestration crisis happens when a lot of blood gets stuck in the spleen or liver. This leads to a sudden drop in hemoglobin levels. It’s very dangerous because it can cause severe anemia and not enough blood volume.
Key Features:
- Splenic or hepatic enlargement
- Severe anemia
- Hypovolemia
Hemolytic Crisis Features
A hemolytic crisis is when red blood cells break down fast, causing a quick drop in hemoglobin. It can be caused by infections or certain medicines.
Notable Characteristics:
- Rapid decline in hemoglobin
- Jaundice
- Potential for severe anemia
Acute Chest Syndrome Presentation
Acute chest syndrome is a serious problem in sickle cell disease. It shows chest pain, cough, and trouble breathing. It also has new spots on the lungs seen on X-rays.
Clinical Features:
- Chest pain
- Respiratory distress
- New pulmonary infiltrates on chest X-ray
Here’s a table that shows the main differences between these crises:
| Crisis Type | Primary Characteristics | Key Symptoms |
| Sequestration Crisis | Splenic or hepatic enlargement, severe anemia | Abdominal pain, fatigue, pallor |
| Hemolytic Crisis | Rapid decline in hemoglobin, jaundice | Fatigue, yellowing of skin, dark urine |
| Acute Chest Syndrome | Chest pain, respiratory distress, and new pulmonary infiltrates | Cough, difficulty breathing, chest pain |
Knowing the unique traits of each crisis helps doctors give better care. This can lead to better results for patients.
Sickle Cell Crisis Pathophysiology: From Molecular Changes to Clinical Symptoms
Sickle cell crisis is a complex process that affects many parts of the body. It starts with the polymerization of hemoglobin S. This leads to a series of events that cause the crisis symptoms.
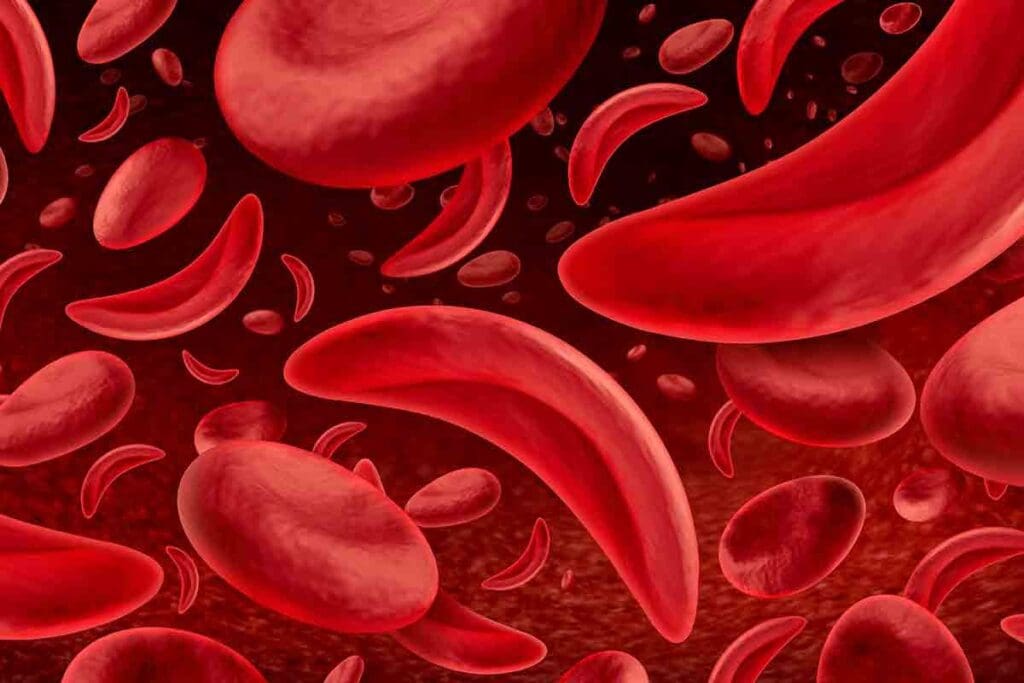
Hemoglobin S Polymerization Process
The polymerization of hemoglobin S is key in sickle cell crisis. When it’s deoxygenated, hemoglobin S changes shape and forms polymers. These polymers make the red blood cells sickle-shaped.
At first, the sickling of red blood cells can be reversed. But repeated cycles cause damage and make the sickling permanent. The speed and amount of polymerization depend on several factors, like the amount of hemoglobin S and oxygen levels.
