Last Updated on November 18, 2025 by Ugurkan Demir
Choosing cervical spine fusion surgery is a big step towards lasting neck pain relief and spinal stability. At Liv Hospital, we focus on you and use the latest care. This ensures your surgery is safe and effective, from start to finish.
Cervical spine fusion, or cervical neck fusion, is a surgery that connects neck vertebrae. It provides stability and relieves pain. This surgery is usually done when other treatments don’t work for conditions like degeneration, fracture, or instability.
We’ll help you understand the preparation and recovery for this surgery. You’ll get important tips for patients looking for top-notch medical care abroad.
Key Takeaways
- Understanding the purpose and benefits of cervical spine fusion surgery.
- Preparation is key to a successful surgical outcome.
- Recovery process and what to expect post-surgery.
- The importance of a patient-centered approach in care.
- Advanced medical treatments available for international patients.
Understanding Cervical Spine Fusion

Cervical spine fusion, or neck vertebrae fusion surgery, is a special surgery. It fuses two or more vertebrae together to stabilize the neck. This is done to ease pain and provide stability for patients with neck issues.
What is C Spine Fusion Surgery?
Cervical spine fusion surgery uses bone grafts and metal implants. The bone graft connects the vertebrae, helping them grow together. Metal implants, like plates and screws, keep the vertebrae in place until the bone heals.
The main goal is to stabilize the cervical spine. This reduces pain and discomfort from vertebrae movement. By fusing the vertebrae, we prevent nerve irritation and offer lasting relief.
Common Conditions Requiring Cervical Fusion
Several conditions may need cervical spine fusion surgery, including:
- Degenerative disc disease, where the discs between the vertebrae wear out
- Spondylolisthesis, a condition where one vertebra slips over another
- Spinal fractures or trauma to the neck
- Spinal deformities, such as scoliosis or kyphosis
- Infection or tumors affecting the spine
These conditions can cause a lot of pain and instability. Surgery is often needed to address these issues.
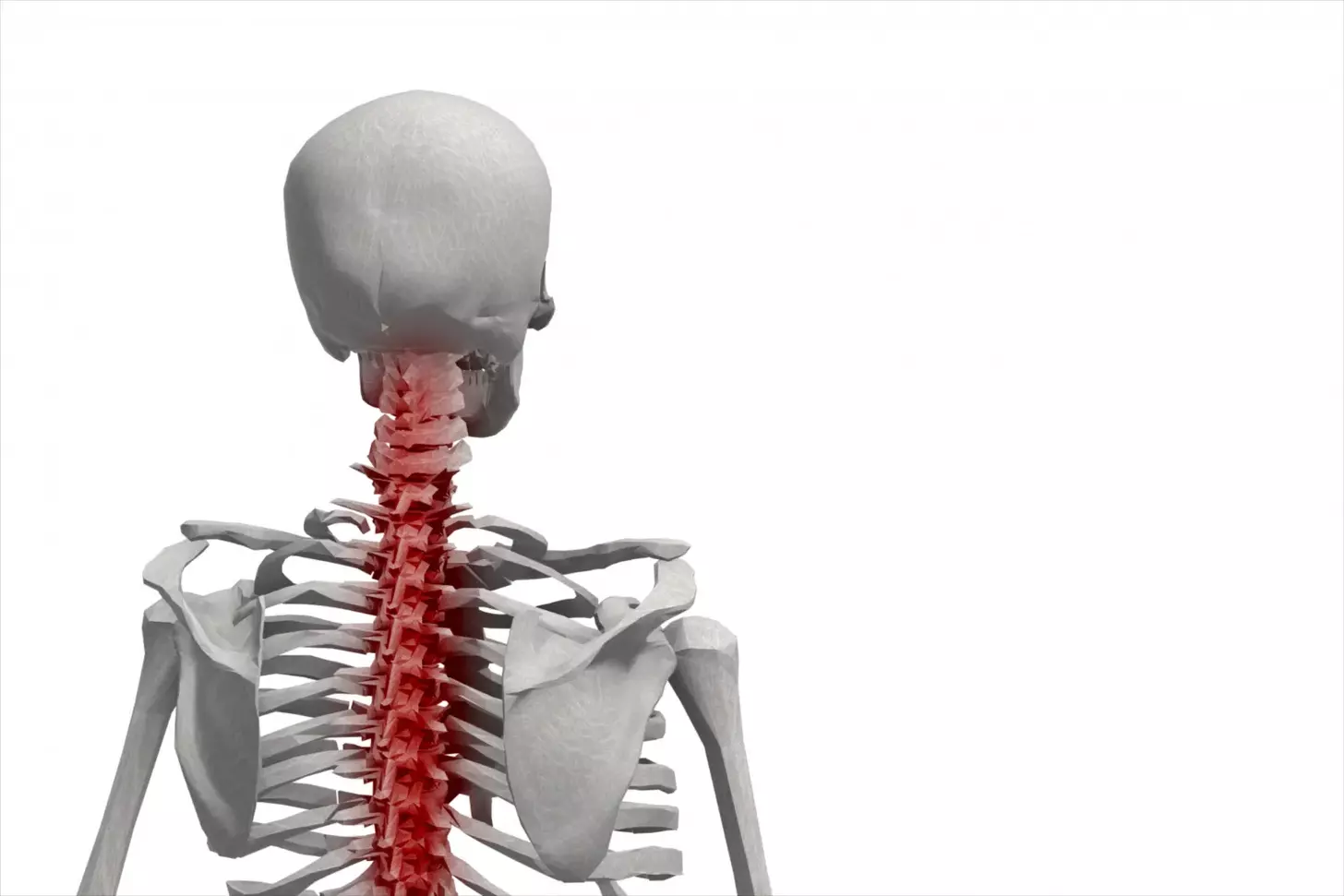
