Last Updated on November 4, 2025 by mcelik
Did you know over 1 million people in the United States get bursitis every year? Many of them feel pain that goes down their legs. Understanding how bursitis leg pain spread occurs can help you manage your symptoms better.
Dealing with leg pain can really mess up your day. Bursitis leg pain spread happens when inflammation in the bursa affects nearby nerves and tissues, causing pain to travel from the joint down the leg. Bursitis, which is the swelling of the fluid-filled sacs around joints, can be very painful and limit your movement.
We’re going to look into bursitis leg pain spread in the leg and how it might affect other areas. We’ll cover what causes it, its symptoms, and how to treat it. Our aim is to help you understand bursitis and its effects on leg pain symptoms.
Key Takeaways
- Bursitis can cause a lot of leg pain and discomfort.
- Knowing the causes and symptoms is key to treating it well.
- There are many ways to manage bursitis-related leg pain.
- Getting a correct diagnosis is important for the right treatment.
- We’ll also look at how bursitis might spread down the leg.
What Is Bursitis and How Does It Affect the Body?
Bursitis is when the bursae get inflamed. Bursae are small sacs filled with fluid. They cushion bones, tendons, and muscles, making movement smooth.
Definition and Function of Bursae
Bursae are key in our musculoskeletal system. They act as a gliding surface between bones, tendons, and muscles. They are found in areas where friction is common. The primary function of bursae is to reduce friction, absorb shock, and help with movement.
Common Locations for Bursitis
Bursitis can happen in many places, but it’s most common in:
- Shoulders
- Elbows
- Hips
- Knees
- Heels
These areas get a lot of use and stress, making them more likely to get bursitis.
The Inflammatory Process in Bursitis
The inflammation in bursitis involves immune cells and chemical mediators. When a bursa gets inflamed, it causes pain, swelling, and limits movement. Knowing how it works helps us find better treatments.
Looking at how bursitis affects the body is important. It can make daily activities hard and lower our quality of life. The pain from bursitis can be severe and may become a long-term problem if not treated.
Types of Bursitis That Can Affect the Leg
It’s important to know the different types of bursitis that can hit the leg. Each type has its own causes and symptoms. We’ll look at the most common types to help you figure out what might be causing your pain.
Hip Bursitis (Trochanteric Bursitis)
Hip bursitis, or trochanteric bursitis, happens when the bursa near the hip gets inflamed. This can lead to pain on the outside of the hip, which might spread down the thigh. Walking or climbing stairs can make the pain worse. It’s a common issue for athletes and people who do a lot of hip movements.
Knee Bursitis (Prepatellar and Pes Anserine Bursitis)
Knee bursitis is another common problem. It comes in two types: prepatellar and pes anserine bursitis. Prepatellar bursitis is at the front of the knee, causing swelling and pain, often in people who kneel a lot. Pes anserine bursitis is on the lower inner knee, causing pain when climbing stairs or getting up from bed.
Ankle and Heel Bursitis (Retrocalcaneal Bursitis)
Ankle and heel bursitis, or retrocalcaneal bursitis, is when the bursa between the Achilles tendon and the calcaneus bone gets inflamed. This causes pain at the back of the heel, which is tough for athletes and people with bad shoes. The pain gets worse with activity and better with rest.
Ischial Bursitis (Weaver’s Bottom)
Ischial bursitis, or weaver’s bottom, affects the bursa near the ischial tuberosity, the bony part in the buttocks where you sit. It causes pain when sitting or lying on it. It’s common in cyclists or people who sit a lot, like those with desk jobs.
Each type of bursitis in the leg has its own traits and causes. Knowing which type you have is key to treating it right. We’ll keep exploring the causes, symptoms, and treatments for bursitis in the next sections.
Understanding Bursitis Leg Pain Spread: Can It Really “Spread”?
It’s important to know if bursitis pain can spread. Bursitis is when the bursae get inflamed. This can make pain move to other parts of the leg.
