Last Updated on November 18, 2025 by Ugurkan Demir

Osteoarthritis is a disease that makes joints hurt, stiff, and swell. Almost half of people over 50 have knee pain, says the National Institute for Health and Care Excellence.
At Liv Hospital, we use advanced methods and care that focuses on the patient for every step in osteoarthritis diagnosis. Finding out if you have osteoarthritis takes a few steps. These include checking how you feel, looking at images, and doing lab tests.
We’ll show you how to find out if you have osteoarthritis. This includes checking how you feel, looking at images, and doing lab tests. Knowing how to diagnose osteoarthritis is key to treating it well.
Key Takeaways
- Diagnosing osteoarthritis needs a few steps.
- Clinical assessment, imaging, and lab tests are key.
- Knowing how to diagnose is important for managing the disease.
- Liv Hospital uses advanced methods for accurate diagnosis.
- We focus on the patient to meet global standards.
Understanding Osteoarthritis: A Complete Overview

To diagnose osteoarthritis well, we need to understand it deeply. This joint disorder affects millions worldwide. Knowing its basics is key for correct diagnosis.
What is Osteoarthritis?
Osteoarthritis is a joint disease where cartilage breaks down. This leads to pain, stiffness, and less mobility. It’s the most common arthritis and often hits weight-bearing joints and those with injuries.
A rheumatologist, says, “Osteoarthritis is more than just wear and tear. It involves genetics, environment, and how joints work.”
Prevalence and Impact
Osteoarthritis is a big health issue worldwide. In the UK, about 10 million people have it. Nearly 30% of those over 45 have knee osteoarthritis on X-rays. In the US, millions are affected too.
| Age Group | Prevalence of Osteoarthritis |
|---|---|
| 45-54 years | 13.9% |
| 55-64 years | 23.1% |
| 65 years and older | 33.6% |
Common Joints Affected
Osteoarthritis hits many joints, but mainly:
- Knees
- Hips
- Hands (mainly the distal interphalangeal joints)
- Spine
Knowing which joints are often affected helps doctors diagnose osteoarthritis better. This way, they can tell it apart from other arthritis types.
By understanding osteoarthritis well, doctors can make better diagnoses. They can then create effective treatment plans for patients.
The Importance of Early and Accurate Diagnosis
Diagnosing osteoarthritis early is very important. It greatly affects a patient’s quality of life. Early diagnosis lets doctors start the right treatments, which can slow the disease.
Benefits of Timely Intervention
Getting a diagnosis early has many benefits. Doctors can suggest targeted exercises and lifestyle changes that help a lot. Exercise is a key treatment for osteoarthritis, and early diagnosis helps make it fit the patient’s needs.
Also, early diagnosis means doctors can use therapies that slow the disease. It helps manage symptoms better. This approach can improve joint function and reduce pain, making life better for patients.
| Benefits of Early Diagnosis | Description |
|---|---|
| Targeted Exercises | Tailored physical activities to improve joint function and reduce pain. |
| Disease-Modifying Therapies | Use of therapies that can potentially slow disease progression. |
| Symptom Management | Better control of osteoarthritis symptoms, improving quality of life. |
Challenges in Osteoarthritis Diagnosis
Diagnosing osteoarthritis can be tough. Symptoms vary a lot among patients. Some feel a lot of pain and trouble moving, while others have little pain despite serious joint damage.
Also, osteoarthritis often happens with other conditions. This makes it hard to tell what’s causing the symptoms. Doctors need to look at the patient’s history, do a detailed physical exam, and use tests to get the diagnosis right.
It’s key for doctors to know these challenges. This helps them make good decisions and give the best care to patients with osteoarthritis.
Clinical Presentation of Osteoarthritis
It’s important to know how osteoarthritis shows up to diagnose and treat it well. This condition affects people in different ways.
Common Symptoms and Warning Signs
Osteoarthritis often causes joint pain, stiffness, and swelling. These signs can make daily tasks hard. Joint pain usually gets worse with more activity and feels better when you rest.
