Last Updated on November 18, 2025 by Ugurkan Demir

Choosing cervical spine surgery is a big decision. Knowing the risks is key for patient safety and peace of mind. At Liv Hospital, we focus on excellence and care for our patients. We aim to reduce risks and improve outcomes for everyone.
Cervical spine procedures, like those at C5-C6-C7, are vital for treating serious issues. But, they also come with risks. These include ongoing pain, failure of surgical hardware, nerve damage, trouble swallowing, and infection.
It’s important for patients to know about these risks before surgery. We’ll look at the most common complications and side effects. We’ll share the latest medical research to help you understand.
Key Takeaways
- Understanding the risks is key before cervical spine surgery.
- Common issues include ongoing pain, hardware failure, and nerve damage.
- Procedures at C5-C6-C7 levels have specific risks and considerations.
- Liv Hospital prioritizes patient-centered care to minimize risks.
- Staying informed about the latest medical research is essential.
Understanding Cervical Spine Surgery

Cervical spine surgery is a set of procedures aimed at easing pressure on the spinal cord or nerves. We will look at the different surgeries and when they are used. This will help patients understand their choices.
Types of Cervical Spine Procedures
Cervical spine surgery uses various methods, like anterior cervical discectomy and fusion (ACDF), posterior cervical laminectomy and fusion, and cervical disc replacement. Each method is for different neck issues.
| Procedure | Description | Common Indications |
|---|---|---|
| ACDF | Removal of herniated disc and fusion of vertebrae | Herniated discs, spinal stenosis |
| Posterior Cervical Laminectomy and Fusion | Removal of lamina and fusion to stabilize the spine | Spinal stenosis, spondylolisthesis |
| Cervical Disc Replacement | Replacement of damaged disc with artificial one | Herniated discs, degenerative disc disease |
Common Indications for Surgery at C5-C6-C7 Levels
Surgery at the C5-C6-C7 levels is often needed for severe degeneration, compression, or spinal cord injuries. Knowing these reasons is key to picking the right treatment.
Preoperative Considerations
Before cervical spine surgery, a detailed check-up, choosing the right patient, and managing other health issues are vital. We stress the need for careful planning before surgery to get the best results.
Anterior vs. Posterior Surgical Approaches
Anterior and posterior surgical methods are used in cervical spine surgery. Each has its own benefits and risks. The choice depends on the location of the problem, the patient’s anatomy, and the surgeon’s preference.
Anterior Cervical Discectomy and Fusion (ACDF)
ACDF is a common treatment for cervical spine issues. It removes the damaged disc and fuses the vertebrae. A study in Frontiers in Surgery shows it works well for many patients.
Posterior Cervical Laminectomy and Fusion
This method is used for problems at the back or all around. It helps by freeing the spinal cord and stabilizing the spine. But, it might have more risks than the front approach.
Comparative Complication Rates
Studies show anterior surgeries have fewer complications (4-10%). Posterior surgeries have more (15-25%). A medical expert says, “The surgical approach greatly affects the risk of problems in cervical spine surgery.”
Knowing these differences helps make better choices. Talk to your doctor about the risks and benefits of each method. This will help decide the best treatment for you.
Most Common Cervical Spine Surgery Complications
It’s important to know about the risks of cervical spine surgery. This surgery is usually safe but can have complications. We’ll look at common issues, including immediate and long-term problems, and specific issues at the C5-C6-C7 levels.
Immediate Post-Operative Complications
Complications can happen right after surgery. These include:
- Infection: This can lead to the need for antibiotics or more surgery.
- Hematoma: A blood collection that can harm nerves or the spinal cord.
- Respiratory issues: Swelling can make it hard to breathe.
- Dysphagia: Trouble swallowing due to swelling or the placement of hardware.
These problems are usually treated with careful monitoring and medical help. Sometimes, more surgery is needed to fix issues like hematoma or infection.
