Last Updated on November 18, 2025 by Ugurkan Demir
Vertebral compression fractures are a big worry for the elderly. They often happen because of osteoporosis or injury. Every year, over 1.5 million people worldwide face this issue. It can cause a lot of pain, make it hard to move, and lower the quality of life.
At Liv Hospital, we’re all about giving top-notch care. Our team is ready to help you deal with vertebral compression fractures. We use a full approach to help you.
Key Takeaways
- Understanding the causes and risks of vertebral compression fractures
- The importance of timely diagnosis and treatment
- Overview of the 7 key steps for managing vertebral compression fractures
- Personalized care approaches at Liv Hospital
- Improving patient outcomes through complete care
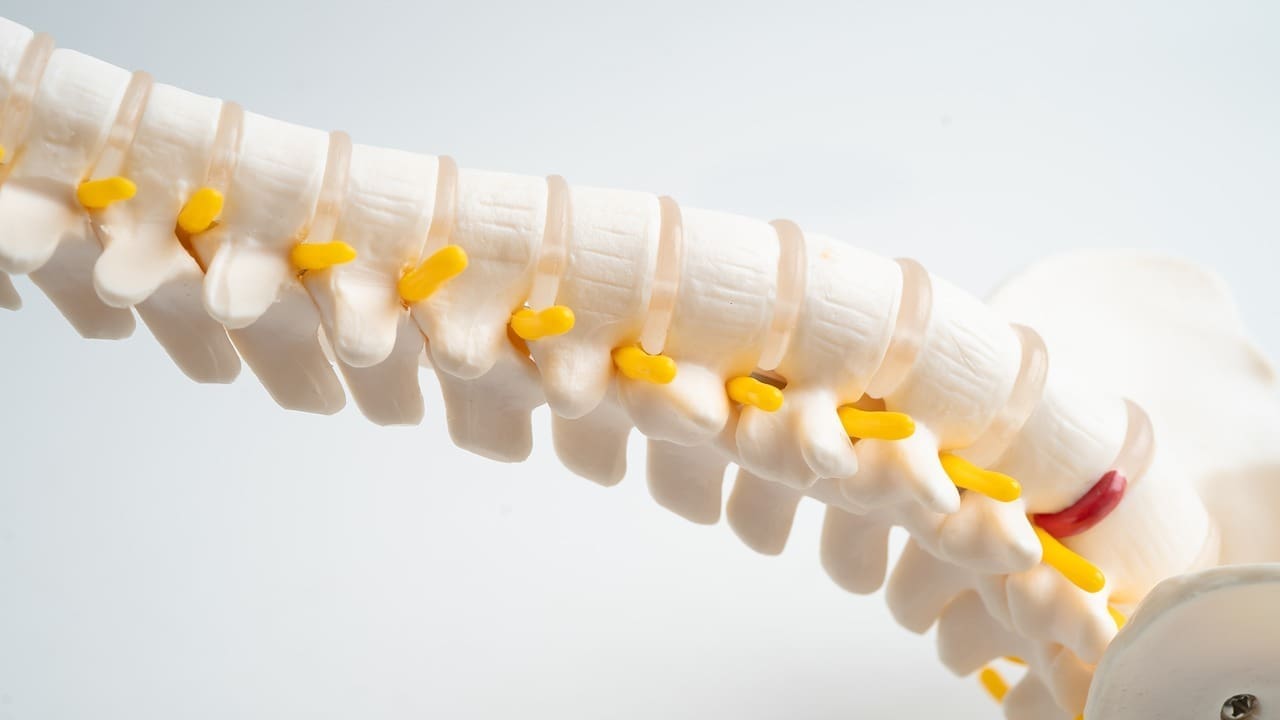
The Impact of Lumbar Compression on Spinal Health

It’s important to know how lumbar compression affects our spine. This can lead to vertebral compression fractures, changing how our spine works and looks.
Definition and Global Prevalence
A compressed vertebral fracture happens when a vertebra collapses. This can be due to osteoporosis, trauma, or disease. It’s a big problem worldwide, affecting millions.