The Mechanism of Pain Radiation
Pain spreading is due to the inflamed bursa and the nervous system. When a bursa gets inflamed, it can bother nearby nerves. This sends pain signals to the brain.
The pattern of pain spreading depends on where the bursa is. For example, hip bursitis can make pain go down the outside of the thigh.
Difference Between Spreading Infection and Spreading Pain
It’s key to tell the difference between infection spread and pain spread. Bursitis is usually an inflammatory issue. But sometimes, it can get infected (septic bursitis).
Infected bursitis is a serious issue that needs quick medical help. Pain spreading is about nerve irritation and inflammation around tissues.
| Characteristics | Spreading Infection | Spreading Pain |
| Cause | Bacterial infection | Inflammation and nerve irritation |
| Symptoms | Redness, warmth, swelling, fever | Pain radiating to surrounding areas |
| Treatment | Antibiotics, drainage | Anti-inflammatory medications, physical therapy |
How Inflammation Affects Surrounding Tissues

Inflammation from bursitis can harm nearby tissues. It can cause swelling that presses on nerves and other bursae.
It also releases chemicals that make nerves more sensitive. This can make pain feel like it’s coming from a wider area.
Knowing how this works helps doctors create better treatment plans. They need to treat the inflamed bursa and the surrounding tissues and pain.
Common Causes of Bursitis in the Leg
Many things can lead to bursitis in the leg. These include repetitive strain and certain medical conditions. Knowing what causes it helps in preventing and treating it.
Repetitive Motion and Overuse
Repetitive motion often causes bursitis, mainly in athletes or those with jobs that involve a lot of leg movement. Running, cycling, or climbing stairs can irritate and inflame the bursae.
Examples of repetitive motion injuries include:
- Runner’s knee (prepatellar bursitis)
- Trochanteric bursitis from repetitive hip movements
Direct Trauma or Injury
Direct trauma to the leg can damage the bursae, leading to bursitis. This can happen from a fall, a blow to the area, or prolonged pressure on the bursa.
“Trauma to the hip or knee area can lead to the development of bursitis, if the injury is not properly managed.”
Falling onto the knee or hip, or getting hit during sports are examples.
Inflammatory Conditions and Autoimmune Disorders
Some inflammatory conditions and autoimmune disorders raise the risk of bursitis. Conditions like rheumatoid arthritis, gout, and other inflammatory arthropathies can cause it.
Rheumatoid arthritis, for example, can cause inflammation in many bursae, including those in the leg.
Infection (Septic Bursitis)
Septic bursitis happens when a bursa gets infected, usually through bacteria entering through a skin break. It needs quick medical care to avoid serious problems.
Risk factors for septic bursitis include:
- Pre-existing skin conditions or wounds near the bursa
- Compromised immune system
Symptoms That Mimic Bursitis Leg Pain Spread
Many medical conditions can look like bursitis, making it hard to diagnose. Leg pain is often thought to be from bursitis. But, other issues can cause similar symptoms, making it tough to figure out what’s wrong.
Sciatica and Nerve Compression
Sciatica is often mistaken for bursitis. It happens when the sciatic nerve gets compressed or irritated. This nerve runs from the lower back to the legs. Symptoms include sharp pain, numbness, and tingling in the leg.
Nerve compression signs can be tricky to spot. They often look like bursitis symptoms.
Tendonitis and Muscle Strains
Tendonitis and muscle strains can also cause leg pain like bursitis. Tendonitis is from overuse or repetitive motion. Muscle strains happen from sudden injury or overstretching.
Both can cause a lot of pain and make it hard to move.
Vascular Conditions
Vascular conditions, like peripheral artery disease (PAD), can also cause leg pain. PAD narrows arteries, cutting off blood flow to the limbs. This pain happens during physical activity.