Long-Term Complications
Complications can also show up months or years later. Some common ones are:
- Hardware failure: This means the implanted parts, like screws, might not work right and need more surgery.
- Adjacent segment degeneration: Wear and tear on nearby spinal segments can cause new symptoms.
- Pseudarthrosis: When the bone doesn’t fuse right, leading to ongoing pain.
- Chronic pain: Pain that lasts a long time, possibly from the surgery not fixing the problem fully or new issues.
Dealing with long-term complications often means ongoing care and might need more surgery.
Specific Complications at C5-C6-C7 Levels
Surgery at the C5-C6-C7 levels has its own risks. These include:
- Nerve root injury: Damage to nerves can cause arm weakness, numbness, or pain.
- Spinal cord injury: This can cause a range of symptoms, from mild weakness to paralysis.
- C5 palsy: A condition that causes weakness or paralysis of muscles controlled by the C5 nerve root.
Knowing these specific risks helps manage patient expectations and improve surgical techniques.
Nerve-Related Complications After Neck Surgery
Nerve injuries can happen after cervical spine surgery. They can come from direct injury or swelling. We’ll look at the causes, signs, and treatments to help patients understand their options.
C5 Palsy and Nerve Root Injury
C5 palsy is a known issue after certain neck surgeries. It causes weakness in muscles controlled by the C5 nerve. Symptoms include deltoid and biceps weakness, affecting daily life.
Spinal Cord Injury Risk
Spinal cord injury is rare but serious after neck surgery. It’s more likely in those with spinal issues. Advanced imaging and neuromonitoring help lower this risk.
Symptoms and Management of Nerve Damage
Nerve damage symptoms vary, from numbness to paralysis. Common signs are:
- Numbness or tingling in the arms or hands
- Muscle weakness
- Loss of coordination
- Pain
Managing nerve damage depends on its severity. Sometimes, physical therapy and pain management work. Other times, surgery is needed to fix the issue.
Dysphagia and Voice Changes Following Anterior Neck Surgery
Anterior neck surgery, like Anterior Cervical Discectomy and Fusion (ACDF), can cause problems. These include swallowing issues and voice changes. These problems can affect a patient’s recovery and life quality. We will look at the causes, symptoms, and how to manage these issues.
Causes of Swallowing Difficulties
Dysphagia, or swallowing problems, can happen after anterior neck surgery. This is due to esophageal irritation, hardware issues, and inflammation. Key causes include:
- Esophageal irritation from surgery tools
- Surgical hardware that sticks out
- Inflammation after surgery
Hoarseness and Vocal Cord Paralysis
Voice changes, like hoarseness and vocal cord paralysis, can happen. This is because of nerve injury during surgery. Symptoms may include:
- Hoarseness or voice quality changes
- Vocal cord paralysis causing breathing or speaking issues
Management and Recovery Timeline
Managing dysphagia and voice changes involves speech therapy and diet changes. Sometimes, more surgery is needed. The recovery time depends on the problem’s severity and the treatment’s success.
It’s important to understand these complications and their management. This helps improve patient care and outcomes after anterior neck surgery.