Other symptoms include:
- Morning stiffness that usually lasts less than 30 minutes
- Crepitus or grinding sensation in the joint
- Bony enlargements or deformities
- Reduced range of motion
Symptom Progression Over Time
Osteoarthritis symptoms can get worse slowly, with ups and downs. Knowing this helps doctors plan better treatments and manage patient hopes.
Risk Factors to Consider
Many things can make osteoarthritis more likely or worse. These include:
| Risk Factor | Description |
|---|---|
| Age | Risk goes up after 45 years |
| Obesity | Extra weight stresses joints |
| Previous Joint Injuries | Old injuries or surgery can raise risk |
| Family History | Genetics play a part in some cases |
Knowing these risk factors helps doctors diagnose and treat osteoarthritis better. They can create a plan that fits each patient’s needs.
How to Diagnose Osteoarthritis: The Clinical Approach
To diagnose osteoarthritis, healthcare providers use a detailed clinical strategy. It starts with a thorough initial patient assessment.
Initial Patient Assessment
The first step in diagnosing osteoarthritis is key. We look at the patient’s overall health, medical history, and symptoms to spot signs of osteoarthritis. This detailed check helps us choose the right diagnostic steps.
Key Questions in Patient History
In taking a patient’s history, we concentrate on important areas to get the right info:
- How long have symptoms lasted and how have they changed?
- Have there been any past injuries or joint problems?
- Is there a family history of osteoarthritis?
- How do current symptoms affect daily life?
By asking specific questions, we gain important insights into the patient’s situation. This helps us spot any warning signs.
Red Flags That Warrant Further Investigation
Some symptoms and findings mean we need to dig deeper. Red flags include:
- Recent injuries or trauma
- Systemic symptoms like fever or weight loss
- Neurological issues
- Severe pain or swelling
Spotting these red flags lets us adjust our diagnosis plan. We might send the patient for more tests or see a specialist.
Physical Examination Techniques
A thorough physical exam is key in diagnosing osteoarthritis. It helps doctors check how joints work and spot signs of the disease. We’ll look at the methods used to examine osteoarthritis.
Joint-Specific Examination Procedures
When checking for osteoarthritis, we focus on specific joints. The methods used depend on the joint but often include looking, feeling, and checking stability.
For example, when checking the knee, we look for swelling, redness, or shape changes. We also check for tenderness and warmth by feeling the joint. To see if the knee is stable, we do tests like the Lachman test.
Assessing Range of Motion
Checking how much a joint can move is important. We look at both how the joint moves on its own and how it moves when someone else moves it. This helps us see if there’s any pain or stiffness.
If a joint can’t move as much as it should, it might be damaged or inflamed. By comparing the joint’s movement to a healthy one, we can see how much it’s affected.
Identifying Crepitus and Bony Enlargement
Crepitus, or a grating feeling in a joint, is a sign of osteoarthritis. We feel for it when moving the joint. Bony growths, or osteophytes, can also be felt or seen.
Both crepitus and bony growths show that osteoarthritis is advanced. They can really affect how well a joint works and how much pain a person feels.
| Sign | Description | Clinical Implication |
|---|---|---|
| Crepitus | Grating or crunching sensation during joint movement | Indicative of cartilage degeneration |
| Bony Enlargement | Visible or palpable enlargement due to osteophyte formation | Signifies advanced osteoarthritis |
| Reduced Range of Motion | Limitation in joint mobility | Reflects joint damage or inflammation |
By using these physical exam techniques, we can better diagnose osteoarthritis. This helps us understand how severe it is and what treatment is needed.
Standardized Diagnostic Criteria for Osteoarthritis
To accurately diagnose osteoarthritis, healthcare professionals must follow recognized criteria. These criteria help ensure patients get the right care and treatment.
Diagnosing osteoarthritis involves clinical presentation, patient history, and diagnostic tests. The American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) have set guidelines. These guidelines are widely used by healthcare providers.
American College of Rheumatology (ACR) Criteria
The ACR has criteria for osteoarthritis classification. These criteria focus on clinical and radiographic features. They help distinguish osteoarthritis from other joint disorders.
The ACR criteria for knee osteoarthritis include:
- Age over 50 years
- Morning stiffness lasting less than 30 minutes
- Crepitus on active motion
- Bony tenderness
- Bony enlargement
- No palpable warmth
These criteria are used with radiographic findings to confirm the diagnosis.
