Last Updated on November 20, 2025 by Ugurkan Demir
We are dedicated to giving top-notch care to those with Pre-B ALL Leukemia. This disease is marked by the growth of immature B-cell precursors in the bone marrow.Learn 7 key pre B ALL leukemia facts. Understand Precursor B-Cell Acute Lymphoblastic Leukemia, a serious and powerful blood cancer.
Pre-B ALL Leukemia is the leading type of ALL in kids, but it can also hit adults. Knowing the important facts about it is key to spotting and treating it right.
In this piece, we’ll share 7 key facts about Pre-B ALL Leukemia. We aim to give a full picture of the disease and how to manage it. Our goal is to help patients and their families understand this tough illness better.
Key Takeaways
- Pre-B ALL Leukemia is a type of cancer that affects the blood and bone marrow.
- It is the most common subtype of ALL in children.
- Pre-B ALL Leukemia can also occur in adults.
- Effective diagnosis and treatment require a thorough grasp of the condition.
- Leading institutions like Liv Hospital are setting new standards in patient-centered care for Pre-B ALL Leukemia.
What Is Pre-B ALL Leukemia? Definition and Classification

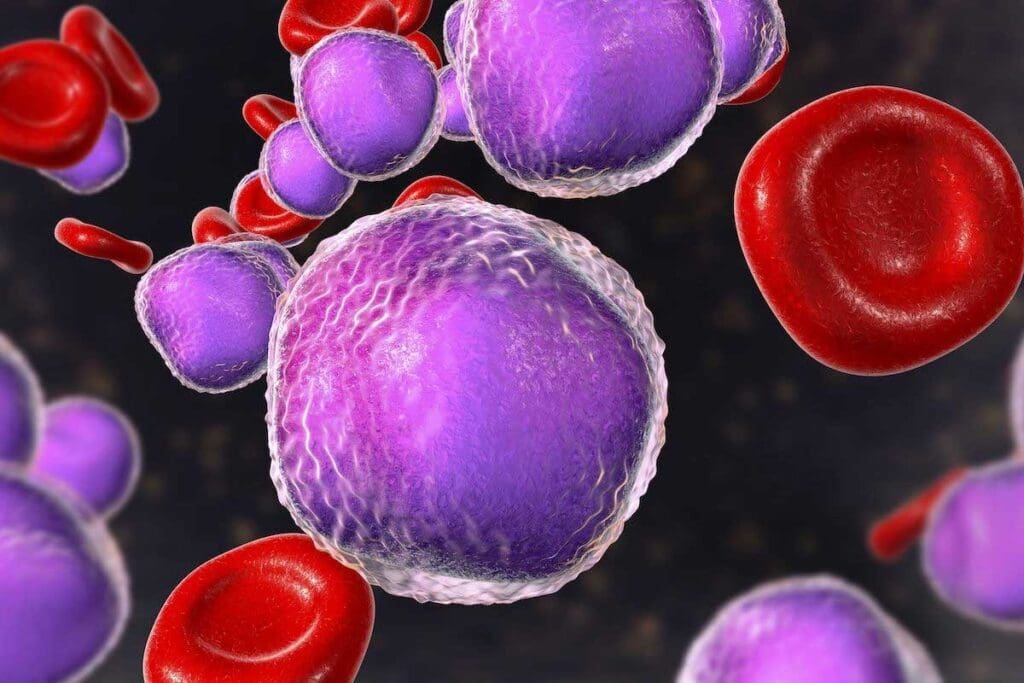
Pre-B cell Acute Lymphoblastic Leukemia (ALL) is a cancer that stops the bone marrow from making normal blood cells. It happens when immature B-cell precursors, called lymphoblasts, grow too much in the bone marrow. This blocks the production of healthy blood cells.
The Fundamentals of Pre-B Cell Development
Pre-B cells are the early stages of B cells, which are key to our immune system. They help fight off infections by making antibodies. Normally, pre-B cells grow in the bone marrow, going through stages to become full B cells. But if this process goes wrong, it can cause leukemia.
The growth of pre-B cells involves many steps, like rearranging genes and showing specific surface markers. These steps are carefully controlled to keep our immune system working properly.
