Last Updated on November 4, 2025 by mcelik
About 80% of adults deal with lower back pain at some point. This is often because of degenerative disc disease. It affects the spine, leading to pain and discomfort that can really affect daily life. When other treatments don’t work, surgery might be an option.
Dealing with back pain is tough. There are many treatments, from simple ones to degenerative disc disease surgery and disc hernia operation. The right treatment depends on how bad the condition is and the patient’s health.
Key Takeaways
- Degenerative disc disease is a common condition causing lower back pain.
- Treatment options vary from conservative management to surgery.
- Surgical interventions include degenerative disc disease surgery and disc hernia operation.
- The choice of treatment depends on the condition’s severity and the patient’s health.
- Understanding the available treatments can help patients make informed decisions.
What Is Degenerative Disc Disease?
Degenerative disc disease affects millions worldwide, causing back pain. It changes how our spine works as we age. This can really hurt our quality of life.
The Anatomy of Healthy Spinal Discs
The spine has vertebrae and discs between them. These discs help our spine move and absorb shock. A healthy disc has a tough outer layer and a soft center.
The outer layer supports the spine, and the soft center absorbs shock. Keeping these discs healthy is key to avoiding back problems.
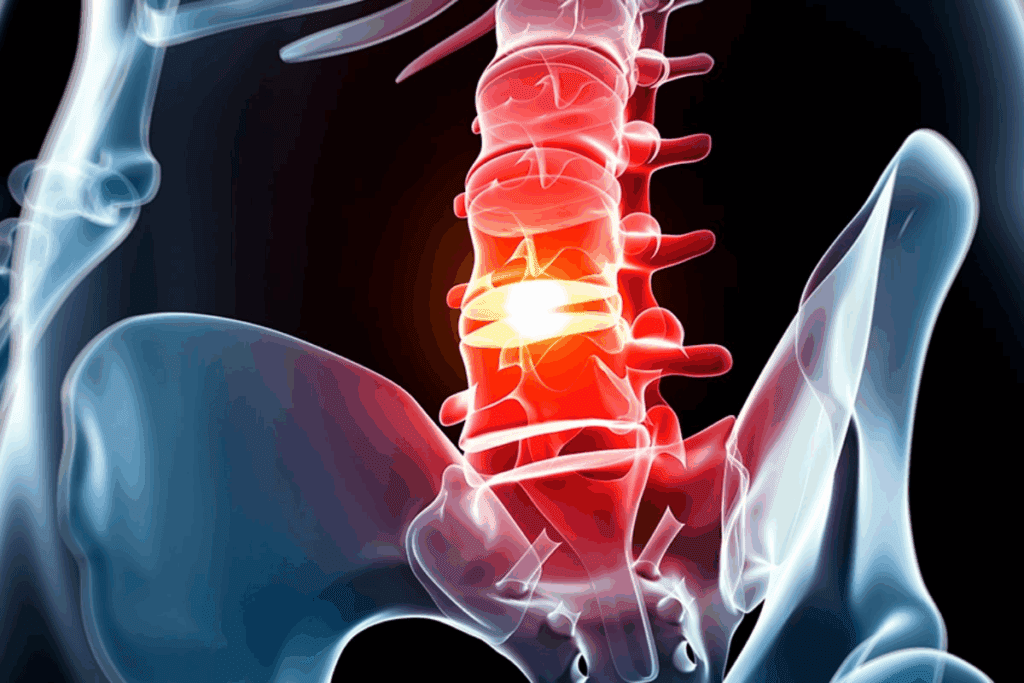
The Degenerative Process Explained
Degenerative disc disease happens when discs wear out. This can cause them to lose water, shrink, and tear. These changes make discs less effective at protecting the spine.
“The degenerative process in the spine is a complex interplay of biochemical, biomechanical, and genetic factors.”
When discs can’t absorb shock well, it puts more stress on the vertebrae. This can lead to pain and swelling.