Referred Pain from Spine Issues
Spine problems, like herniated discs or spinal stenosis, can also cause leg pain. This pain is felt in areas other than the actual problem. It makes diagnosis hard.
Knowing about these conditions is key for the right diagnosis and treatment. By understanding the differences, doctors can give better care.
Diagnosing the Source of Leg Pain
Diagnosing leg pain requires a detailed look at the symptoms and tests. We use many methods to find the cause of pain. This ensures we can treat it well.
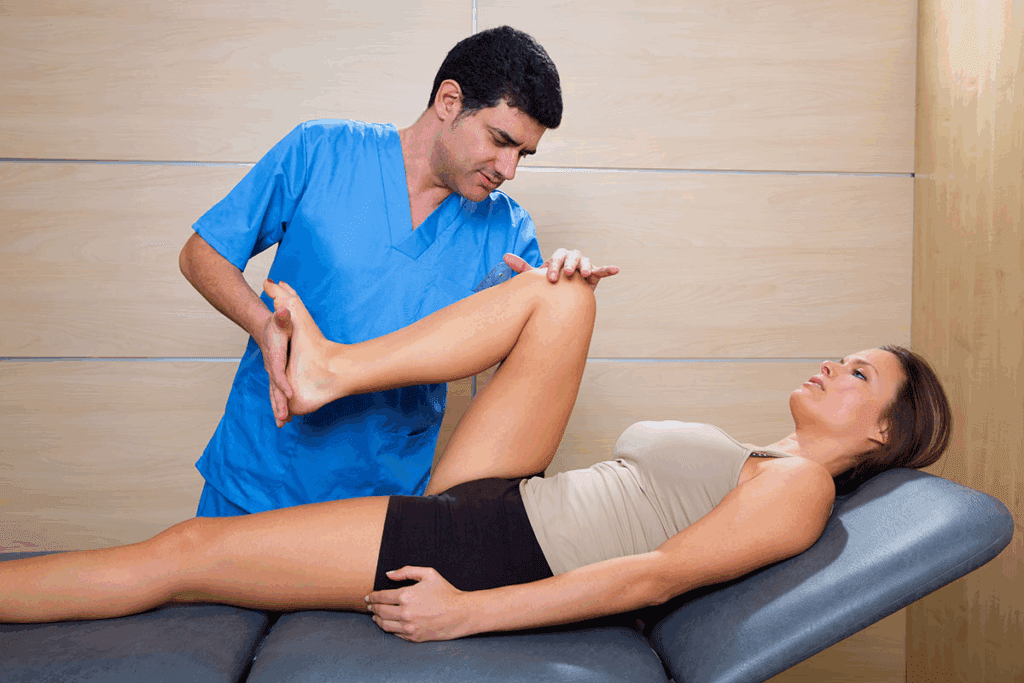
Physical Examination Techniques
A detailed physical check is key in finding leg pain’s cause. We look at the patient’s past health, check the painful area, and do special tests. Physical examination techniques help us see how well the area moves, the muscle strength, and if nerves are affected.
We might do tests like a straight leg raise to check for sciatica. Or we might check the knee’s stability to see if ligaments are hurt.
Imaging Studies (X-rays, MRI, Ultrasound)
Imaging tests are very important in finding leg pain’s cause. We use X-rays to see bones, MRI for soft tissue, and ultrasound for tendons and ligaments. These tests let us see inside and find pain causes.
An MRI can spot tendonitis, ligament sprains, or bursitis. X-rays can show fractures or bone wear.
Laboratory Tests for Inflammatory Markers
Lab tests are key in finding inflammation that might cause leg pain. We test blood for markers like ESR or CRP to see inflammation levels.
These tests help us find conditions like rheumatoid arthritis or infections that might be causing pain.
Differential Diagnosis Process
The differential diagnosis process looks at many possible causes of leg pain. We use symptoms, imaging, and lab results to narrow down causes.
