Last Updated on November 20, 2025 by Ugurkan Demir
Beta thalassemia is a hereditary blood disorder. It happens because of mutations in the beta-globin gene. This leads to less or no beta hemoglobin chains being made. Learn 12 key beta thalassemia causes. Understand the crucial diagnostic features of this serious blood disorder you should know.
This genetic disorder affects how hemoglobin is made. Hemoglobin is a protein in red blood cells. It carries oxygen to the body’s tissues.
At Liv Hospital, we focus on the patient. We use leading expertise and new diagnostic methods. This helps us give accurate thalassemia assessment and care that fits each person.
Knowing how beta thalassemia starts is key. It helps us diagnose and manage it well.
Key Takeaways
- Beta thalassemia is caused by genetic mutations affecting hemoglobin production.
- Diagnostic features include variable outcomes ranging from asymptomatic to severe anemia.
- Liv Hospital offers patient-centered care with advanced diagnostic techniques.
- Understanding the genetic basis is key to managing the condition.
- Personalized care is essential for effective management of beta thalassemia.
What Is Beta Thalassemia: Essential Background

Beta thalassemia is a genetic disorder that affects how red blood cells make hemoglobin. This protein is key for carrying oxygen. The condition happens because of mutations in the beta-globin gene. This leads to less or no beta-globin chains in hemoglobin.
Definition and Types of Beta Thalassemia
Beta thalassemia impacts hemoglobin production. There are various types, mainly based on how severe the condition is. The main difference is between beta thalassemia major vs minor. Heterozygous beta thalassemia (minor) causes mild symptoms. On the other hand, homozygous mutations (major) result in severe anemia that needs frequent blood transfusions.
Global Distribution and At-Risk Populations
Beta thalassemia is common in people from the Mediterranean, Middle Eastern, Southern Asian, and African regions. It’s linked to the history of malaria in these areas. The genetic mutations that cause thalassemia help protect against malaria. Knowing the global distribution of beta thalassemia and who is at risk is vital for health programs and genetic counseling.
Primary Beta Thalassemia Causes: Genetic Mutations

Mutations in the beta-globin gene are the main cause of beta thalassemia. This leads to less or no beta hemoglobin chains being made. Beta thalassemia is a genetic disorder that affects how the beta-globin chains of hemoglobin are made. Hemoglobin is key for carrying oxygen in red blood cells.
Point Mutations in the Beta-Globin Gene
Over 350 mutations can cause beta thalassemia, with about 20 causing 80% of cases. Point mutations change a single DNA base in the beta-globin gene. These changes can cause different types of beta thalassemia, like a complete loss of beta-globin production (β) or a reduced production (β).
Deletions and Other Genetic Abnormalities
Deletions and other genetic issues can also lead to beta thalassemia. Deletions remove part of the beta-globin gene, causing a loss of function if big enough. Other problems include mutations that mess up the beta-globin gene’s splicing or make abnormal beta-globin mRNA.
Inheritance Patterns and Family Risk
Beta thalassemia is inherited in an autosomal recessive pattern. This means you need two mutated alleles to have the major form of the disease. Carriers, with one normal and one mutated allele, usually don’t show symptoms but can pass the mutated gene to their kids. Knowing how it’s inherited is key for genetic counseling and understanding family risk.
Pathophysiology of Beta Thalassemia
Beta thalassemia happens when the body can’t make enough beta-globin chains. This lack causes a chain of problems leading to anemia and other issues.
Alpha/Beta Chain Imbalance Mechanism
The main problem in beta thalassemia is the imbalance between alpha and beta globin chains. Alpha chains are made normally, but beta chains are not. This imbalance makes alpha chains toxic to red blood cells.
Ineffective Erythropoiesis Process
In beta thalassemia, the bone marrow tries to make more red blood cells to fight anemia. But, it fails because the cells die off. This makes the bone marrow grow too much, causing bone deformities.
Chronic Hemolysis and Its Effects
Chronic hemolysis is a big part of beta thalassemia. The imbalance between alpha and beta chains makes red blood cells break down. This leads to anemia and other problems like a big spleen, jaundice, and more infections.
The main points of beta thalassemia’s pathophysiology are:
- Imbalance between alpha and beta globin chains
- Ineffective erythropoiesis leading to anemia and bone marrow expansion
- Chronic hemolysis resulting in hemolytic anemia and related complications
Beta Thalassemia Major vs Minor: Critical Distinctions
The main difference between beta thalassemia major and minor is in their genetic makeup and severity. Beta thalassemia major, also known as Cooley’s anemia, is a severe form that needs lifelong medical care. On the other hand, beta thalassemia minor is milder and usually doesn’t need much medical help.
Heterozygous Beta Thalassemia (Minor Form)
Heterozygous beta thalassemia, or beta thalassemia minor, happens when someone has one mutated beta-globin gene. This condition causes mild anemia and often doesn’t show many symptoms. People with beta thalassemia minor usually live a normal life and don’t need regular transfusions or intense treatments.
Key characteristics of beta thalassemia minor include:
- Mild microcytic anemia
- Minimal or no symptoms
- No significant impact on quality of life
Homozygous Beta Thalassemia (Major Form)
Homozygous beta thalassemia, or beta thalassemia major, occurs when someone has two mutated beta-globin genes. This severe form causes serious anemia, growth issues, and other problems. People with beta thalassemia major need regular blood transfusions and chelation therapy to manage iron buildup.
Common complications associated with beta thalassemia major include:
- Severe anemia requiring regular transfusions
- Skeletal deformities due to bone marrow expansion
- Growth retardation and delayed puberty
Intermediate Thalassemia Characteristics
Intermediate thalassemia falls between beta thalassemia major and minor. It has a range of anemia levels and might need occasional transfusions. The treatment for intermediate thalassemia depends on the person’s specific needs and how they’re doing.