Common Causes and Risk Factors
Many things can lead to degenerative disc disease. These include:
- Aging
- Genetic predisposition
- Smoking
- Obesity
- Occupational hazards involving heavy lifting or bending
| Risk Factor | Description | Impact on Disc Health |
| Aging | Natural wear and tear over time | Loss of disc hydration and height |
| Smoking | Reduced blood supply to discs | Increased degeneration rate |
| Obesity | Increased stress on spinal discs | Accelerated wear and tear |
Knowing about these risk factors helps prevent and manage the disease. By changing things we can, we might slow down disc degeneration.
Symptoms That Indicate Disc Degeneration
Disc degeneration can cause many symptoms. These include pain, neurological issues, and problems with daily activities. We will look at each of these in more detail.
Pain Patterns and Characteristics
The pain from degenerative disc disease is different for everyone. It can feel like a dull ache or sharp stabbing in the back. Sometimes, the pain spreads to the arms or legs, depending on where the disc is affected.
Common pain patterns include:
- Localized back pain that gets worse with certain movements or positions
- Radiating pain to the extremities, often referred to as radiculopathy
- Pain that gets worse after sitting, standing, or lifting heavy things for a long time
Neurological Symptoms
As disc degeneration gets worse, it can cause nerve problems. These symptoms include:
- Numbness or tingling in the arms or legs
- Muscle weakness, mainly in the arms or legs
- Loss of reflexes in the affected areas
In severe cases, degenerative disc disease can cause serious nerve problems. For example, cauda equina syndrome is a serious condition that needs immediate medical help.
Functional Limitations
The symptoms of degenerative disc disease can make everyday tasks hard. Common problems include:
- Difficulty bending, lifting, or twisting
- Reduced mobility and stiffness in the spine
- Challenges with standing or sitting for a long time
It’s important to understand these symptoms. This helps find the right medical care and ways to manage the condition. It can improve your quality of life.
Diagnosing Degenerative Disc Disease
To diagnose degenerative disc disease, doctors use a mix of clinical judgment, imaging, and sometimes injections. This detailed method is key to figuring out how bad the disease is and what treatment is best.
Clinical Evaluation Process
The first step is a detailed medical history and physical check-up. We look at the patient’s pain, how long they’ve had it, and any nerve problems. This helps us find out what might be causing their pain and guides us to the next steps.
We also check the patient’s movement, reflexes, and muscle strength. Special tests might be done to see if nerves are being pinched. These tests help us understand how much the discs are worn down and how it affects nerves.
Imaging Studies
Imaging tests are key to confirming degenerative disc disease. We usually start with X-rays to see if the spine is aligned right and if there are any big changes. But X-rays can’t show soft tissues like discs well.
For a closer look, we often suggest Magnetic Resonance Imaging (MRI). MRI shows discs, nerves, and soft tissues clearly, helping us see how bad the disc damage is. Sometimes, Computed Tomography (CT) scans are used for detailed bone pictures.
Diagnostic Injections
Diagnostic injections are used in some cases to find the source of pain. These involve putting a local anesthetic in areas like facet joints or around nerves. If the pain goes away, it confirms that area is the problem.
These injections are helpful when tests show several possible pain sources. By blocking pain in specific spots, we can pinpoint the main cause of symptoms. This helps us create a more focused treatment plan.
Non-Surgical Treatment Approaches
There are many non-surgical ways to manage degenerative disc disease. These methods help ease symptoms, improve function, and enhance life quality.
Physical Therapy Interventions
Physical therapy is key in managing degenerative disc disease. Our physical therapists create custom exercise plans. These plans strengthen the muscles around the spine, improve flexibility, and promote good posture.
These exercises help reduce pain and stop further damage. Physical therapy also includes manual therapy like massage and joint mobilization. Heat, cold, and electrical stimulation are used to manage pain and inflammation.