By carefully looking at symptoms, medical history, and test results, we can find the exact cause. Then, we can make a good treatment plan.
The Pain Pathway: How Bursitis Pain Travels Through the Leg
To understand bursitis pain, we must see how it moves through the leg. Bursitis pain travels through the nerves. Knowing this helps us manage it better.
Neurological Mechanisms of Pain Transmission
Bursitis pain travels through complex nerve paths. When a bursa gets inflamed, it hurts the nerves around it. These nerves send pain signals to the spinal cord and brain.
This process uses many neurotransmitters and pain modulators. They can make the pain stronger or weaker. The pain path is not simple. It involves many connections and sensory inputs.
Referred Pain Patterns in Leg Bursitis
Referred pain is common in bursitis. For example, hip bursitis can cause thigh or knee pain. Knowing these patterns helps in diagnosing and treating.
In leg bursitis, pain can spread in different ways. It depends on the bursa and the person’s body. Often, pain follows nerve paths, like the sciatic nerve in ischial bursitis.
Pain Distribution Maps for Different Types of Bursitis
Each type of bursitis in the leg has its own pain pattern. Trochanteric bursitis hurts the outer hip and thigh. Prepatellar bursitis affects the knee’s front.
| Type of Bursitis | Common Pain Location | Radiation Pattern |
| Trochanteric Bursitis | Outer hip | Down the lateral thigh |
| Prepatellar Bursitis | Front of the knee | Localized, may radiate slightly around the kneecap |
| Ischial Bursitis | Buttock area | Down the back of the thigh, potentially to the lower leg |
Central Sensitization and Chronic Pain Development
Central sensitization is key in chronic pain from bursitis. When pain lasts, it changes the nervous system. This makes it more sensitive to pain.
Understanding central sensitization is vital for treating chronic pain. We need to treat the inflammation and the nervous system’s response to pain.
Risk Factors for Developing Bursitis in the Leg
Knowing the risk factors for bursitis in the leg is key to preventing it. Bursitis is an inflammatory condition that affects the bursae. It can greatly impact a person’s quality of life. We will look at the factors that increase the risk of getting bursitis in the leg.
Age-Related Factors
Age is a big risk factor for bursitis in the leg. As we get older, our bursae don’t work as well. This makes them more likely to get inflamed. Older adults are more at risk because of years of wear and tear on their joints.
Occupational and Athletic Risk Factors
Certain jobs and sports can raise the risk of bursitis. For example, people who do repetitive motions or put a lot of stress on their joints are at higher risk. This includes:
- Athletes in high-impact sports
- Workers who often kneel or climb
- People with jobs that require a lot of leg movement
Medical Conditions That Increase Risk
Some medical conditions make people more likely to get bursitis. These include:
- Rheumatoid arthritis
- Gout
- Diabetes
- Infections that can spread to the bursae
These conditions can either directly affect the bursae or make inflammation more likely.
Anatomical Variations and Biomechanical Issues
Anatomical variations and biomechanical issues can also lead to bursitis. For instance, differences in leg length or abnormal gait patterns can put uneven stress on the bursae. This can cause inflammation.
By knowing these risk factors, people can take steps to lower their chance of getting bursitis in the leg. This includes changing activities, using protective gear, and managing any underlying medical conditions.
When Bursitis Becomes Chronic: Long-term Effects on Leg Function
Chronic bursitis can have lasting effects on leg function. It can change how you walk, weaken muscles, and affect your mood. These changes can lower your quality of life.
Changes in Gait and Movement Patterns
Chronic bursitis often alters an individual’s walking pattern as a means to avoid pain. This can lead to abnormal wear and tear on other joints. It might cause more problems.
People often adjust their walk to avoid pain. This can affect their mobility in many ways.
Muscle Weakness and Atrophy
Long-term inflammation and pain from chronic bursitis can weaken muscles. This is because of reduced movement and the body’s natural pain response.