European League Against Rheumatism (EULAR) Guidelines
EULAR guidelines recommend a diagnosis of osteoarthritis. They emphasize a thorough clinical assessment and imaging studies. The diagnosis should be based on persistent joint pain, physical findings, and radiographic features.
“The diagnosis of osteoarthritis is mainly clinical, supported by radiographic findings.”
Clinical Classification Systems
Clinical classification systems categorize osteoarthritis based on severity and characteristics. The Kellgren-Lawrence grading system is one such system. It classifies osteoarthritis based on radiographic findings.
| Grade | Description |
|---|---|
| 0 | Normal |
| 1 | Doubtful narrowing of joint space and possible osteophytic lipping |
| 2 | Definite osteophytes and possible narrowing of joint space |
| 3 | Moderate multiple osteophytes, definite narrowing of joint space, some sclerosis, and possible deformity of bone contour |
| 4 | Large osteophytes, marked narrowing of joint space, severe sclerosis, and definite deformity of bone contour |
In conclusion, standardized diagnostic criteria for osteoarthritis are key for accurate diagnosis and effective management. By using the ACR criteria, EULAR guidelines, and clinical classification systems, healthcare providers can ensure patients receive the right care.
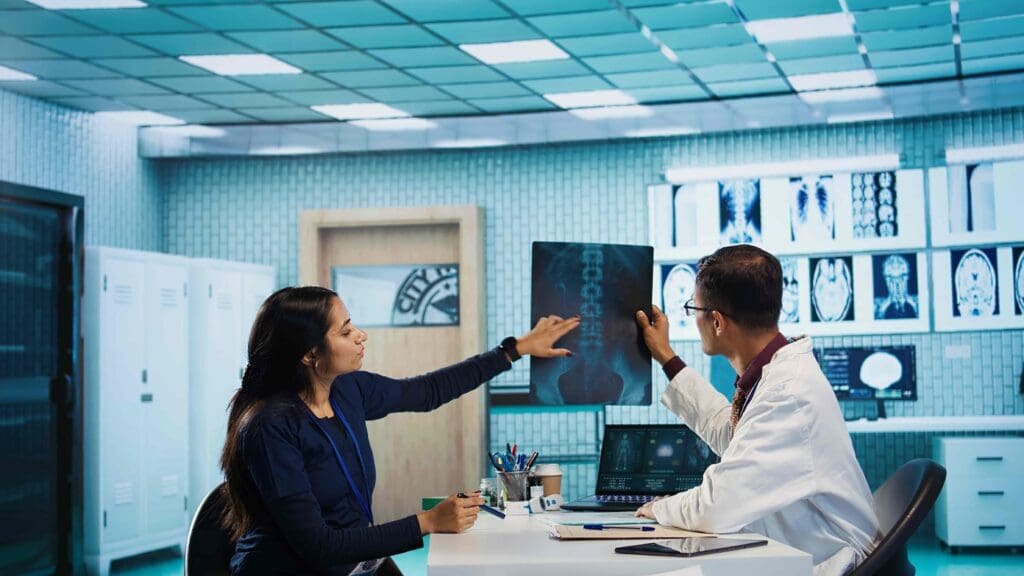
Imaging Studies in Osteoarthritis Diagnosis
Imaging studies are key in diagnosing osteoarthritis. They show joint damage visually. This helps doctors understand how bad the damage is and plan treatment.
X-Ray Findings and Interpretation
X-rays are often used to diagnose osteoarthritis. They show signs like joint space narrowing and osteophyte formation. Joint space narrowing means cartilage loss, and osteophytes are bony growths around the joint.
Doctors look for signs of damage in X-rays. They check for subchondral sclerosis and cysts. These signs mean the osteoarthritis is advanced and help in determining its stage.
When to Use MRI
MRI is not usually needed for osteoarthritis but is helpful in complex cases. It shows detailed images of soft tissues like cartilage, ligaments, and tendons. This helps in a full assessment of joint health.
We suggest MRI when soft tissue damage needs to be checked or X-rays are unclear. It can also spot other conditions that might look like osteoarthritis.