Research shows that vertebral compression fractures can really hurt our ability to function. They can also make our lives less enjoyable.
How Compression Affects Vertebral Structure
When a compression fracture of vertebra happens, it can cause big problems. The vertebra collapsing can push bone fragments into the spinal canal. This can harm our nerves.
The main issues are:
- Altered spinal mechanics
- Potential neurological damage
- Increased risk of further fractures
We see that a vertebral compression fracture is more than just a small problem. It can harm our whole spine. So, it’s key to understand and tackle lumbar compression to avoid long-term damage.
Types and Causes of Vertebral Compression Fractures
It’s important to know about vertebral compression fractures. They can really affect someone’s life if not treated right away.
Wedge Fractures: The Most Common Type
Wedge fractures are the most common. They happen when the front of the vertebra collapses. This makes the vertebra wedge forward. Often, this is because of osteoporosis, which weakens bones.
Burst Fractures and Retropulsion Complications
Burst fractures happen when the vertebra breaks in many directions. This can push bone fragments into the spinal canal. This can hurt the nerves.
Primary Causes: Osteoporosis, Trauma, and Disease
Osteoporosis, trauma, and diseases like cancer cause these fractures. Osteoporosis is a big reason, mainly in older people.
| Cause | Description | Common Population |
|---|---|---|
| Osteoporosis | Weakens bones, making them susceptible to fractures | Elderly |
| Trauma | Physical injury causing immediate fracture | All ages, specially younger individuals |
| Disease (e.g., Cancer) | Diseases that weaken bone structure | Varies depending on disease prevalence |
Doctors say, “Osteoporosis is a silent disease that can lead to significant morbidity if not properly managed.” Early treatment can really help people with these fractures.
Recognizing the Warning Signs and Symptoms
It’s important to know the signs of vertebral compression fractures early. These fractures can show up in different ways. So, it’s key to be aware of the various symptoms.
Acute Pain Presentation
Acute vertebral compression fractures cause sudden, severe back pain. This pain is usually in the fracture area and gets worse with movement. Seeking medical help quickly is vital to manage pain and avoid more harm.
Chronic Pain and Progressive Deformity
Chronic vertebral compression fractures can lead to ongoing pain and spinal deformity. This deformity can make your posture or height look different. It’s important to watch your symptoms and get medical help if they don’t get better or get worse.
When to Seek Immediate Medical Attention
If you have severe back pain, numbness, tingling, or weakness in your legs, get medical help right away. These signs can mean a serious problem, like a severe vertebral compression fracture or nerve damage. We aim to give the best care for patients with these fractures.
Studies show that catching symptoms early is key to managing them well. By knowing the signs and symptoms, patients can get the right care. This helps lower the chance of complications.
Step 1: Obtaining an Accurate Diagnosis
Getting a correct diagnosis is key to managing vertebral compression fractures well. We stress the need for a detailed diagnostic process. This helps tell vertebral compression fractures apart from other spinal injuries.
Clinical Evaluation Process
A thorough clinical evaluation is vital for diagnosing vertebral compression fractures. It includes a detailed medical history and physical exam. Studies show the importance of accurate diagnosis through a mix of clinical evaluation and imaging.
Essential Imaging Techniques
Imaging is key in diagnosing vertebral compression fractures. We use different imaging methods to check the spine accurately.
X-ray Assessment
X-ray is often the first choice for checking vertebral compression fractures. It quickly shows vertebral height and alignment. X-ray is key for spotting fractures and deformities.
CT Scanning Benefits
CT scanning gives more detailed images than X-ray. It’s great for a precise fracture assessment. CT scanning is good for complex fracture checks.
MRI for Soft Tissue Evaluation
MRI is essential for soft tissue injuries with vertebral compression fractures. It shows the spinal cord, nerves, and other soft tissues. MRI is vital for checking spinal health.