Pain Management Strategies
Managing pain is vital in treating degenerative disc disease. We use various strategies, including medication, lifestyle changes, and alternative therapies.
Our healthcare team works with patients to create a pain management plan. This plan may include medications and lifestyle changes like weight management and stress reduction.
Activity Modification Guidelines
Changing activities to avoid making the condition worse is important. We give patients guidelines for daily activities that don’t stress the spine.
We advise on proper lifting, maintaining a healthy weight, and avoiding heavy bending or twisting. These changes help reduce discomfort and prevent further injury.
By using these non-surgical treatments together, we help patients with degenerative disc disease see big improvements. They feel better and live better lives.
Medication Options for Disc Pain
For those with degenerative disc disease, medication is key in managing pain. Disc-related pain can significantly disrupt daily life, but a variety of treatment options can provide relief.
Over-the-Counter Medications
Over-the-counter (OTC) meds are often the first choice for disc pain. These include:
- Acetaminophen: Good for mild to moderate pain.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Like ibuprofen and naproxen, they cut down inflammation and pain.
Always follow the dosage and talk to a doctor before taking meds for a long time.
Prescription Pain Medications
For more intense pain, prescription meds might be needed. These include:
- Stronger NSAIDs: Prescription versions that are more potent.
- Muscle Relaxants: Helps with muscle spasms from disc degeneration.
- Opioids: For severe pain, but used carefully due to side effects and risk of addiction.
Always use prescription meds under a doctor’s guidance to avoid risks.
Topical Treatments
Topical treatments offer pain relief right where it hurts. These include:
- Topical NSAIDs: Creams, gels, or patches applied to the skin.
- Lidocaine Patches: Numbs the area to ease pain.
- Capsaicin Creams: Made from chili peppers, these creams can lessen pain.
Topical treatments can be used alone or with other pain management plans.
| Medication Type | Examples | Use |
| Over-the-Counter | Acetaminophen, Ibuprofen | Mild to moderate pain |
| Prescription | Stronger NSAIDs, Muscle Relaxants, Opioids | Moderate to severe pain |
| Topical Treatments | Topical NSAIDs, Lidocaine Patches, Capsaicin Creams | Localized pain relief |
Injection Therapies for Degenerative Disc Disease
Injection therapies are a big step forward in treating degenerative disc disease. They aim to lessen pain and swelling, boost function, and maybe dodge surgery.
Epidural Steroid Injections
Epidural steroid injections are a common treatment for degenerative disc disease. They put corticosteroids near the spinal cord to cut down swelling and ease pain. These shots can give a lot of relief to those with pain from the spine or who haven’t gotten better with other treatments.
Benefits: Less swelling, pain relief, and they’re not very invasive.
Facet Joint Injections
Facet joint injections target the facet joints, which can get inflamed and hurt because of degenerative disc disease. These shots mix a local anesthetic with a corticosteroid to lessen pain and swelling in the facet joints.
Procedure: The shot goes right into the affected facet joint under imaging guidance.
Medial Branch Blocks
Medial branch blocks are diagnostic shots used to figure out if the pain comes from the facet joints. By numbing the nerves that supply the facet joints, doctors can find out where the pain is coming from. This helps decide if treatments like radiofrequency ablation are needed.
Purpose: Diagnostic, to find out where the pain is.
Regenerative Medicine Injections
Regenerative medicine injections, like platelet-rich plasma (PRP) therapy, are being looked at for their healing abilities in damaged discs. Even though the FDA warns against unapproved regenerative medicine shots, some approved ones might help reduce pain and improve function.
| Therapy Type | Purpose | Benefits |
| Epidural Steroid Injections | Reduce inflammation and pain | Minimally invasive, quick recovery |
| Facet Joint Injections | Reduce pain and inflammation in facet joints | Targets specific pain source, combines diagnostic and therapeutic benefits |
| Medial Branch Blocks | Diagnose facet joint pain | Helps in planning further treatment |
| Regenerative Medicine Injections | Promote healing in damaged discs | Potential for long-term pain relief, minimally invasive |
When Is Degenerative Disc Disease Surgery Recommended?