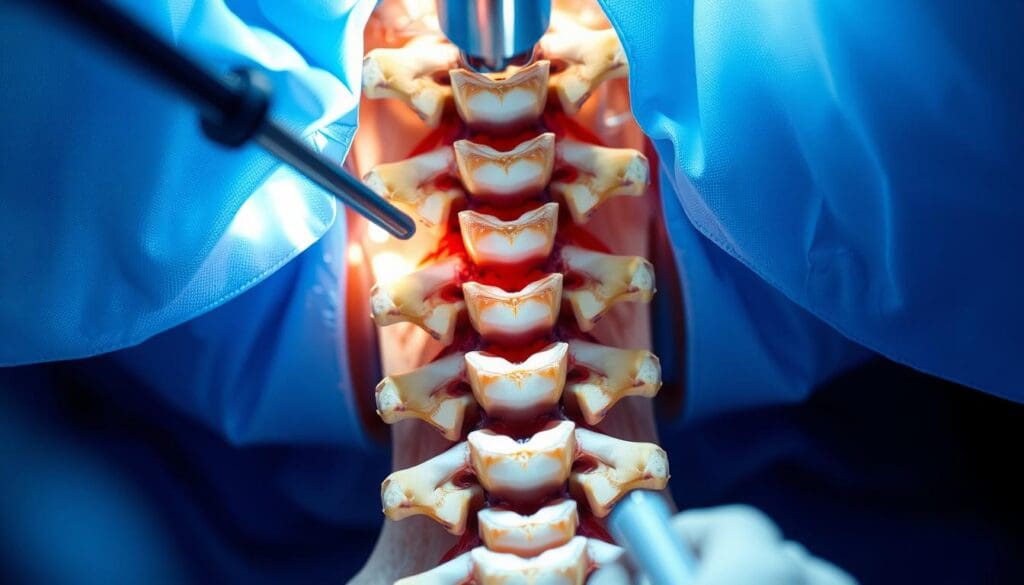
Hardware Complications in Cervical Spine Surgery
Cervical spine surgery is usually safe but can have hardware issues that affect long-term results. We will look at common problems like implant failure, degeneration of adjacent segments, and pseudarthrosis.
Implant Failure and Displacement
Implant failure and displacement are possible issues after cervical spine surgery. Implant failure can happen for many reasons, like bad bone quality or too much stress on the implant. This can cause instability and might need another surgery. We watch patients closely for signs of implant failure to act quickly.
Adjacent Segment Degeneration
Adjacent segment degeneration is a long-term problem that can happen after cervical spine surgery. When vertebrae fuse, it can put more stress on the segments next to them. This can make them wear out faster. Regular follow-up is key to catch early signs of degeneration and treat it well.
Pseudarthrosis (Failed Fusion)
Pseudarthrosis, or failed fusion, is when the bone doesn’t heal right around the implant. This can be because of smoking, bad bone quality, or not being immobilized enough. We use advanced imaging to find pseudarthrosis and plan how to fix it.
Knowing about these hardware problems is key to managing patient hopes and improving surgery results. By understanding the risks and acting early, we can reduce problems and help patients recover better.
Wound Healing and Scarring After Cervical Surgery
Wound healing and scarring are big worries for those having cervical spine surgery. It’s key to heal wounds well to avoid problems and get better fast. We’ll look at infections, scarring from ACDF surgery, and how to handle cosmetic issues.
Incidence and Types of Infections
Wound infections can happen after cervical spine surgery. These can be surface infections or deeper ones that affect the hardware or bone. We’ll talk about who’s at risk and how to prevent these infections.
- Superficial wound infections
- Deep infections involving hardware or bone
Scar Formation After ACDF Surgery
Scarring is a part of surgery. After ACDF surgery, how much scarring you get can vary. We’ll cover what affects scarring and ways to reduce it.
Cosmetic Concerns and Management
Scarring can be a big deal for patients. We’ll look at ways to deal with it, like creams and scar removal surgery.
Understanding wound healing and scarring after cervical surgery helps us manage these issues better. This way, we can improve how patients do after surgery.
Recovery Time After C5-C6-C7 Surgery
The recovery time after C5-C6-C7 surgery can vary a lot. It depends on the type of surgery done. Patients usually have different recovery times based on whether they had an anterior or posterior cervical surgery.
Typical Recovery Timeline for Anterior Procedures
Anterior cervical discectomy and fusion (ACDF) procedures have a shorter recovery time. Most people can get back to their usual activities in 4 to 6 weeks. “Anterior cervical surgery generally allows for quicker recovery due to less muscle disruption,” say spinal surgeons.
We see that patients start feeling better in the first few weeks after surgery.
Extended Recovery After Posterior Cervical Surgery
Posterior cervical surgery takes longer to recover from. This is because it involves more muscle dissection. Patients might need 8 to 12 weeks or more to fully recover.