Cellular Adhesion and Vascular Damage
Sickled red blood cells stick more to the blood vessel walls, causing blockages. This is because of adhesion molecules on both the cells and the vessel walls. This sticking damages the blood vessels and makes them more prone to inflammation and clotting.
These blockages also lead to tissue damage and infarctions. This damage worsens the blood vessel problems. It’s a big part of why sickle cell disease is so serious.
Inflammatory Response and Tissue Injury
The inflammatory response is very important in a sickle cell crisis. Sickled cells and damaged blood vessel walls release inflammatory cytokines. This makes the inflammation worse and causes more tissue damage.
This inflammation creates a cycle of more blockages and damage. It’s a vicious cycle that makes the crisis worse.
| Pathophysiological Mechanism | Clinical Consequence |
| Hemoglobin S Polymerization | Sickling of Red Blood Cells |
| Cellular Adhesion | Vaso-occlusion and Ischemia |
| Inflammatory Response | Tissue Injury and Organ Damage |
Critical Laboratory Findings in Sickle Cell Crises
Diagnosing sickle cell crises relies on specific lab tests. These tests give vital information to doctors. They help in diagnosing and managing these crises well.
Complete Blood Count Abnormalities
A complete blood count (CBC) is key in diagnosing sickle cell crises. It shows signs like anemia, a common sign of sickle cell disease. The CBC shows low hemoglobin and high reticulocyte counts, showing the bone marrow’s effort to fight anemia.
We look at CBC results to see how severe anemia is. A big drop in hemoglobin or a high reticulocyte count can mean a crisis or a complication like aplastic crisis.
| Parameter | Normal Range | Typical Findings in Sickle Cell Crisis |
| Hemoglobin (g/dL) | 13.8-17.2 (male) | Often decreased, sometimes severely |
| Reticulocyte Count (%) | 0.5-1.5 | Usually elevated, indicating a bone marrow response |
| White Blood Cell Count (x10^9/L) | 4.5-11 | May be elevated due to stress response or infection |
Reticulocyte Count as a Diagnostic Clue
The reticulocyte count is a key part of the CBC. It shows if the bone marrow is making new red blood cells. In sickle cell disease, a high count means the bone marrow is working hard to replace lost red blood cells.
A low reticulocyte count with severe anemia might mean an aplastic crisis. This is when the bone marrow stops making red blood cells. But a high count means the bone marrow is doing its job to fight anemia.
Blood Smear Examination Results
A blood smear gives us information on red and white blood cells and platelets. In sickle cell crises, it shows sickled red blood cells. These are clear signs of the disease.
We look at the blood smear for other signs, like Howell-Jolly bodies. These show if the spleen is not working properly, which is common in sickle cell disease. Finding these signs helps us understand how severe the disease is and its effect on the spleen.
Early Recognition of Aplastic Crisis: Warning Signs and Symptoms
Knowing the warning signs and symptoms of aplastic crisis can greatly help patients with sickle cell disease. Aplastic crisis is a serious issue where the bone marrow stops making red blood cells. It often happens because of parvovirus B19 infection.
Progressive Fatigue and Pallor
Progressive fatigue is a major symptom of aplastic crisis. Patients feel extremely weak and tired, even after resting. They also show pallor, or pale skin, because of fewer red blood cells. These symptoms can appear quickly, sometimes in just a few days.
Cardiovascular Manifestations
Aplastic crisis can cause cardiovascular manifestations like tachycardia (rapid heart rate) and shortness of breath. With fewer red blood cells, the heart has to work harder. This can lead to heart palpitations and other heart problems. Patients might also feel dizzy or lightheaded because of less oxygen to the tissues.
Distinguishing Features from Other Crises
It’s important to tell an aplastic crisis apart from other sickle cell crises. Unlike vaso-occlusive crises, which cause pain from blocked blood vessels, an aplastic crisis is marked by a big drop in red blood cell production. A low reticulocyte count is a key sign, showing the bone marrow can’t make new red blood cells.
Spotting these warning signs early lets healthcare providers start treatment quickly. This can help improve patient outcomes. We stress the need for close monitoring and quick medical help if symptoms get worse or if there’s severe anemia.
Comprehensive Sickle Cell Crisis Management Protocol
Managing a sickle cell crisis needs a detailed plan. This plan should tackle the condition’s complex nature. Healthcare providers can use this protocol to better care for patients.
Initial Assessment and Stabilization
When a patient has a sickle cell crisis, a thorough check-up is key. This includes looking at their medical history and doing a physical exam. It helps figure out the crisis type and what might have caused it.