Medical pain mapping helps find the most affected muscle areas. It guides specific rehabilitation efforts.
Impact on Joint Health and Mobility
Chronic bursitis can harm joint health and mobility. The ongoing inflammation causes joint stiffness and reduced range of motion. This makes daily tasks hard.
| Joint Issue | Effect on Mobility | Common Symptoms |
| Joint Stiffness | Reduced flexibility | Pain, stiffness |
| Reduced Range of Motion | Limited mobility | Pain during movement |
Psychological Effects of Chronic Leg Pain
Chronic bursitis pain can cause psychological effects like depression and anxiety. The ongoing discomfort can harm mental health. It’s important to treat both physical and mental pain.
Knowing how chronic bursitis affects mental health is key. It helps in giving full care to those with chronic bursitis.
Medical Treatments for Bursitis in the Leg
There are many ways to treat bursitis in the leg. The right treatment depends on how bad the bursitis is, what caused it, and where it is. These treatments can help make life better for those with bursitis.
Anti-inflammatory Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) help with pain and swelling. Over-the-counter NSAIDs like ibuprofen work well for mild to moderate cases. For more severe cases, doctors might prescribe stronger NSAIDs.
It’s important to take the right amount of medicine. Always talk to a doctor before starting any new medication, even if it’s over-the-counter. This is true for people with stomach problems or other health issues.
Corticosteroid Injections
Corticosteroid injections are very effective for reducing swelling and pain. These injections put medicine right where it’s needed. They are used when other treatments don’t work or when the bursitis is very bad.
Even though these injections work well, they can have side effects. These might include pain where the injection was given, thinner skin, and, rarely, infection.
Antibiotics for Septic Bursitis
For bursitis caused by an infection, antibiotics are the main treatment. The type of antibiotic needed depends on the bacteria causing the infection. Sometimes, taking fluid from the bursa is needed to find out what bacteria it is and to choose the right antibiotic.
It’s very important to start antibiotics quickly. This helps avoid serious problems and helps the body get better faster.
Aspiration and Surgical Interventions
In some cases, draining the bursa or removing it surgically is needed. Draining the bursa is often done with ultrasound to guide the needle. Surgery is usually only for cases that don’t get better with other treatments.
These options have their own risks and benefits. Deciding to have these procedures should be done with a doctor’s advice.
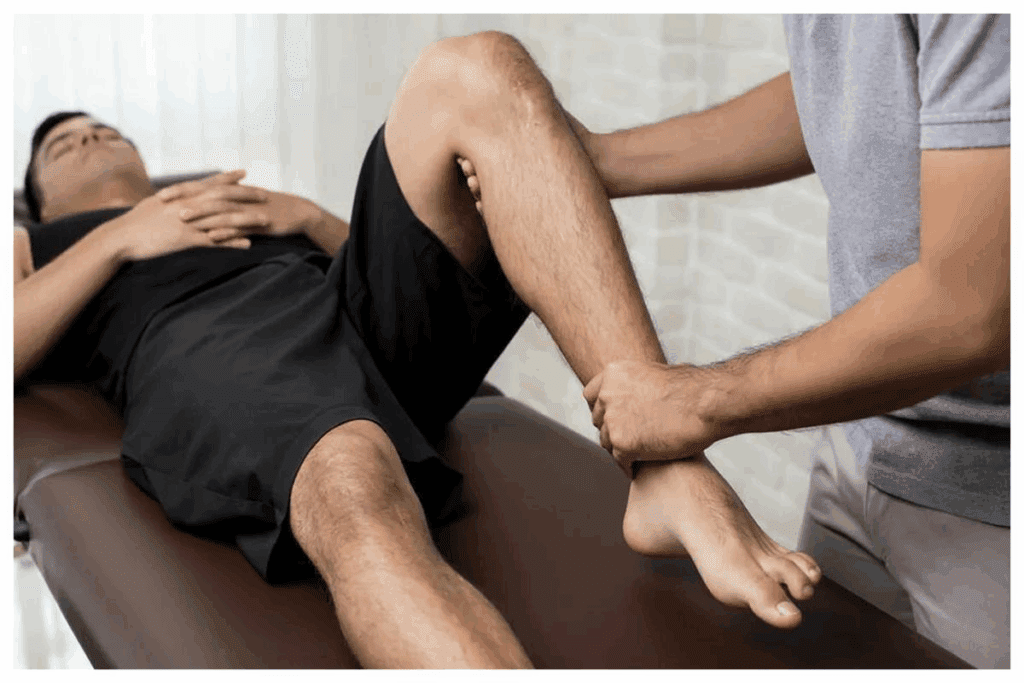
Physical Therapy Approaches for Leg Bursitis
Physical therapy is key in managing leg bursitis. It helps reduce pain and improves function. Leg bursitis can make daily activities hard. Our physical therapy focuses on reducing inflammation, improving mobility, and strengthening the affected areas.