How Pre-B ALL Differs From Other Leukemia Types
Pre-B ALL stands out because of its unique markers and genetic traits. Unlike other leukemias, Pre B ALL has lymphoblasts with specific B-cell markers.
| Characteristics | Pre B ALL | Other Leukemia Types |
| Cell Origin | B-cell precursors | Varies (T-cell, myeloid, etc.) |
| Immunophenotype | B-cell markers (CD19, CD22) | Different markers based on lineage |
| Genetic Abnormalities | Specific translocations (e.g., BCR-ABL) | Varies by leukemia type |
Knowing these differences is key to diagnosing and treating Pre-B ALL right. The unique traits of Pre-B ALL help doctors decide on treatments and predict how well patients will do.
The Biology Behind Pre-B ALL Leukemia
To understand Pre B ALL leukemia, we must first learn about B-cells. B-cells are key to our immune system, making antibodies to fight off infections. They start in the bone marrow and grow into mature B-cells in our blood and lymphoid tissues.
Normal B-Cell Development Process
B-cell development starts in the bone marrow. It involves several steps, from pro-B cells to mature B-cells. This process is controlled by genetics and molecular events. Any disruption can cause leukemia.
Cellular and Molecular Abnormalities
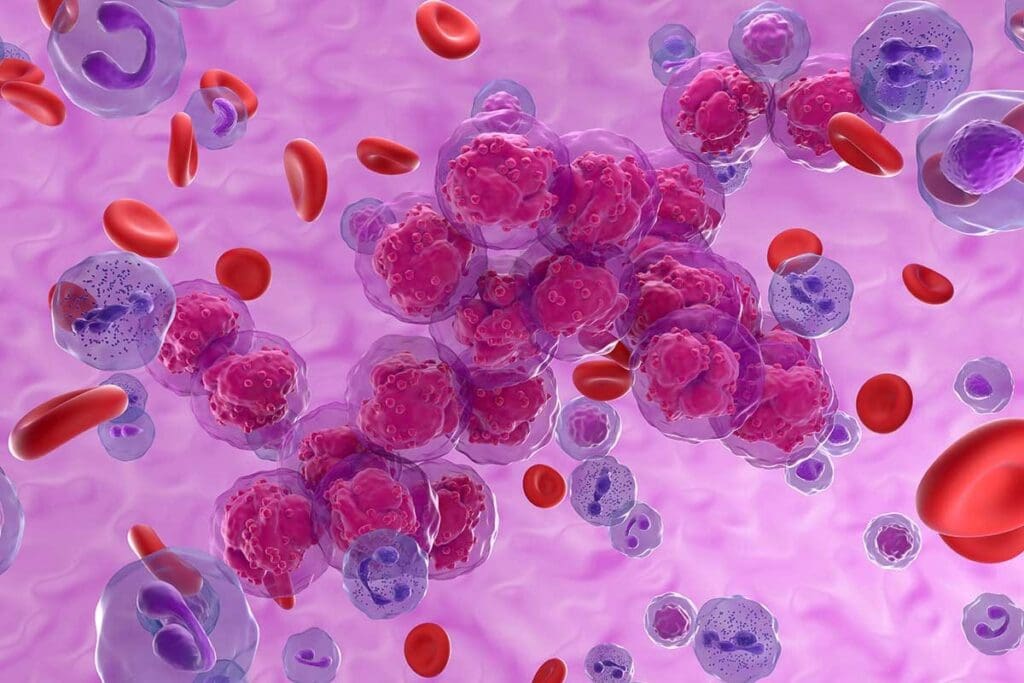
In Pre-B ALL leukemia, cells and molecules go wrong. This includes genetic mutations and changes in chromosomes. These issues stop normal B-cell growth, causing cancer cells to grow too much. Studies show that genetic changes play a big role in Pre B ALL leukemia.
How Malignant Transformation Occurs
Leukemia turns malignant when cells undergo genetic or chromosomal changes. These changes let cancer cells grow more than normal cells. A top leukemia researcher says,
“The genetic alterations in B-cell precursor ALL are diverse and have significant implications for disease biology and treatment.”
Knowing this helps us create better treatments.
By studying Pre-B ALL leukemia, we can tackle its complexities. This is key to making treatments that really work.
Epidemiology: Pre-B ALL’s Impact Across Age Groups
Studies show that Pre-B ALL affects people differently by age. Knowing this helps us understand its big impact.