Other Imaging Modalities: CT and Ultrasound
Other imaging tools like CT and ultrasound also help in diagnosing osteoarthritis. CT scans show bone details and can spot small changes in joints.
Ultrasound is good for checking soft tissue inflammation and finding effusions. It’s great for guiding injections and other procedures.
Kellgren-Lawrence Grading System
The Kellgren-Lawrence grading system is used to classify osteoarthritis severity on X-rays. It goes from Grade 0 (normal) to Grade 4 (severe).
This system makes diagnosing and staging osteoarthritis easier. It helps doctors talk about cases clearly and decide on treatments.
Laboratory Tests for Differential Diagnosis
Laboratory tests are key in figuring out what’s wrong with your joints. They help doctors tell osteoarthritis apart from other joint diseases. Even though osteoarthritis is mostly diagnosed through physical checks and imaging, lab tests are vital. They help rule out other conditions that might look like osteoarthritis.
Role of Blood Tests
Blood tests are a big part of diagnosing osteoarthritis. There’s no single blood test for osteoarthritis, but these tests can rule out other joint pains. Some important blood tests include:
- Rheumatoid Factor (RF) and Anti-CCP Antibodies: These tests spot rheumatoid arthritis, an autoimmune disease that can look like osteoarthritis.
- Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP): These tests show if there’s inflammation, which can point to other joint diseases.
- Uric Acid Levels: This test checks for gout, a condition with high uric acid and joint pain.
Synovial Fluid Analysis
Looking at the fluid in your joints is another way to diagnose osteoarthritis. It helps doctors tell osteoarthritis apart from other joint problems. Here’s how it works:
- Aspiration of Synovial Fluid: A sterile needle takes fluid from the joint.
- Analysis of Fluid Characteristics: The fluid is checked for color, clarity, and if it has crystals or cells.
In osteoarthritis, the fluid is usually normal or a bit thick. It might have a few white blood cells. But in inflammatory arthritis, there are more white blood cells.
Biomarkers in Osteoarthritis
Scientists are working on finding biomarkers for osteoarthritis. They want to find markers that can spot osteoarthritis early and track how it changes. Some possible biomarkers are:
- Collagen Fragments: These are pieces of collagen that show cartilage breakdown.
- Inflammatory Mediators: Some inflammatory chemicals might be higher in osteoarthritis.
These biomarkers are promising, but they’re not used in diagnosis yet. More research is needed.
Differentiating Osteoarthritis from Other Joint Conditions
It’s important to tell osteoarthritis apart from other joint diseases for better treatment. Osteoarthritis and other conditions share similar symptoms, making it hard to diagnose correctly.
Rheumatoid Arthritis vs. Osteoarthritis
Rheumatoid arthritis (RA) and osteoarthritis (OA) are two different conditions. OA is caused by wear and tear of the cartilage. RA, on the other hand, is an autoimmune disease that causes inflammation and can damage joints severely if not treated.
The main differences between RA and OA are:
- Symmetry: RA usually affects both sides of the body, while OA can be uneven.
- Morning Stiffness: RA causes longer morning stiffness, whereas OA’s stiffness is shorter.
- Systemic Symptoms: RA can cause fatigue and fever, which OA does not.
Gout and Pseudogout
Gout and pseudogout can be mistaken for osteoarthritis because of similar symptoms. Gout is caused by crystals in the joints leading to sudden inflammation. Pseudogout is caused by different crystals.
What sets gout and pseudogout apart from OA is:
- Acute Onset: Gout and pseudogout have sudden, severe pain and swelling.
- Inflammatory Signs: Both show signs of inflammation like redness and swelling.
- Crystal Presence: Finding specific crystals in the fluid confirms the diagnosis.
Other Inflammatory Arthropathies
Conditions like psoriatic arthritis and ankylosing spondylitis can also mimic osteoarthritis. These conditions cause inflammation and can damage joints over time.
What makes them different is:
- Skin and Nail Changes: Psoriatic arthritis often comes with skin and nail psoriasis.
- Spinal Involvement: Ankylosing spondylitis mainly affects the spine, but can also involve other joints.
- Family History: Many of these conditions run in families.