Therapeutic Exercises and Stretches
Therapeutic exercises and stretches are vital for leg bursitis. They improve flexibility, strengthen muscles, and enhance leg function. Key exercises include:
- Stretching exercises to improve flexibility and reduce stiffness in the leg.
- Strengthening exercises to build strong muscles around the affected bursa, providing better support and reducing the risk of further irritation.
- Range of motion exercises to maintain or improve the mobility of the affected joint.
Our physical therapists create a personalized exercise program for each patient.
Manual Therapy Techniques
Manual therapy techniques are essential for leg bursitis. They improve tissue health, reduce pain and inflammation, and enhance mobility. Common techniques include:
- Soft tissue mobilization to reduce muscle tension and promote healing.
- Joint mobilization to improve joint mobility and reduce stiffness.
- Myofascial release to release tension in the fascia surrounding the muscles and joints.
These techniques help patients see significant improvements in their symptoms.
Modalities (Ultrasound, Electrical Stimulation, etc.)
Modalities like ultrasound and electrical stimulation are used to enhance healing and reduce pain. Ultrasound therapy uses sound waves to promote tissue repair and reduce inflammation. Electrical stimulation stimulates muscle contractions, reduces pain, and improves circulation.
Gait Training and Movement Reeducation
Gait training and movement reeducation are vital for patients with leg bursitis. Abnormal gait patterns can worsen bursitis. Our physical therapists assess and improve gait and movement patterns. This may include:
- Gait training to improve walking patterns and reduce stress on the affected bursa.
- Movement reeducation to teach patients how to move more efficiently and safely, minimizing the risk of further irritation.
By addressing these aspects, we help patients regain normal function and reduce future bursitis risk.
Home Remedies and Self-Care for Bursitis Leg Pain
Home remedies and self-care are key to easing bursitis leg pain. They help improve life quality. Simple steps can manage symptoms and lessen flare-ups.
The RICE Protocol
The RICE protocol is a mainstay for bursitis leg pain at home. It stands for Rest, Ice, Compression, and Elevation. Rest the area to avoid more irritation. Use Ice to cut down inflammation. Apply Compression to lessen swelling. And Elevate the leg to boost circulation and ease pain.
Over-the-Counter Pain Management
OTC pain relievers like NSAIDs can help with bursitis leg pain. But, it’s important to stick to the dosage and talk to a doctor, mainly for long-term use.
Supportive Devices and Braces
Supportive devices and braces offer extra relief. They reduce strain on the bursae. For example, knee or hip braces can stabilize the joint and lessen irritation.
Activity Modification Strategies
Changing activities to avoid making the pain worse is essential. This might mean adjusting workouts, resting often, and avoiding certain positions.
By using these home remedies and self-care tips, people can manage their bursitis leg pain better. This improves their overall life quality.