If conservative treatments don’t help, surgery might be needed. We look at how bad the symptoms are, how they affect daily life, and if there are nerve problems.
Indicators of Failed Conservative Treatment
Conservative treatment fails if pain and limited movement don’t get better. This includes physical therapy, pain management, and changing activities. We check for:
- Persistent pain that interferes with daily activities
- Lack of improvement in functional abilities
- Ongoing neurological symptoms such as numbness or weakness
If these signs are there, surgery might be the next step.
Progressive Neurological Deficits
Neurological problems getting worse are a big worry. Symptoms like numbness, weakness, or bladder issues mean nerves are being squeezed. We watch for these signs and adjust treatment plans.
“Timely surgical intervention can prevent long-term neurological damage and improve outcomes for patients with degenerative disc disease.”
Functional Limitation Thresholds
Big problems with daily activities or work are key to thinking about surgery. If degenerative disc disease makes it hard to do everyday things or keep a job, we look at surgery.
Patient Selection Criteria
Choosing the right patients for surgery is important. We look at their health, how bad the condition is, and how well they might recover. We consider:
- The patient’s age and overall health status
- The severity of disc degeneration and associated symptoms
- Previous treatments and their outcomes
- Psychological factors that may influence recovery
By looking at these things, we decide if surgery is right for someone with degenerative disc disease.
Cervical Spine Surgical Options
Surgical options for the cervical spine offer hope for those whose degenerative disc disease hasn’t responded to conservative treatments. It’s key to know the different procedures and their benefits.
Anterior Cervical Discectomy and Fusion (ACDF)
ACDF is a common surgery for cervical spine degenerative disc disease. It removes the damaged disc and fuses the vertebrae to stabilize the spine.
Benefits of ACDF:
- Relief from pain and neurological symptoms
- Stabilization of the spine
- High success rate for fusion
We use ACDF for patients with significant disc degeneration, herniation, or spinal instability. The surgery is done through an anterior (front) approach.
Cervical Artificial Disc Replacement
Cervical artificial disc replacement is a motion-preserving option instead of fusion. It replaces the damaged disc with an artificial one, allowing for natural spine movement.
| Procedure | Benefits | Indications |
| Cervical Artificial Disc Replacement | Preserves motion, reduces risk of adjacent segment disease | Single-level disc degeneration, minimal facet joint disease |
| Anterior Cervical Discectomy and Fusion (ACDF) | High fusion success rate, relief from pain and neurological symptoms | Multi-level disc degeneration, significant spinal instability |
Posterior Cervical Approaches
Posterior cervical approaches access the spine from the back. These procedures are often used to decompress the spinal cord or nerves.
We consider posterior cervical approaches for patients with specific anatomical issues or when a posterior decompression is necessary. These procedures can be highly effective in relieving pressure on the spinal cord and nerves.
In conclusion, the choice of surgical procedure for cervical spine degenerative disc disease depends on various factors. These include the extent of degeneration, spinal stability, and patient-specific needs. We work closely with our patients to determine the most appropriate surgical option.
Thoracic Disc Disease Interventions
Thoracic disc disease treatments have grown, giving patients many surgical choices. We know treating this disease well means looking at each patient’s unique spine details.
Unique Challenges of Thoracic Disc Surgery
Surgery in the thoracic area is tough because of its anatomy and close location to vital organs. The spine’s limited movement and the rib cage’s presence make it hard to get to.