Anatomy of the Cervical Spine
The cervical spine, or neck, has seven vertebrae (C1-C7). They provide flexibility and support for the head. The vertebrae are separated by discs, which absorb shock and allow for smooth movement.
It’s important to know the anatomy of the cervical spine. This helps us understand the surgery and the conditions that need cervical fusion. The cervical spine is complex, and any damage can cause a lot of pain.
When C Spine Fusion is Necessary

For many, cervical spine fusion is needed after trying other treatments. This choice can be tough, but it’s often the best way to fix serious spine problems.
Failed Conservative Treatments
First, we try non-surgical methods like physical therapy and medicine. But if these don’t work, surgery might be next. For example, Meredith had surgery after other treatments didn’t help her.
Common conservative treatments that may fail include:
- Physical therapy and exercises
- Pain management through medication
- Lifestyle changes such as improved posture and ergonomic adjustments
- Epidural steroid injections
Qualifying Conditions for Surgery
Cervical spine fusion is for specific problems that don’t get better with other treatments. These include:
- Degenerative disc disease
- Spinal stenosis
- Scoliosis
- Herniated discs
- Spondylolisthesis
Diagnostic Tests and Evaluations
Before surgery, patients get tests to check their spine. These tests show if and how much surgery is needed.
Common diagnostic tests include:
- X-rays to assess the alignment and structure of the spine
- CT scans to provide detailed images of the spinal anatomy
- MRI scans to evaluate soft tissue and nerve compression
- Myelogram to assess the spinal canal and nerve roots
Understanding these results helps us choose the right surgery and plan the best treatment.
Fusion vs. Non-Fusion Alternatives
It’s important to know the difference between fusion and non-fusion options for your cervical spine. When other treatments don’t work, surgery might be needed.
Conservative Treatment Options
We look at non-surgical treatments first. This includes physical therapy, medication for pain, and changes in your daily life. For example, improving your posture or taking breaks to stretch if you sit a lot.