Preventing Bursitis Recurrence in the Leg
It’s important to prevent bursitis from coming back if you’ve had it before. Knowing why it happens is key to keeping your legs healthy. We’ll look at ways to stop it from coming back, like using the right body mechanics and wearing protective gear.
Proper Body Mechanics and Ergonomics
Good body mechanics and ergonomics are vital. They help you stay in the right position during daily tasks and work. Ergonomic adjustments at work, like the right chair and monitor, can help a lot. It’s also good to stretch and move around, even if you sit or stand a lot.
Protective Equipment for Activities
Wearing the right gear can prevent bursitis from coming back. Athletes and sports players should use knee and elbow pads. Padding and bracing offer extra support and protection.
Strengthening and Flexibility Programs
Strengthening and flexibility exercises are important. Doing exercises that make the muscles around the joint stronger helps. Flexibility exercises like stretching also help with movement and reduce stiffness.
Lifestyle Modifications for Long-term Prevention
Changing your lifestyle is key to preventing bursitis from coming back. Keeping a healthy weight helps reduce joint pressure. Also, doing low-impact activities like swimming or cycling keeps joints moving without too much strain.
When to Seek Medical Attention for Leg Pain
Leg pain is not something to ignore. Knowing when to see a doctor is key. Some pain might go away with rest, but other signs mean you need to see a doctor right away.
Red Flag Symptoms That Require Immediate Care
Some leg pain symptoms are urgent. These include:
- Severe pain that doesn’t improve with rest
- Swelling, redness, or warmth around the affected area
- Weakness or numbness in the leg
- Changes in skin color or temperature
- Fever or chills with leg pain
- Recent trauma or injury to the leg
If you notice any of these, get medical help fast.
Differentiating Between Normal and Abnormal Pain Progression
It’s important to know when pain is normal and when it’s not. Normal pain:
- Gets better with rest and self-care
- Is managed with over-the-counter pain meds
- Doesn’t stop you from doing daily things
But abnormal pain might:
- Get worse despite trying to rest and care for it
- Make it hard to do daily activities and sleep
- Be with other symptoms like numbness or tingling
If you’re not sure about your pain, talk to a doctor.
Questions to Ask Your Healthcare Provider
When you see a doctor for leg pain, have questions ready. Ask:
- What might be causing my leg pain?
- What tests do I need to find out the cause?
- What treatments are available for my condition?
- Are there lifestyle changes that can help?
- What could happen if I don’t get treated?
These questions help you understand your situation better.
Preparing for Your Medical Appointment
To get the most from your doctor’s visit, prepare well. Here’s how:
- Keep a pain diary to track your pain
- List all your medications and dosages
- Share any past injuries or health issues
- Write down questions for your doctor
Being prepared helps your doctor understand your situation better. They can then give you the right treatment plan.
Patient Experiences: Case Studies of Bursitis Leg Pain Spread
Bursitis leg pain spread is complex. We learn a lot from patient experiences and case studies. These stories help us understand the challenges patients face and what works to manage their pain.
Athletic Injuries and Recovery Stories
Athletes often get bursitis from too much motion and overuse. For example, a pro runner got trochanteric bursitis. This caused severe hip pain that went down his leg.
Thanks to physical therapy, the runner got better. He did exercises and manual therapy to heal. He was able to run again.
Key parts of his recovery were:
- Exercises for the hip and core
- Changing his running to avoid more strain
- Using devices to ease pain while running
Occupational Bursitis Management
Jobs with lots of repetition or pressure can lead to bursitis. A construction worker got prepatellar bursitis, also known as housemaid’s knee. He learned how important it is to change his work and use protective gear.
| Intervention | Outcome |
| Use of knee pads | Reduced pressure on the affected bursa |
| Regular breaks for rest and stretching | Decreased frequency of flare-ups |
| Physical therapy | Improved knee function and reduced pain |
Elderly Patients and Age-Related Bursitis
Older people get bursitis more easily because of age and less mobility. An elderly patient with ischial bursitis showed how gentle exercises and proper seating help. Pain management also played a big role in improving their life.