Key challenges include:
- Navigating the complex anatomy
- Managing risks associated with proximity to vital organs
- Addressing the limited mobility of the thoracic spine
Surgical Approaches to the Thoracic Spine
There are many surgical ways to go, each suited for different needs. The right method depends on the disc’s spot, the patient’s health, and the surgeon’s skill.
| Surgical Approach | Indications | Benefits |
| Posterior Approach | Herniated discs, spinal stenosis | Less invasive, quicker recovery |
| Anterior Approach | Central disc herniations, vertebral body lesions | Direct access to the disc, better visualization |
| Lateral Approach | Paracentral disc herniations | Avoids major vessels and organs, less muscle disruption |
Minimally Invasive Options for Thoracic Discs
Minimally invasive surgery (MIS) has changed how we treat thoracic disc disease. MIS cuts down on tissue damage, scarring, and speeds up recovery.
Benefits of MIS include:
- Smaller incisions
- Less muscle disruption
- Reduced risk of complications
- Faster return to normal activities
As spinal surgery techniques improve, treating thoracic disc disease will get even better. This means better results and a better life for patients.
Lumbar Degenerative Disc Disease Surgery
When other treatments don’t work, surgery might be needed for lumbar degenerative disc disease. This choice is big, and we’re here to help you understand your options.
Microdiscectomy Procedure
A microdiscectomy is a small surgery to remove a part of a herniated disc. It’s less invasive than older methods, with a smaller cut and less damage. We use the latest tools and techniques for the best results.
This surgery helps you recover faster and feel less pain afterward. It’s a good choice for those who haven’t gotten better with other treatments.
Lumbar Fusion Procedures
Lumbar fusion joins two or more vertebrae together. It uses bone grafts and sometimes rods or screws. This makes the spine more stable and can lessen pain from abnormal movement.
There are several ways to do lumbar fusion, like PLIF and TLIF. We pick the best one for you based on your condition and health.
Lumbar Artificial Disc Replacement
Lumbar artificial disc replacement keeps the spine moving by replacing a damaged disc with an artificial one. It’s designed to keep the spine flexible, which might lower the chance of problems at other segments.
This surgery is for those with just one bad disc. We check each patient to see if this is the right choice for them.
Every surgery has its own good points and possible downsides. We talk with our patients to find the best surgery for their needs and situation.
Minimally Invasive Spine Surgery Techniques
Spine surgery has made big strides with new, less invasive methods. These methods aim to cause less damage, speed up recovery, and improve results for patients.
Endoscopic Discectomy
Endoscopic discectomy uses an endoscope to see the disc and nearby areas. It removes damaged disc parts through a small cut, harming less tissue.
Benefits of Endoscopic Discectomy: It often means less pain after surgery, shorter hospital stays, and quicker getting back to daily life than old methods.
Tubular Retractor Systems
Tubular retractor systems are tools in spine surgery. They use dilators to make a small path to the spine. This path lets surgeons use instruments without big cuts.
Advantages: Tubular retractors cause less muscle damage. This leads to faster healing by keeping more of the body’s natural structure intact.
Percutaneous Fixation Methods
Percutaneous fixation uses small cuts to place screws and rods for spine stability. It’s often paired with other minimally invasive surgeries.
Key Benefits: It stabilizes the spine with less tissue harm. This can mean less pain after surgery and quicker healing.
Benefits of Minimally Invasive Approaches
These new spine surgery methods have big advantages over old ways. They lead to less blood loss, less pain, and shorter hospital stays. These benefits help patients get back to their lives faster and feel happier with their care.
| Technique | Description | Benefits |
| Endoscopic Discectomy | Removal of damaged disc material using an endoscope | Less post-operative pain, shorter hospital stay |
| Tubular Retractor Systems | Minimally invasive access to the spine using tubular retractors | Minimizes muscle damage, promotes faster recovery |
| Percutaneous Fixation | Stabilization of the spine through small incisions | Reduced tissue disruption, less post-operative pain |
Emerging Technologies in Disc Treatment
Treatment for degenerative disc disease is getting better with new technologies. We’re learning more about spinal health and finding new ways to tackle disc problems.