Key conservative treatments include:
- Physical therapy to strengthen neck muscles and improve flexibility
- Pain management through medication or injections
- Lifestyle changes to reduce strain on the cervical spine
Artificial Disc Replacement
Artificial disc replacement is a non-fusion option for some. It replaces a damaged disc with an artificial one. This helps keep the spine mobile, which is good for those with single-level disc disease.
When Fusion Is the Best Choice
Fusion surgery is best for serious instability or when many parts of the spine are affected. It’s also chosen for severe disc wear or when other surgeries didn’t help.
The benefits of fusion surgery include:
- High success rate for improving symptoms
- Stabilization of the spine
- Potential for significant pain reduction
Choosing surgery is a big decision. We weigh the pros and cons of fusion and non-fusion options. This helps us find the best treatment for your condition and needs.
Types of C Spine Fusion Procedures
Surgeons use different methods for cervical spine fusion. The choice depends on the patient’s condition, health, and the surgeon’s opinion.
Traditional Open Surgery
Traditional open surgery for c spine fusion requires a big incision. This method lets the surgeon see the area clearly. It’s often used for complex cases.
Key aspects of traditional open surgery include:
- A larger incision to provide direct access to the spine
- Potential for more tissue disruption and longer recovery times
- Often used for more complex or severe spinal conditions
Minimally Invasive Spine Fusion Techniques
Minimally invasive spine fusion is becoming more popular. It aims to reduce recovery time and tissue damage. These procedures use smaller incisions and special tools.
Benefits of minimally invasive spine fusion include:
- Smaller incisions, resulting in less scarring
- Reduced muscle damage and less post-operative pain
- Shorter hospital stays and faster return to normal activities
Recent advancements have made minimally invasive spine fusion a good option for many patients.
Bone Grafts and Hardware Options
Bone grafts are key in spinal fusion surgery. They help new bone tissue grow, joining vertebrae. Hardware like plates, screws, and rods helps keep the spine stable while it heals.
Types of bone grafts used in c spine fusion include:
- Autografts (taken from the patient’s own body)
- Allografts (donated bone tissue)
- Synthetic bone grafts
The choice of bone graft and hardware depends on the patient’s condition, the surgeon’s preference, and the fusion procedure’s needs.
Benefits and Risks of Cervical Fusion Surgery
Cervical fusion surgery is a common treatment for many cervical spine problems. It helps patients with chronic pain and improves their quality of life. It’s important to know both the good and bad sides of this surgery.
Expected Outcomes and Success Rates
Research shows cervical spine fusion surgery works well for some patients. It has results as good as or better than other treatments. Many patients feel less pain and see better neurological function.
Here are some good things that can happen after surgery:
- Less or no chronic neck pain
- Better movement and range of motion
- A stable cervical spine
- Less numbness or tingling
The success of the surgery depends on several things. These include the patient’s health, the condition being treated, and the surgical method.
Potential Complications
Even though cervical fusion surgery is usually safe, there are risks. These can include:
- Infection at the surgery site
- Nerve damage or irritation
- Hardware failure (if used)
- Pseudarthrosis (bones not fusing)
- Adjacent segment disease
It’s important for patients to talk to their surgeon about these risks. This helps understand how they might affect each person.
Long-term Considerations
After surgery, patients need to think about long-term effects. These can affect their recovery and spinal health. These include:
- Possible disease in the vertebrae next to the fused area
- Need for ongoing care to check the fusion and spinal health
- Limitations in neck movement due to the fusion
Knowing these long-term factors helps patients prepare for life after surgery. It helps them make informed decisions about their care.
Pre-Surgery Preparation
The weeks before cervical spine fusion surgery are key for your health and recovery. We’ll show you how to get ready for a successful surgery and recovery.
Choosing the Right Surgeon
Finding a skilled surgeon is vital for a good cervical spine fusion surgery. Look into your surgeon’s qualifications, like their experience with spinal fusion and success rates. says a seasoned surgeon can greatly improve your surgery’s outcome.