We stress the need for physical therapy during this time to help with recovery.
Persistent Pain Management Strategies
Managing pain after C5-C6-C7 surgery is very important for a good recovery. We suggest a multi-modal approach. This includes medication, physical therapy, and lifestyle changes.
“Effective pain management is key to improving patient outcomes and facilitating a smoother recovery,” studies say. Our team helps patients create personalized pain management plans.
How Serious is Neck Surgery? Assessing the Risks
It’s important for patients and doctors to understand the risks of neck surgery. This surgery can save lives or greatly improve quality of life. But, it also comes with risks that need careful thought.
Mortality and Serious Complication Rates
While rare, serious complications from neck surgery can have big effects. The death rate for these surgeries is usually low. But, it can change based on the surgery type and the patient’s health.
A study in the Journal of Neurosurgery: Spine showed a death rate of less than 1% for a common surgery called ACDF.
Complications can include spinal cord damage, major nerve problems, and hardware failure. These risks depend on the surgery type, the patient’s health, and how complex the surgery is.
| Complication Type | Incidence Rate |
|---|---|
| Mortality | <1% |
| Spinal Cord Injury | 0.5-1.5% |
| Major Neurological Deficits | 1-3% |
Risk Factors That Increase Surgical Danger
Some factors can make neck surgery riskier. These include diabetes, smoking, and obesity, which can slow healing and raise infection risk. Older age and existing nerve problems can also make surgery harder.
“The presence of comorbidities significantly impacts the risk profile of patients undergoing cervical spine surgery,” notes a study in the Spine Journal. “Careful preoperative evaluation and optimization of these conditions is critical.”
Comparing Risks to Benefits for Different Conditions
When thinking about neck surgery, weighing risks against benefits is key. For those with severe or worsening nerve problems, surgery might be the best choice. But, for milder symptoms, a less invasive approach might be better.
Choosing to have neck surgery should be a personal decision. It depends on the patient’s health, risks, and what surgery can offer.
Conclusion: Making Informed Decisions About Cervical Spine Surgery
As we wrap up our talk on cervical spine surgery, it’s clear that making smart choices is key. Knowing the good and bad sides of surgery helps patients make better decisions.
Cervical spine surgery can change lives, easing chronic pain and boosting life quality. But, it’s important to know the possible risks, like complications and side effects.
This article aims to help patients grasp the surgery’s benefits and risks. We urge patients to talk to their doctors to make choices that fit their needs.
Understanding cervical spine surgery fully is vital for making informed choices. With the right knowledge, patients can face their treatment with confidence.
FAQ
What are the most common complications of cervical spine surgery?
Common complications include infection, hematoma, and breathing problems. Other issues are hardware failure, degeneration of nearby segments, and ongoing pain. Nerve problems like C5 palsy and spinal cord injuries are also concerns.
What is the difference between anterior and posterior cervical spine surgery?
Anterior surgery is done from the front of the neck, often for ACDF. Posterior surgery is from the back, used for laminectomy and fusion. The choice depends on the problem’s location and type.
What are the risks associated with ACDF surgery?
ACDF surgery risks include swallowing and voice issues, hardware failure, and degeneration of nearby segments. Nerve injuries and spinal cord problems are also possible.
How serious is neck surgery, and what are the mortality and serious complication rates?
Neck surgery has risks, but death is rare. Serious complications vary by procedure and patient. Always talk about risks and benefits with a doctor.
What is the typical recovery time after C5-C6-C7 surgery?
Recovery time varies by surgery type and patient. Anterior surgeries usually have quicker recovery than posterior ones.
What are the symptoms and management of nerve damage after neck surgery?
Nerve damage symptoms are numbness, weakness, and pain. Treatment depends on damage severity and location. It may include physical therapy, pain management, or more surgery.
Can cervical spine surgery cause voice changes or swallowing difficulties?