By using clinical evaluation and these imaging methods, we can get a precise diagnosis. Then, we can plan an effective treatment for vertebral compression fractures.
Step 2: Initial Pain Management Strategies
Managing pain well is key when treating vertebral compression fractures. It helps improve patients’ quality of life during treatment.
Medication Options and Considerations
There are many ways to manage pain from vertebral compression fractures. You can use over-the-counter pain relievers like acetaminophen and NSAIDs. e severe pain, prescription medications like opioids are available.
- Acetaminophen: Effective for mild to moderate pain
- NSAIDs: Useful for reducing inflammation and relieving pain
- Opioids: Reserved for severe pain management under strict supervision
Non-Pharmaceutical Pain Relief Approaches
There are also non-medical ways to ease pain. These include physical therapy, heat or cold therapy, and relaxation techniques like deep breathing or meditation.
Managing Acute vs. Chronic Pain
It’s important to know the difference between acute and chronic pain. Acute pain happens right after the fracture and needs strong pain management. Chronic pain lasts longer and needs a long-term plan.
Studies show that a mix of medicine and non-medical methods works best for pain relief. We help patients create a pain plan that fits their needs for the best results.
Step 3: Activity Modification and Rest Protocols
The third step in managing vertebral compression fractures is balancing activity and rest. This balance helps in healing, prevents injury, and keeps the spine healthy.
Appropriate Rest Without Deconditioning
Rest is key in recovery, but avoiding deconditioning is also important. Patients should do gentle exercises to keep muscles strong and flexible while resting. Long bed rest can cause muscle loss, bone weakening, and heart health issues.
A study in the Journal of Orthopaedic & Sports Physical Therapy shows the need for rest and activity balance. This prevents deconditioning in vertebral compression fracture patients.
“Prolonged bed rest can result in significant loss of muscle mass and strength, particular in older adults.”
Safe Movement Techniques
Safe movement techniques are key to avoiding injury and aiding healing. We tell patients to avoid heavy lifting, bending, or twisting. They should use proper body mechanics for daily activities.
| Movement | Safe Technique | Action to Avoid |
|---|---|---|
| Lifting | Bend at the knees, keep back straight | Bending at the waist |
| Sitting | Use a straight-backed chair, feet on floor | Slouching or leaning forward |
| Standing | Keep weight evenly distributed on both feet | Leaning to one side |
Gradual Return to Activities
Returning to activities slowly is important to avoid re-injury and ensure a lasting recovery. Patients should increase their activity levels gradually. This helps build strength and endurance without harming the spine.
By following these guidelines, patients can improve their recovery from vertebral compression fractures. This reduces the chance of future spinal problems.
Step 4: Bracing and External Support Methods
Bracing is key in managing vertebral compression fractures. It gives the spine support while it heals. Studies show that the right brace can lead to better recovery.
Types of Braces for Vertebral Compression
There are many braces for vertebral compression fractures. Each one offers different support and stability. Here are a few common ones:
- Jewett braces, which are hyperextension braces used to stabilize the spine and promote healing.
- Thoracic lumbar sacral orthoses (TLSO) braces, which support the thoracic and lumbar regions.
- Cruciform anterior spinal hyperextension (CASH) braces, known for their ease of use and effectiveness in promoting spinal stability.
Proper Fitting and Wearing Schedule
Getting the brace fitted right is important for its effectiveness and comfort. It’s best to have a healthcare professional experienced in orthotics do the fitting. The wearing schedule depends on the fracture’s severity and the brace type.
Patients usually wear the brace for several hours a day. The time can be reduced as the fracture heals.
Duration of Bracing Treatment
The bracing treatment time varies based on the fracture’s severity and healing pace. It’s usually 6 to 12 weeks. Regular check-ups with a healthcare provider are needed to track progress and adjust the treatment if needed.
Knowing about the different braces, how to fit them, and when to wear them helps patients use bracing effectively for vertebral compression fractures.
Step 5: Minimally Invasive Procedures
When other treatments don’t work, we turn to minimally invasive procedures. These steps help treat vertebral compression fractures. They offer pain relief and stability for those who haven’t seen improvement.