Childhood Prevalence: The Majority
Pre-B cell ALL leukemia is the main type of ALL in kids. It makes up about 75 to 80 percent of cases. It hits kids most between 2 and 5 years old.
| Age Group | Prevalence of Pre-B ALL |
| 0-1 year | Low |
| 2-5 years | High (peak incidence) |
| 6-10 years | Moderate |
| Adults | Lower than in children |
Adult Cases: Differences in Presentation and Risk Factors
In adults, Pre-B ALL is less common. It shows up differently and has unique risk factors. Adults face a tougher fight because of health issues and the disease’s nature.
Key differences in adult Pre-B ALL include:
- Lower incidence compared to children
- Different genetic mutations
- Higher risk of treatment-related complications
Genetic Factors Driving Pre-B Acute Lymphoblastic Leukemia
Pre-B Acute Lymphoblastic Leukemia is caused by many genetic changes. These changes affect B-cells’ development and function. This leads to leukemia.
Key Genetic Mutations and Chromosomal Abnormalities
Several genetic mutations and chromosomal abnormalities are linked to Pre-B ALL. These include:
- ETV6-RUNX1 fusion: This genetic abnormality is common in pediatric Pre B ALL. It comes from a chromosomal translocation.
- Hyperdiploidy: This means cells have more than 50 chromosomes. It’s often seen in children and has a good prognosis.
- Hypodiploidy: Cells have fewer than 44 chromosomes. This is linked to a poorer prognosis.
- MLL gene rearrangements are more common in infant leukemia. It’s associated with a poor outcome.
- BCR-ABL1 fusion: Also known as the Philadelphia chromosome. This abnormality is more common in adult Pre-B ALL.
These genetic changes can be found through tests like cytogenetic analysis and molecular diagnostics.
How Genetics Influences Treatment Decisions and Outcomes
The genetic makeup of Pre-B ALL greatly affects treatment choices and outcomes. For example:
| Genetic Abnormality | Treatment Approach | Prognosis |
| ETV6-RUNX1 fusion | Standard chemotherapy | Favorable |
| Hyperdiploidy | Standard chemotherapy | Favorable |
| BCR-ABL1 fusion | Tyrosine kinase inhibitors + chemotherapy | Improved with targeted therapy |
| MLL gene rearrangements | Intensive chemotherapy | Poor |
Understanding the genetic factors behind Pre-B ALL is key to better treatment plans. As research grows, using genetic information in treatment is becoming more important.
Recognizing Pre-B ALL Symptoms and Warning Signs
It’s important to know the symptoms of Pre-B ALL leukemia early. This helps in getting the right treatment fast. We’ll list the common signs and symptoms to help you spot them.
Primary Symptoms: Fatigue, Bruising, and Infections
People with Pre-B ALL leukemia often feel very tired, bruise easily, and get sick a lot. Feeling tired a lot is because of not enough red blood cells. Easy bruising happens when there are not enough platelets, making it hard to stop bleeding.
Getting sick often is because leukemia cells take over the healthy white blood cells. This weakens the immune system.
Secondary Symptoms: Bone Pain and Lymph Node Swelling
Some people might also feel pain in their bones or have swollen lymph nodes. Bone pain happens when leukemia cells build up in the bone marrow. This makes it hurt.
Lymph node swelling means the leukemia is affecting the lymphatic system. This is a sign that something is wrong.
Emergency Warning Signs Requiring Immediate Care
Some symptoms need to be seen by a doctor right away. These include severe bleeding, trouble breathing, or high fever. If you see any of these, get help fast.
Spotting these symptoms early can really help in treating Pre B ALL leukemia. If you’re feeling any of these, talk to a doctor right away.
Diagnostic Journey for Pre-B Cell Acute Lymphocytic Leukemia
To diagnose Pre B Cell Acute Lymphocytic Leukemia, doctors use several steps. They start with initial screenings and then move to more detailed tests. This careful process helps find the exact cause of the disease. It’s key to creating a good treatment plan.
Initial Blood Work and Physical Examination
The first step is a physical check-up and blood tests. Doctors look for signs like swollen lymph nodes and pale skin. They also do blood tests to see if there are too many or too few blood cells.
- A CBC can show if there’s anemia or too many white blood cells, which might mean leukemia.
- Blood smears help find any odd cells.
Bone Marrow Biopsy: The Definitive Diagnostic Test
A bone marrow biopsy is the main test for Pre-B ALL. It takes a sample from the hip bone for a close look.