Yes, surgery can affect voice and swallowing due to nerve or esophageal issues. These problems are often temporary but can last for some.
What is the incidence of infection after cervical spine surgery?
Infection rates vary by surgery and patient. Knowing risk factors and preventive steps is key to reducing infection risk.
How can I minimize scarring after ACDF surgery?
Proper wound care and following instructions can reduce scarring. Talking to a doctor about cosmetic concerns helps too.
What are the risk factors that increase the danger associated with neck surgery?
Risks include patient health, surgery complexity, and pre-op evaluation. Understanding these is vital for making informed choices.
How do I compare the risks to benefits for different conditions when considering neck surgery?
Discussing your condition, surgery options, and outcomes with a doctor is key. Knowing the risks and benefits helps in making a decision.
What is the risk of hardware failure or displacement after cervical spine surgery?
Hardware failure or displacement risk depends on hardware type, patient factors, and surgery technique. Understanding and minimizing these risks is important.
Can cervical spine surgery lead to adjacent segment degeneration?
Yes, surgery can cause degeneration of nearby segments due to changed mechanics. Knowing the risks and how to reduce them is essential.
What are the most common complications of cervical spine surgery?
Common complications include infection, hematoma, and breathing problems. Other issues are hardware failure, degeneration of nearby segments, and ongoing pain. Nerve problems like C5 palsy and spinal cord injuries are also concerns.
What is the difference between anterior and posterior cervical spine surgery?
Anterior surgery is done from the front of the neck, often for ACDF. Posterior surgery is from the back, used for laminectomy and fusion. The choice depends on the problem’s location and type.
What are the risks associated with ACDF surgery?
ACDF surgery risks include swallowing and voice issues, hardware failure, and degeneration of nearby segments. Nerve injuries and spinal cord problems are also possible.
How serious is neck surgery, and what are the mortality and serious complication rates?
Neck surgery has risks, but death is rare. Serious complications vary by procedure and patient. Always talk about risks and benefits with a doctor.
What is the typical recovery time after C5-C6-C7 surgery?
Recovery time varies by surgery type and patient. Anterior surgeries usually have quicker recovery than posterior ones.
What are the symptoms and management of nerve damage after neck surgery?
Nerve damage symptoms are numbness, weakness, and pain. Treatment depends on damage severity and location. It may include physical therapy, pain management, or more surgery.
Can cervical spine surgery cause voice changes or swallowing difficulties?
Yes, surgery can affect voice and swallowing due to nerve or esophageal issues. These problems are often temporary but can last for some.
What is the incidence of infection after cervical spine surgery?
Infection rates vary by surgery and patient. Knowing risk factors and preventive steps is key to reducing infection risk.
How can I minimize scarring after ACDF surgery?
Proper wound care and following instructions can reduce scarring. Talking to a doctor about cosmetic concerns helps too.
What are the risk factors that increase the danger associated with neck surgery?
Risks include patient health, surgery complexity, and pre-op evaluation. Understanding these is vital for making informed choices.
How do I compare the risks to benefits for different conditions when considering neck surgery?
Discussing your condition, surgery options, and outcomes with a doctor is key. Knowing the risks and benefits helps in making a decision.
What is the risk of hardware failure or displacement after cervical spine surgery?
Hardware failure or displacement risk depends on hardware type, patient factors, and surgery technique. Understanding and minimizing these risks is important.
Can cervical spine surgery lead to adjacent segment degeneration?
Yes, surgery can cause degeneration of nearby segments due to changed mechanics. Knowing the risks and how to reduce them is essential.
Références
- Journal of Spine Surgery (JSS) : https://jss.amegroups.org/article/view/4813/html
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC4843080/
- Alex Taghva, MD : https://alextaghvamd.com/blog/acdf-surgery-risks
- Surgical Neurology International : https://surgicalneurologyint.com/surgicalint-articles/a-review-of-complication-rates-for-anterior-cervical-diskectomy-and-fusion-acdf
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC7154369