Medical Evaluations and Tests
We’ll do detailed medical checks before surgery to check your health and spot risks. These might include:
- Blood tests for infections or bleeding issues
- Imaging tests like X-rays, MRI, or CT scans to see your spine’s condition
- Heart checks to make sure your heart is strong enough for surgery
Medication Adjustments
Some medications might need to be changed or stopped before surgery to lower risks. We’ll look at your meds, like blood thinners, and tell you what changes are needed.
Home Preparation for Recovery
Getting your home ready for recovery is key for a smooth transition after surgery. We suggest:
| Preparation Task | Description |
|---|---|
| Clearing clutter | Remove tripping hazards and make your home path clear |
| Setting up a recovery area | Make a comfy and quiet spot for rest and recovery |
| Stocking essentials | Have food, water, and meds easily accessible |
By taking these steps, you can set yourself up for a successful surgery and recovery. We’re here to support you every step of the way.
What to Expect During C Spine Fusion Surgery
As you prepare for C spine fusion, knowing what to expect can be reassuring. We believe being informed helps reduce anxiety and makes the experience smoother.
Anesthesia and Surgical Setup
C spine fusion surgery is usually done under general anesthesia. This keeps you comfortable and pain-free during the procedure. We use the latest anesthesia techniques and monitoring for your safety.
Anesthesia for spine surgery is key. It lets us make the necessary corrections without causing you stress or discomfort.
Surgical Approaches (Anterior vs. Posterior)
The surgical approach for spine fusion depends on your condition and the surgeon’s judgment. There are two main approaches: anterior (from the front) and posterior (from the back).
- Anterior Approach: This method accesses the spine from the front of the neck. It’s used for some cervical spine fusions.
- Posterior Approach: This method accesses the spine from the back of the neck. It’s used for conditions needing back stabilization.
Duration and Hospital Stay
The surgery can last from 2 to 4 hours, depending on the case. Most patients leave the hospital a few days after surgery. They must be stable and recovering well.
| Surgery Duration | Hospital Stay |
|---|---|
| 2-4 hours | 2-3 days |
Immediate Post-Operative Experience
After surgery, you’ll be watched closely in the recovery room for any issues. We focus on pain management. We use medicines and other methods to reduce pain.
Recovery times vary for patients. Some recover quickly, while others need more time. Our team provides detailed post-operative care to support your recovery.
Studies, like Meredith’s successful surgery, show that many patients are discharged within a few days. But, everyone’s experience is different.
Early Post-Operative Care
The time right after cervical spine fusion surgery is very important. Good care can really help with recovery. It includes managing pain, taking care of the wound, and watching for any problems.
Pain Management Strategies
Managing pain is key after surgery. We use many ways to help, like medicine, physical therapy, and relaxation techniques.
Medications are a big part of pain control. We’ll tell you how to use them right, including how much and any side effects.
Wound Care and Monitoring
It’s very important to take good care of the wound to avoid infection and help it heal. We’ll show you how to care for the surgical site and what to watch for.
Keep an eye on the wound for any signs of trouble, like redness, swelling, or discharge. If you see anything odd, call your doctor right away.
Neck Brace and Support Options
You might need a neck brace or cervical collar to keep your neck stable early on. We’ll talk about the different kinds and how to use them.
The right neck brace depends on your surgery and needs. Your doctor will choose the best one for you.
Warning Signs to Watch For
Know the warning signs for problems like infection, nerve damage, or hardware failure. Look out for severe pain, numbness or tingling, trouble swallowing, or fever.
If you notice any of these, get help fast. Catching and treating problems early can make a big difference.
Physical therapy is also key in getting better after neck fusion surgery. It helps you move and get strong again. Like Meredith, a good physical therapy plan can lead to a great recovery.
| Warning Signs | Possible Complications | Action |
|---|---|---|
| Severe pain, numbness, tingling | Nerve damage | Seek medical attention |
| Difficulty swallowing, fever | Infection | Contact healthcare provider |
| Increasing pain, hardware failure symptoms | Hardware failure | Immediate medical evaluation |
Recovery Timeline and Rehabilitation
Recovering from cervical spine fusion surgery takes time and effort. It involves a series of steps to help you regain strength and mobility. Each stage is important for a full recovery.