Important strategies were:
- Gentle stretching to keep flexibility
- Using cushioned seats to ease pressure
- Starting with simple strengthening exercises
Lessons Learned from Chronic Cases
Chronic bursitis teaches us a lot about long-term care. Patients with long-term bursitis leg pain found help in a team effort. This included medical treatment, physical therapy, and changes in their lifestyle.
Important lessons from these cases are:
- The need for a complete treatment plan
- The importance of ongoing education and support for patients
- The role of lifestyle changes in managing long-term symptoms
Conclusion: Managing and Understanding Bursitis Leg Pain
Managing bursitis well means using a mix of medical care, physical therapy, and changes in lifestyle. We’ve looked at what bursitis is, its types, causes, symptoms, and how to treat it. Knowing about bursitis leg pain is key to a good treatment plan.
To tackle bursitis, you need a plan that covers all bases. This includes medicines to reduce inflammation and pain, along with physical therapy. This can include exercises and manual therapy to help ease symptoms.
It’s vital to understand bursitis leg pain and how it affects your daily life. By using a full approach to manage bursitis, you can see better results and avoid long-term pain and damage. Our aim is to give you the knowledge and tools to manage bursitis and enhance your life quality.
FAQ
What is bursitis and how does it affect the leg?
Bursitis is when a bursa, a fluid-filled sac, gets inflamed. This sac cushions joints and reduces friction. In the leg, it can cause pain, swelling, and make it hard to move. It affects areas like the hip, knee, and ankle.
Can bursitis spread down the leg?
Bursitis itself doesn’t spread down the leg. But, the pain from it can spread to other areas. This happens because of inflammation and irritation of tissues around it. Knowing how pain spreads is key to managing symptoms.
What are the common causes of bursitis in the leg?
Causes include repetitive motion, direct trauma, inflammatory conditions, and infection. Activities like running or cycling can increase risk. These activities put stress on joints.
How is bursitis diagnosed?
Doctors use physical exams, imaging like X-rays or MRI, and lab tests to diagnose. They look at symptoms and medical history to find the cause of pain.
What are the treatment options for bursitis in the leg?
Treatments include anti-inflammatory meds, corticosteroid injections, and antibiotics for infections. Physical therapy is also used. Sometimes, aspiration or surgery is needed to manage symptoms and help healing.
How can I prevent bursitis recurrence in the leg?
To prevent it, use proper body mechanics and protective gear. Do exercises to strengthen and stretch. Maintaining a healthy weight and avoiding repetitive stress on joints also helps.
What are the symptoms that mimic bursitis leg pain spread?
Symptoms like sciatica, tendonitis, muscle strains, and vascular conditions can look like bursitis. A detailed diagnosis is needed to find the real cause of symptoms.
When should I seek medical attention for leg pain?
See a doctor if you have severe pain, swelling, or trouble walking. If pain gets worse or doesn’t go away, get medical help to find the cause and get treatment.
How does physical therapy help in managing bursitis?
Physical therapy includes exercises, manual therapy, and modalities like ultrasound. These help reduce pain, improve movement, and strengthen muscles.
What are some home remedies for managing bursitis leg pain?
Home remedies include the RICE protocol (rest, ice, compression, elevation), over-the-counter pain meds, and using supportive devices. Modifying activities to reduce stress on joints also helps.
Can bursitis lead to chronic pain and long-term effects on leg function?
Untreated or poorly managed bursitis can cause chronic pain, changes in movement, muscle weakness, and decreased mobility. Early and effective treatment can prevent these long-term effects.
What are the risk factors for developing bursitis in the leg?
Risk factors include age, certain jobs or sports, medical conditions, and body structure. Knowing these can help prevent and treat bursitis early.
Reference
- Gomez, L. P. (2024). Greater trochanteric pain syndrome. In NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK557433/