Next-Generation Artificial Discs
New artificial discs are being made to act like real spinal discs. They’re designed to last longer and wear less, which could help patients more. These discs use advanced materials and designs to fit better with the body.
These new discs are tested a lot to make sure they’re safe and work well. Doctors are doing studies to see how they help different people.
Annular Repair Technologies
Technologies for fixing the annulus fibrosus are important for treating disc disease. The annulus is the outer part of the disc that can get damaged. Fixing it might stop the disc from getting worse and make other treatments work better.
There are many ways to fix the annulus, like stitching it or using special materials that help it heal. These ideas could make disc treatments last longer and need fewer surgeries.
Biologics for Disc Regeneration
Biologics for fixing discs are a new area of research. They try to get the body to heal damaged disc tissue on its own. This could help discs work better again.
Scientists are studying these treatments to see if they’re safe and effective. It’s important to test them well before they’re used widely.
Motion Preservation Innovations
Innovations for keeping the spine moving are being developed. These include new kinds of artificial discs and other implants. They help the spine stay flexible, which can reduce stress on other parts of the spine.
Creating these technologies requires understanding how the spine works. As they improve, they offer hope for people who want to stay active despite disc disease.
Recovery After Degenerative Disc Disease Surgery
Patients who have surgery for degenerative disc disease go through a detailed recovery plan. This plan covers immediate care after surgery, a rehabilitation program, and how to get back to work and daily activities.
Immediate Post-Operative Care
The first part of recovery is key. Patients stay in a recovery room for a few hours before going home. It’s vital to follow the doctor’s instructions to recover well. These instructions might include:
- Rest and Activity Modification: Avoiding heavy lifting, bending, or strenuous activities.
- Pain Management: Using prescribed medications to manage pain effectively.
- Wound Care: Keeping the surgical site clean and dry to prevent infection.
Rehabilitation Process
The rehabilitation phase is a big part of getting better after surgery. A good rehab program helps regain strength, improve flexibility, and keep the spine healthy. Our rehab includes:
- Physical Therapy: Tailored exercises to improve mobility and strength.
- Gradual Return to Activities: Progressively increasing activity levels to return to normal functioning.
- Education on Body Mechanics: Learning proper techniques to prevent future injuries.
Return to Work Considerations
Going back to work after surgery is a big step. The timing and how to get back to work depend on the surgery type, job demands, and health. We look at several things when advising on returning to work:
- Job Demands: Assessing the physical demands of the job and determining necessary modifications.
- Workplace Accommodations: Identifying possible accommodations for a smoother return to work.
- Gradual Return: Starting with part-time hours or modified duties to ease back into work.
By managing recovery well, including immediate care, rehab, and work return, patients can get the best results from surgery.
Potential Risks and Complications
It’s important to know the risks of degenerative disc disease surgery before making a decision. Surgery can help many people, but it’s not without risks.
Surgery-Specific Complications
Degenerative disc disease surgery has its own set of risks. These include nerve damage, infection, and bleeding. Sometimes, the surgery may not solve all symptoms, or new ones might appear.
Nerve damage is a big worry because nerves are near the surgery area. Though rare, it can cause numbness, tingling, or paralysis. Careful planning and precise surgical techniques are key to lowering this risk.
Long-term Considerations
After recovery, there are long-term things to think about. These include faster degeneration of discs near the surgery area. There’s also a chance of hardware failure if instruments were used.
- Adjacent segment disease
- Hardware failure
- Recurrent disc herniation
Regular check-ups with your doctor are vital to watch for these long-term issues.
Strategies to Minimize Complications
To lessen surgery risks, several steps can be taken. Choosing an experienced surgeon is critical, as their skill matters a lot. Following post-op instructions and doing physical therapy can also help.
Living a healthy lifestyle, with a good diet and exercise, can also help your spine. This might lower the chance of future problems.