Quickly checking the patient’s airway, breathing, and circulation (ABCs) is also vital. Recent guidelines suggest starting with oxygen, hydration, and pain relief.
Key steps in the initial check-up are:
- Vital sign measurement
- Physical examination
- Laboratory tests (e.g., complete blood count, reticulocyte count)
Pain Management Strategies
Managing pain is a big part of caring for sickle cell crisis patients. We suggest using a mix of medicines and other methods. Opioid analgesics might be needed for severe pain, but we must watch for addiction risks.
| Pain Management Strategy | Description |
| Opioid Analgesics | Used for severe pain management, with careful monitoring for side effects |
| Non-Opioid Analgesics | Used for mild to moderate pain or in conjunction with opioids |
| Non-Pharmacological Interventions | Includes relaxation techniques, heat or cold therapy, and distraction methods |
Hydration and Electrolyte Balance
Keeping well-hydrated is key to managing a sickle cell crisis. It helps blood flow better and lowers sickled red blood cells. We use intravenous fluids to keep hydration and electrolyte balance right. It’s important to watch electrolyte levels to avoid problems.
Oxygen Therapy Guidelines
Oxygen therapy is vital, mainly for those with acute chest syndrome or severe anemia. We give oxygen to keep oxygen levels high, as checked by pulse oximetry.
By sticking to this detailed management plan, healthcare providers can help patients with sickle cell crises more effectively. It’s all about a detailed approach to meet these complex needs.
Special Management Considerations for Aplastic Crisis
Aplastic crisis is a serious problem for people with sickle cell disease. It happens when the bone marrow can’t make enough red blood cells. This leads to a quick drop in hemoglobin levels.
Urgent Transfusion Protocols
One key way to manage aplastic crisis is through urgent transfusions. Red blood cell transfusions help keep hemoglobin levels stable. This ensures tissues get enough oxygen.
We start thinking about transfusions when hemoglobin levels get too low. Or when the heart shows signs of trouble.
The goal of transfusions is to treat anemia and stop sickle-cell hemoglobin production. This reduces the risk of more problems. Choosing the right blood products and transfusion rate is important to avoid issues like hyperviscosity.
Infection Control Measures
Keeping infections at bay is vital in managing aplastic crisis. People with sickle cell disease are more prone to infections. This risk gets even higher during an aplastic crisis because the bone marrow isn’t working properly.
We stress the need for strict infection control measures. This includes using the right antibiotics and vaccines. Watching for infection signs and starting antibiotics quickly is key.
Monitoring for Complications
It’s important to watch closely for any complications. We check hemoglobin levels, reticulocyte count, and overall health regularly. We also look out for heart problems and acute chest syndrome.
Using continuous cardiac monitoring and other tools helps us catch and treat problems fast.
Hospital Admission Criteria
Because aplastic crisis is so serious, hospital care is often needed. We admit patients with severe anemia, heart issues, or other big problems.
In the hospital, a team of doctors and nurses works together. They include hematologists and intensive care specialists. This team provides the best care possible.
Prevention Strategies and Long-term Care
Preventing sickle cell disease crises is key. Long-term care includes medication, lifestyle changes, and regular doctor visits.
Benefits of Hydroxyurea Therapy
Hydroxyurea helps reduce painful crises and may cut down on blood transfusions. It boosts fetal hemoglobin production, helping red blood cells not to sickle. This improves life quality for those with sickle cell disease.
Hydroxyurea therapy offers several benefits:
- Less frequent painful crises
- Lower need for blood transfusions
- Longer survival
Vaccination Recommendations
Vaccines are vital to prevent infections that can cause sickle cell crises. People with sickle cell disease are more at risk of infections because their immune systems are weak. Stick to this vaccination schedule:
- Pneumococcal conjugate vaccine (PCV)
- Pneumococcal polysaccharide vaccine (PPSV)
- Meningococcal conjugate vaccine
- Haemophilus influenzae type b (Hib) vaccine
Regular Monitoring Schedule
Regular checks are vital for managing sickle cell disease. This includes:
- Regular blood tests to check hemoglobin and detect anemia or infection
- Checking organ function, like the spleen and kidneys
- Keeping an eye on overall health and adjusting treatment as needed
Patient Education and Self-Care
Teaching patients about their disease and involving them in care is key. They should know the crisis signs and when to get medical help. Self-care includes:
- Drinking plenty of water
- Avoiding extreme temperatures
- Managing stress
- Keeping a healthy lifestyle with diet and exercise
By using these prevention and care strategies, people with sickle cell disease can live better lives.
Emerging Treatments and Future Directions
New treatments are changing how we manage sickle cell disease. These advancements could lead to better care for those affected. Patients might see improvements in their health and quality of life.