Activity Restrictions in the First Few Weeks
In the first weeks, you’ll need to limit your activities. This means avoiding heavy lifting, bending, or twisting. A study in BMC Public Health shows that a good rehab plan can greatly improve your outcome.
Initial Physical Therapy (1-3 Months)
After 1-3 months, you’ll start physical therapy. This stage helps you regain basic mobility and strength. You’ll do gentle exercises to improve your range of motion and reduce stiffness.
It’s key to work with a healthcare professional to make sure your physical therapy fits your needs.
Progressive Strengthening (3-6 Months)
Between 3-6 months, you’ll move to more intense strengthening exercises. This phase is vital for getting back your functional strength. Always work with your physical therapist to ensure you’re doing exercises correctly and safely.
Return to Normal Activities (6-12 Months)
Most people can get back to normal activities in 6-12 months. This time can vary based on your surgery and health. It’s important to be patient and not rush your recovery.
The following table outlines a general recovery timeline and rehabilitation milestones:
| Timeframe | Recovery Stage | Activities |
|---|---|---|
| 0-3 weeks | Initial Recovery | Rest, limited activity, pain management |
| 1-3 months | Initial Physical Therapy | Gentle exercises, mobility improvement |
| 3-6 months | Progressive Strengthening | Strengthening exercises, functional training |
| 6-12 months | Return to Normal Activities | Gradual return to full activities, sports |
Every patient’s recovery is different. Your health, age, and surgery specifics can affect your timeline. By sticking to a structured rehab plan and working with healthcare professionals, you can achieve the best results after cervical spine fusion surgery.
Life After Cervical Spine Fusion
The journey doesn’t end after cervical spine fusion surgery. It’s key to know what to expect in the years ahead. The surgery can greatly improve symptoms but may require avoiding certain activities and making long-term care changes.
Long-term Activity Modifications
Patients often need to adjust their lifestyle after surgery. They should avoid heavy lifting, bending, or twisting. They also need to change their exercise routines to fit their new spine.
Meredith’s story shows how important lifestyle changes are. She made her activities less stressful on her neck. She did gentle exercises and stayed away from contact sports.
Preventing Adjacent Segment Disease
One big concern after surgery is adjacent segment disease (ASD). ASD happens when the vertebrae next to the fused area get stressed. This can lead to more degeneration or herniation.
To lower this risk, patients should keep a healthy weight and exercise regularly but safely. They should also keep good posture. Regular check-ups are key to watch the spine and catch any problems early.
“Understanding the possible long-term issues and taking steps to prevent them can greatly improve life after cervical spine fusion surgery.”
Follow-up Care Schedule
Having a set follow-up care plan is important. It helps track healing and catch any problems early. Follow-ups are usually at 3, 6, and 12 months after surgery, and then every year after that.
- First visits check on wound healing and pain control.
- Later visits look at how well the fusion is doing and the spine’s health.
- Long-term visits watch for signs of adjacent segment disease and other issues.
When to Contact Your Doctor
It’s important for patients to know when to call their doctor after surgery. Look out for severe pain, numbness or tingling in your arms or legs, trouble walking, or signs of infection like fever or redness around the surgery site.
Knowing these signs and talking openly with your healthcare team can help you get the best results after cervical spine fusion surgery.
Conclusion
Cervical spine fusion surgery is a complex process. It needs careful planning, precise surgery, and good care after. Understanding the benefits and risks is key.
Getting ready for surgery is very important. You need to pick the right doctor and do medical checks. Also, you should adjust your meds and daily life. Knowing the risks helps you recover smoothly.
Rehab is a big part of getting better. It involves slowly getting back to normal and therapy. It’s important to know the risks and work with your healthcare team.