Vertebroplasty: Process and Outcomes
Vertebroplasty is a procedure where bone cement is injected into a fractured vertebra. It stabilizes the vertebra and reduces pain. Studies show it can give significant pain relief and improve life quality for those with vertebral compression fractures.
Kyphoplasty: Technique and Benefits
Kyphoplasty is another procedure that stabilizes the vertebra and tries to restore lost height. It uses a balloon to inflate the vertebra before adding bone cement. This method improves spinal alignment and lowers the risk of further deformity.
Patient Selection for Interventional Procedures
Choosing the right patients for vertebroplasty or kyphoplasty is key. We look at the fracture’s severity, osteoporosis, and overall health. Those with severe fractures or who haven’t improved with other treatments are often good candidates.
By carefully choosing and applying the right procedure, we can effectively relieve pain and enhance life quality.
Conclusion: Long-Term Management and Prevention
Managing vertebral compression fractures well needs a few steps. Eating foods high in calcium and vitamin D is key. Also, doing exercises that make your bones stronger is important. Sometimes, taking medicine for osteoporosis is needed.
It’s also vital to prevent falls. You can do this by improving your balance and removing dangers at home. Using tools to help you move around safely is helpful too.
Going to the doctor regularly is a must. They can check your bones and help with any spinal problems.
By following these tips, you can lower your chance of getting more fractures. We aim to give top-notch care to everyone, including international patients. We help them deal with the challenges of spinal health.
FAQ
What is a vertebral compression fracture?
A vertebral compression fracture happens when a vertebra collapses. This usually occurs due to osteoporosis or injury. It causes the vertebra to compress.
What are the symptoms of a vertebral compression fracture?
Symptoms include back pain, a deformity, and sometimes, nerve problems. If you have severe or ongoing pain, see a doctor right away.
How are vertebral compression fractures diagnosed?
Doctors use a physical exam and imaging like X-rays, CT scans, and MRIs. These help see how bad the fracture is and if there are other issues.
What are the treatment options for vertebral compression fractures?
Treatments include pain relief medicines, changing how you move, and using braces. Sometimes, doctors do procedures like vertebroplasty or kyphoplasty.
What is vertebroplasty, and how does it help?
Vertebroplasty is a small procedure where cement is put into the vertebra. It helps stabilize it and ease pain. It’s for those with severe pain or who haven’t gotten better with other treatments.
How can I prevent future vertebral compression fractures?
To prevent fractures, manage osteoporosis, stay at a healthy weight, exercise, and avoid falls. Regular check-ups are also important to keep an eye on your bones.
Can vertebral compression fractures lead to long-term complications?
Yes, if not treated well, fractures can cause chronic pain, more deformity, and lower quality of life. Getting the right treatment early is key to avoiding these problems.
What is the role of bracing in managing vertebral compression fractures?
Bracing helps support the spine and reduce pain. The type and how long you wear it depend on the fracture’s severity and your needs.
Are there different types of vertebral compression fractures?
Yes, there are wedge, burst, and retropulsion fractures. Knowing the type and cause helps doctors choose the best treatment.
How do I know if I have a chronic vertebral compression fracture?
Chronic fractures cause ongoing pain and deformity. If you’ve had a fracture before, it’s important to check in with your doctor to manage any ongoing issues.
Références
- CNSO : https://www.cnsomd.com/blog/spinal-cord-compression-symptoms-treatment-and-urgency
- Canadian Cancer Society : https://cancer.ca/en/treatments/side-effects/spinal-cord-compression
- Merck Manuals (Professional Version) : https://www.merckmanuals.com/professional/neurologic-disorders/spinal-cord-disorders/spinal-cord-compression
- NCBI Bookshelf : https://www.ncbi.nlm.nih.gov/books/NBK557604
- Cancer Research UK : https://www.cancerresearchuk.org/about-cancer/coping/physically/spinal-cord-compression/about