Novel Pharmaceutical Agents
New drugs are being developed to tackle sickle cell disease from different angles. Some aim to reduce painful crises and may even help patients live longer.
Key Developments:
- Voxelotor increases hemoglobin’s oxygen affinity, reducing sickling.
- Crizanlizumab, a monoclonal antibody, cuts down vaso-occlusive crises.
These breakthroughs are major steps forward. They offer patients more effective ways to manage their condition.
Gene Therapy Approaches
Gene therapy could be a game-changer for sickle cell disease. It aims to fix the genetic issue causing the disease, aiming for normal hemoglobin production.
“Gene therapy has the power to change sickle cell disease treatment by tackling the disease’s root cause.”
–Hematologist
Gene editing tools like CRISPR/Cas9 are showing promise in early trials. This opens doors for more research and development.
Stem Cell Transplantation Advances
Stem cell transplantation is a rare cure for sickle cell disease. Efforts are being made to make it safer and more effective.
| Treatment | Description | Potential Benefits |
| Gene Therapy | Corrects the genetic mutation causing sickle cell disease | Potential cure, eliminates disease symptoms |
| Stem Cell Transplantation | Replaces the patient’s bone marrow with healthy donor cells | Curative reduces the risk of complications |
| Novel Pharmaceutical Agents | Reduces frequency of painful crises and improves survival | Improved quality of life, reduced healthcare utilization |
As research keeps moving forward, we expect these new treatments to greatly improve sickle cell disease management. This brings hope to patients and their families.
Conclusion: Improving Outcomes Through Early Intervention and Comprehensive Care
Managing sickle cell disease well needs a team effort. It’s all about starting early and giving full care. This way, we can make life better for those with the disease.
Starting early is key to handling sickle cell crises. This includes types like aplastic and vaso-occlusive crises. Full care means managing pain, staying hydrated, and controlling infections.
We all play a part in bettering sickle cell disease care. Healthcare teams, patients, and families must work together. This way, we can create care plans that fit each person’s needs.
Research and new medical ways are helping us improve sickle cell disease care. We must keep focusing on early action and full care. This will help patients get the best results.
FAQ
What is a sickle cell crisis?
A sickle cell crisis is a painful episode for those with sickle cell disease. It can be triggered by dehydration, infection, or extreme temperatures.
What are the different types of sickle cell crises?
There are several types of sickle cell crises. These include vaso-occlusive, aplastic, sequestration, and hemolytic crises. Each has its own characteristics and symptoms.
What is an aplastic crisis in sickle cell disease?
An aplastic crisis happens when the bone marrow stops making red blood cells. It’s often caused by parvovirus B19 infection. This leads to severe anemia.
How is a vaso-occlusive crisis managed?
Managing vaso-occlusive crisis involves pain relief and hydration. Oxygen therapy is also used. The goal is to ease symptoms and prevent further complications.
What is the role of hydroxyurea in sickle cell disease management?
Hydroxyurea is a medication that can reduce the frequency and severity of sickle cell crises. It increases fetal hemoglobin production, which helps prevent red blood cell sickling.
What laboratory tests are critical for diagnosing sickle cell crises?
Important tests include complete blood count, reticulocyte count, and blood smear examination. These help diagnose and differentiate between various types of sickle cell crises.
How can an aplastic crisis be distinguished from other types of sickle cell crises?
Aplastic crisis is marked by a significant drop in reticulocyte count and severe anemia. This distinguishes it from other crises, which have different laboratory findings and symptoms.
What are the warning signs of an impending aplastic crisis?
Warning signs include progressive fatigue, pallor, and cardiovascular symptoms. These indicate a possible aplastic crisis that needs immediate medical attention.
What are the emerging treatments for sickle cell disease?
New treatments include novel pharmaceuticals, gene therapy, and stem cell transplantation. These offer promising options for managing sickle cell disease.
How can patients with sickle cell disease prevent crises?
Prevention involves staying hydrated, avoiding extreme temperatures, and getting vaccinated. Adhering to prescribed medications like hydroxyurea is also key.
What is the importance of patient education in sickle cell disease management?
Patient education is vital. It empowers individuals to manage their condition, recognize early warning signs, and follow treatment plans.
References:
- Gliklich, R. E., & Stellingwerf, L. (2022). Clinical and laboratory features of aplastic crisis in sickle cell disease patients infected with parvovirus B19. Blood Advances, 6(12), 3751–3759.https://ashpublications.org/bloodadvances/article/6/12/3751/492625