Key findings from a bone marrow biopsy include:
- Seeing lots of lymphoblasts means it’s acute lymphoblastic leukemia.
- Immunophenotyping shows the leukemia cells are B-cell precursors.
Advanced Diagnostic Methods: Flow Cytometry and Genetic Analysis
More advanced tests are important for confirming the diagnosis and learning about Pre-B ALL.
Flow cytometry checks the proteins on leukemia cells. It helps find markers for Pre-B ALL. Genetic tests look for chromosomal and genetic changes. This info helps predict the disease’s course and find treatment options.
Some key genetic analyses include:
- FISH (Fluorescence In Situ Hybridization) to find genetic problems.
- PCR (Polymerase Chain Reaction) to spot specific genetic changes.
Comprehensive Treatment Approaches for Pre-B ALL Cancer
Pre-B ALL cancer treatment uses many therapies together for the best results. The plan is made just for each patient. It considers their age, health, and the leukemia’s genetic details.
Standard Chemotherapy Protocols and Phases
Chemotherapy is key in treating Pre-B cell acute lymphoblastic leukemia. The treatment has several stages: induction, consolidation, and maintenance. The goal of the first phase is to get rid of leukemia cells in the bone marrow.
The next phase, consolidation, aims to kill any cancer cells left. Maintenance therapy is then used to keep the cancer from coming back. This phase can last from months to years.
The type of chemotherapy used can change based on the patient’s risk level and how well they respond. High-risk patients might need stronger treatments.
Targeted Therapies: Monoclonal Antibodies and Small Molecules
Targeted therapies are also important in treating Pre-B ALL cancer. Monoclonal antibodies, like blinatumomab, target proteins on leukemia cells. This helps get rid of them. Small molecule inhibitors, such as tyrosine kinase inhibitors, block cancer growth by stopping certain molecular pathways.
- Monoclonal antibodies: Blinatumomab, rituximab
- Small molecule inhibitors: Tyrosine kinase inhibitors
Stem Cell Transplantation: When and Why It’s Recommended
Stem cell transplantation, or bone marrow transplantation, is for high-risk Pre B cell lymphoblastic leukemia patients or those who have had a relapse. It replaces the patient’s bad bone marrow with healthy stem cells. These can come from a donor or the patient themselves.
The choice to do a stem cell transplant depends on many things. These include the patient’s health, how well they’ve responded to treatment, and the leukemia’s genetic makeup.
By using all these treatments together, we can give patients with Pre-B acute lymphocytic leukemia a detailed and tailored plan. This helps them have a better chance of long-term remission and survival.
Revolutionary CAR T-Cell Therapy for Pre-B Cell Lymphoblastic Leukemia
Pre-B-cell ALL leukemia treatment has seen a big change with CAR T-cell therapy. This new approach uses the body’s immune system to fight cancer. It’s a big step forward in fighting this disease.
The Science Behind CAR T-Cell Engineering
CAR T-cell therapy starts by taking T-cells from a patient’s blood. Then, these T-cells are changed to find and attack cancer cells. This way, T-cells can target Pre B cell lymphoblastic leukemia cells exactly, making treatment more precise.
The change involves adding a special receptor to the T-cells. This receptor lets them see a specific antigen on leukemia cells. This targeted method helps avoid harming healthy cells, reducing side effects seen with old treatments.
Patient Selection Criteria and Real-World Outcomes
Not every patient can get CAR T-cell therapy. Only those with certain biomarkers and good health qualify. Studies have shown good results, with many patients getting better.
Real-world results are also positive. CAR T-cell therapy is changing how we treat Pre-B cell ALL leukemia. More research is needed to make it even better and safer.
Managing Treatment Side Effects and Long-Term Complications
Handling the side effects of Pre-B ALL treatment is key. Patients with Pre-B Cell Acute Lymphoblastic Leukemia face many side effects. These can be short-term or last a long time.
Acute Side Effects and Their Management
Side effects of Pre-B ALL treatment include fatigue, nausea, hair loss, and increased risk of infections. Doctors use medicines and supportive care to help. For example, antiemetic drugs fight nausea, and G-CSF lowers infection risk.