Long-term Outcomes of Disc Treatments
It’s important for patients to know about the long-term effects of disc treatments before they decide on spine surgery. We see that success is not just about pain relief. It also means better quality of life and being able to function well again.
Quality of Life Improvements
Improving a patient’s quality of life is a main goal of disc treatment. Research shows that successful surgery can greatly improve daily activities and social life. Patients often feel better mentally and see a drop in anxiety and depressionafter surgery.
Pain Relief Expectations
Pain relief is a big part of what patients hope for from disc treatments. While results can vary, most patients see a big drop in pain after surgery. How much pain relief they get can depend on the surgery type and their health before surgery.
Functional Recovery Statistics
Being able to function well again is another key success factor. Many patients get back to their pre-disease level of function after surgery. Rehabilitation is key in this process, with special physical therapy helping patients recover fully.
Factors Affecting Surgical Success
Several things can affect how well disc treatments work in the long run. These include the patient’s health, any other health issues, and following the rehab plan after surgery. Choosing the right surgery for each patient is also very important for the best results.
By knowing these factors and what to expect, patients can make better choices about their care. This leads to better long-term outcomes.
Conclusion
Degenerative disc disease is a complex condition that needs a detailed treatment plan. We’ve looked at non-surgical and surgical options like physical therapy, medication, and spine surgery.
A treatment plan for degenerative disc disease should be made just for you. It considers how bad your symptoms are, your health, and your lifestyle. Spine surgery has helped many people feel better and live more comfortably.
Effective treatment for degenerative disc disease combines different approaches. This way, each person gets a plan that fits their needs. Knowing about these options helps patients choose the best care for themselves.
We’ve talked about the importance of a mix of treatments for degenerative disc disease. This includes both non-surgical and surgical methods. Such a plan helps doctors give care that’s just right for each patient, leading to better health and happiness.
FAQ
What is degenerative disc disease?
Degenerative disc disease happens when spinal discs lose their cushioning. This leads to pain and discomfort. It’s a natural aging process but can be made worse by other factors.
What are the symptoms of degenerative disc disease?
Symptoms include back pain, stiffness, and limited mobility. It can also cause numbness, tingling, or weakness in the arms or legs.
How is degenerative disc disease diagnosed?
Doctors use a mix of clinical checks, MRI or CT scans, and diagnostic injections to find the pain’s source.
What are the non-surgical treatment options for degenerative disc disease?
Non-surgical treatments include physical therapy, pain management, and changing activities. Medications like over-the-counter pain relievers and prescriptions are also used.
When is surgery recommended for degenerative disc disease?
Surgery is considered when other treatments don’t work. It’s also needed for progressive neurological issues or significant mobility problems.
What are the surgical options for degenerative disc disease?
Surgical options include discectomy, spinal fusion, and artificial disc replacement. Minimally invasive techniques like endoscopic discectomy are also used.
What is the recovery process like after degenerative disc disease surgery?
Recovery involves immediate care, rehabilitation, and planning for returning to work. The specifics depend on the surgery type.
What are the possible risks and complications of degenerative disc disease surgery?
Risks include surgery-specific issues, long-term effects, and the chance of infection, nerve damage, or hardware failure.
Can degenerative disc disease be prevented?
While it’s a natural aging process, a healthy lifestyle can reduce its risk. This includes regular exercise and a balanced diet.
What are the long-term outcomes of degenerative disc disease treatment?
Long-term outcomes can include better quality of life, pain relief, and improved function. Success depends on the condition’s severity and treatment effectiveness.
Are there any emerging technologies for treating degenerative disc disease?
Yes, new technologies include advanced artificial discs, annular repair, and biologics for disc regeneration. These aim for more effective and less invasive treatments.
Reference
- Koopman, A., & Spiegl, U. J. (2012). Diagnostic testing for degenerative disc disease. International Journal of Research in Orthopaedics, 1(3), 1–6. https://pmc.ncbi.nlm.nih.gov/articles/PMC3401540/