Getting a correct diagnosis is key. It involves looking at the patient’s history, doing a physical exam, and running tests. By accurately identifying the condition, doctors can provide the right treatment to help patients.
Special Considerations in Specific Populations
Diagnosing osteoarthritis in different groups is key to good care. We must look at the patient’s age and health history. This helps us tailor the diagnosis and treatment.
Diagnosing Osteoarthritis in Younger Patients
It’s hard to diagnose osteoarthritis in young people. They might have other reasons for joint pain. We need to think about past injuries or birth defects that could lead to osteoarthritis.
“Younger patients with osteoarthritis often have different symptoms than older ones,” studies say. This makes it harder to diagnose.
Elderly Patients with Multiple Comorbidities
Elderly patients often have many health issues. This makes diagnosing osteoarthritis tricky. We must check their overall health, including diabetes and heart disease.
For example, older patients with kidney problems might need special imaging or medicine. A full check-up is vital for treating osteoarthritis in this group.
Athletes and Individuals with Previous Joint Injuries
Athletes and those with joint injuries are more likely to get osteoarthritis. We need to think about their sports level, past injuries, and surgeries. They might need detailed tests like MRI to see joint damage.
A famous orthopedic surgeon, said, “Early diagnosis and treatment are key for athletes with osteoarthritis.” This shows how important it is to catch it early in this group.
By focusing on these special groups, we can better diagnose osteoarthritis. This leads to more effective treatment plans.
Diagnostic Challenges and Pitfalls to Avoid
Diagnosing osteoarthritis is tricky because it starts slowly and looks like other joint problems. As doctors, we face these challenges to make sure we diagnose and treat it right.
Common Misdiagnoses
Osteoarthritis is often mistaken for other arthritis types or joint issues. This mistake leads to the wrong treatment plans. It’s often confused with rheumatoid arthritis, gout, and pseudogout.
| Condition | Key Differentiating Features |
|---|---|
| Rheumatoid Arthritis | Symmetrical joint involvement, presence of rheumatoid factor, and anti-CCP antibodies |
| Gout | Acute onset, presence of monosodium urate crystals in synovial fluid, and elevated serum urate levels |
| Pseudogout | Presence of calcium pyrophosphate dihydrate crystals in synovial fluid |
When to Refer to a Specialist
It’s important to send patients to specialists if we’re not sure what’s wrong or if treatments don’t work. Specialists can do more tests and offer new treatments.
Indications for Referral:
- Uncertain diagnosis despite thorough evaluation
- Presence of red flags suggesting other serious conditions
- Inadequate response to initial treatment
Addressing Diagnostic Uncertainty
We can reduce uncertainty by doing a detailed check-up and using the right tests. Sometimes, we need to ask for help from specialists. This helps us not miss any possible problems.
Conclusion: Putting It All Together for Accurate Diagnosis
Getting a correct diagnosis of osteoarthritis involves a detailed check-up, imaging, and lab tests. These steps help doctors make a precise diagnosis. This allows for quick and effective treatment.
We’ve looked at how to diagnose osteoarthritis. This includes checking the patient, doing physical exams, and using imaging and lab tests. Each step is important for finding out if someone has osteoarthritis and how bad it is.
Understanding osteoarthritis well is key to making a correct diagnosis. Doctors use specific criteria to make sure they’re right. This helps them tell osteoarthritis apart from other joint problems.
Tests like X-rays, MRI, and fluid analysis from the joint are very helpful. They give doctors the info they need to plan the best treatment. By using all these tests together, doctors can create treatment plans that really work for each patient.
FAQ
REFERENCES
- American Academy of Family Physicians. (2012, January 15). Osteoarthritis: Diagnosis and treatment. American Family Physician, 85(1), 49–56. Retrieved from https://www.aafp.org/pubs/afp/issues/20120101/p49.html American Academy of Family Physicians
- Hopkins Arthritis Center. (n.d.). Diagnostic guidelines for arthritis. Retrieved from https://www.hopkinsarthritis.org/physician‑corner/education/arthritis‑education/diagnostic‑guidelines nhs.uk+1
- National Health Service (NHS). (2023, March 20). Osteoarthritis. Retrieved from https://www.nhs.uk/conditions/osteoarthritis/ nhs.uk