Long-Term Health Considerations for Survivors
Survivors of Pre-B ALL might deal with long-term health issues. These include cardiotoxicity, secondary malignancies, and endocrine disorders. Regular check-ups are vital to watch for and manage these problems. This means heart checks, cancer screenings, and hormone tests.
Understanding and tackling both short-term and long-term effects of Pre-B ALL treatment helps survivors live better lives.
Prognosis Factors and Survival Rates in Pre-B ALL Patients
Pre-B ALL’s outcome depends on several factors. These include age, genetic changes, and how well the patient responds to treatment. Knowing these factors helps doctors choose the best treatment and predict how well a patient will do.
Key Prognostic Indicators: Age, Genetics, and Response to Treatment
Several important factors affect Pre-B ALL patients’ outcomes. Age is a big one, with kids usually doing better than adults. Genetic mutations, like the Philadelphia chromosome, also play a big role. How well a patient responds to treatment is another key indicator of survival.
Current Survival Statistics Across Different Demographics
Survival rates for Pre-B ALL have gotten much better over time. Thanks to new treatments, kids with Pre-B ALL now have a 90% 5-year survival rate. For adults, the rate is between 30% and 50%, depending on several factors.
Relapse Risks and Second Remission Possibilities
Even with good initial results, relapse is a big worry, mainly for high-risk patients. The chance of getting a second remission depends on how long the first remission lasted and genetic mutations. Knowing these risks helps doctors plan better follow-up care.
Conclusion: Navigating Life After Pre-B ALL Diagnosis
Life after a Pre-B ALL diagnosis needs a lot of support and guidance. Pre-B Cell Acute Lymphoblastic Leukemia, or Pre-B ALL, is a serious condition. It affects not just the patient but also their loved ones.
Pre-B ALL causes abnormal growth of precursor B cells. This leads to symptoms that need quick treatment. Treatment often includes chemotherapy, targeted therapies, and sometimes stem cell transplants.
Those with Pre B ALL or pre-B acute lymphoblastic leukemia all need to know about treatment options. They also need to understand the importance of follow-up care. Thanks to medical research, survival rates have gotten better.
Having a strong support network is key. This includes healthcare providers, family, and support groups. They help deal with the challenges of Pre-B Cell ALL. With the right care and support, we can make life better for those affected.
FAQ
What is Pre-B ALL leukemia?
Pre-B ALL leukemia is a cancer that affects the blood and bone marrow. It’s caused by the growth of immature B-cell precursors.
What are the symptoms of Pre-B ALL leukemia?
Symptoms include anemia, fatigue, and easy bruising. You might also get infections often, feel pain in bones or joints, and have swollen lymph nodes.
How is Pre-B ALL leukemia diagnosed?
Doctors use blood tests, bone marrow biopsies, and genetic tests. These include flow cytometry and genetic testing to find specific mutations.
What are the treatment options for Pre-B ALL leukemia?
Treatments include standard chemotherapy, targeted therapies like monoclonal antibodies, and stem cell transplants. CAR T-cell therapy is also a new option for some patients.
What is the prognosis for Pre-B ALL patients?
The outlook depends on age, genetics, and how well the treatment works. Survival rates vary, and the risk of relapse is a concern.
How do genetic factors influence Pre-B ALL leukemia?
Genetic mutations in B-cell development are key in Pre-B ALL. They affect treatment choices and outcomes.
Can Pre-B ALL leukemia be treated with targeted therapies?
Yes, targeted therapies like monoclonal antibodies and small molecules are used. They offer a precise way to target cancer cells.
What is CAR T-cell therapy for Pre-B cell lymphoblastic leukemia?
CAR T-cell therapy is a new treatment. It makes a patient’s T-cells attack cancer cells. It shows great promise in treating Pre-B cell lymphoblastic leukemia.
How are treatment side effects managed in Pre-B ALL patients?
Managing side effects involves a detailed plan. It aims to reduce both immediate and long-term problems. This ensures survivors have the best quality of life.
References:
- Vora, A., & Goulden, N. (2018). Advances in B-cell Precursor Acute Lymphoblastic Leukemia. British Journal of Haematology, 182(4), 487-497. https://pmc.ncbi.nlm.nih.gov/articles/PMC6746003/
- American Cancer Society. (2025). Childhood acute lymphoblastic leukemia treatment (PDQ®)–Health professional version. https://www.cancer.gov/types/leukemia/hp/child-all-treatment-pdq