We aim to give patients the knowledge to make good choices about their care. With the right care and rehab, patients can recover well and live better.
FAQ
What is cervical spine fusion surgery?
Cervical spine fusion surgery is a procedure that fuses neck vertebrae together. This is done to stabilize the spine and ease pain. It’s usually needed when other treatments don’t work for conditions like degeneration or fractures.
What are the common conditions that require cervical fusion?
Conditions needing cervical fusion include degenerative disc disease and spinal stenosis. Scoliosis, fractures, and instability also require this surgery.
How is cervical spine fusion surgery performed?
The surgery can be done through open surgery or minimally invasive methods. It uses bone grafts and metal implants to join the vertebrae.
What are the benefits of cervical spine fusion surgery?
The surgery relieves pain, stabilizes the spine, and improves life quality. It also helps prevent further damage or degeneration.
What are the risks and possible complications of cervical spine fusion surgery?
Risks include infection, nerve damage, and hardware failure. Adjacent segment disease is also a complication.
How long does it take to recover from cervical spine fusion surgery?
Recovery time varies, but most people can get back to normal in 6-12 months.
What is the role of physical therapy in cervical spine fusion recovery?
Physical therapy is key in regaining mobility and strength. Patients should follow a professional’s advice on exercises.
What are the long-term implications of cervical spine fusion surgery?
Long-term effects include the risk of adjacent segment disease. Ongoing care and activity modifications are also needed.
How can I prevent adjacent segment disease after cervical spine fusion surgery?
Preventing adjacent segment disease requires a healthy lifestyle and following professional advice. Regular check-ups are also important.
What is the difference between cervical spine fusion and artificial disc replacement?
Fusion fuses vertebrae together, while replacement uses an artificial disc. The choice depends on the condition and patient’s health.
How do I choose the right surgeon for cervical spine fusion surgery?
Choose a surgeon by researching their qualifications and success rates. Ask about their approach and care team.
What are the necessary preparations for cervical spine fusion surgery?
Preparations include medical evaluations, medication adjustments, and home preparation for recovery.
What is cervical spine fusion surgery?
Cervical spine fusion surgery is a procedure that fuses neck vertebrae together. This is done to stabilize the spine and ease pain. It’s usually needed when other treatments don’t work for conditions like degeneration or fractures.
What are the common conditions that require cervical fusion?
Conditions needing cervical fusion include degenerative disc disease and spinal stenosis. Scoliosis, fractures, and instability also require this surgery.
How is cervical spine fusion surgery performed?
The surgery can be done through open surgery or minimally invasive methods. It uses bone grafts and metal implants to join the vertebrae.
What are the benefits of cervical spine fusion surgery?
The surgery relieves pain, stabilizes the spine, and improves life quality. It also helps prevent further damage or degeneration.
What are the risks and possible complications of cervical spine fusion surgery?
Risks include infection, nerve damage, and hardware failure. Adjacent segment disease is also a complication.
How long does it take to recover from cervical spine fusion surgery?
Recovery time varies, but most people can get back to normal in 6-12 months.
What is the role of physical therapy in cervical spine fusion recovery?
Physical therapy is key in regaining mobility and strength. Patients should follow a professional’s advice on exercises.
What are the long-term implications of cervical spine fusion surgery?
Long-term effects include the risk of adjacent segment disease. Ongoing care and activity modifications are also needed.
How can I prevent adjacent segment disease after cervical spine fusion surgery?
Preventing adjacent segment disease requires a healthy lifestyle and following professional advice. Regular check-ups are also important.
What is the difference between cervical spine fusion and artificial disc replacement?
Fusion fuses vertebrae together, while replacement uses an artificial disc. The choice depends on the condition and patient’s health.
How do I choose the right surgeon for cervical spine fusion surgery?
Choose a surgeon by researching their qualifications and success rates. Ask about their approach and care team.
What are the necessary preparations for cervical spine fusion surgery?
Preparations include medical evaluations, medication adjustments, and home preparation for recovery.