Management strategies for intermediate thalassemia may include:
- Occasional blood transfusions
- Monitoring for complications
- Supportive care to improve quality of life
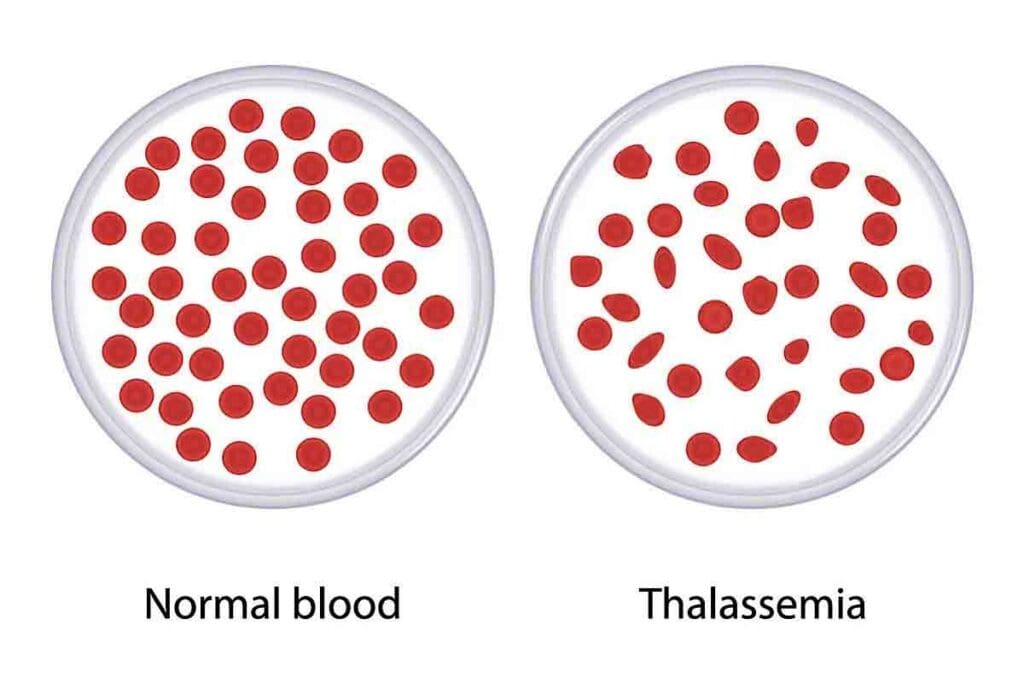
Diagnostic Feature #1: Thalassemia Microcytic Anemia
Thalassemia microcytic anemia is a key sign of beta thalassemia. It shows red blood cells that are smaller than usual and have less hemoglobin. This makes them appear pale.
Microcytic Hypochromic Red Cell Morphology
Beta thalassemia causes these small, pale red cells. This happens because of gene mutations that affect hemoglobin production. Without enough hemoglobin, the cells are both small and pale.
Distinguishing from Iron Deficiency Anemia
Thalassemia and iron deficiency anemia both show small, pale red cells. But, they have different causes. Iron deficiency anemia has low iron levels and high TIBC. Thalassemia, on the other hand, has normal or high iron levels.
Complete Blood Count Patterns
A complete blood count (CBC) is key in diagnosing thalassemia. It shows low MCV and MCH, which means the red cells are small and pale.
| CBC Parameter | Typical Finding in Thalassemia |
| MCV (Mean Corpuscular Volume) | Decreased |
| MCH (Mean Corpuscular Hemoglobin) | Decreased |
| MCHC (Mean Corpuscular Hemoglobin Concentration) | Decreased or Normal |
| RDW (Red Cell Distribution Width) | Variable |
The CBC pattern, along with other signs, helps tell thalassemia apart from other anemias.
Diagnostic Feature #2: Beta Thalassemia Blood Smear Findings
Blood smear findings are key in diagnosing beta thalassemia. They show typical changes in red blood cells. A blood smear test is a major tool that helps understand these changes.
Characteristic Peripheral Smear Abnormalities
In beta thalassemia, blood smears often show red blood cells of different sizes and shapes. These changes point to the disease’s cause.
A study in InTech Open found these changes are vital for diagnosis. It shows how important blood smears are in diagnosing beta thalassemia.
Target Cells and Basophilic Stippling
Two key features in beta thalassemia blood smears are target cells and basophilic stippling. Target cells look like a “bull’s eye” because of how hemoglobin is spread. Basophilic stippling shows as small dots in red blood cells, caused by ribosomal RNA.
Nucleated Red Blood Cells in Circulation
Nucleated red blood cells in the blood are another important sign of beta thalassemia. These cells are usually found in the bone marrow. Their presence in the blood shows the body is under stress to make more red blood cells.
| Blood Smear Feature | Description | Significance in Beta Thalassemia |
| Target Cells | Bull’s eye appearance due to hemoglobin redistribution | Characteristic feature of beta thalassemia |
| Basophilic Stippling | Aggregated ribosomal RNA appearing as punctate inclusions | Indicative of disturbed hemoglobin synthesis |
| Nucleated Red Blood Cells | Presence of immature red blood cells in circulation | Signifies erythropoietic stress |
Looking at blood smear findings is essential in diagnosing beta thalassemia. It gives important clues about the disease and helps doctors make a diagnosis.
Diagnostic Feature #3: Hemoglobin Electrophoresis in Beta Thalassemia
Hemoglobin electrophoresis is a key tool for finding and measuring different hemoglobin types. It’s used to spot beta thalassemia in patients. This method is vital for diagnosing and treating the condition.
Principles and Methodology
This test separates hemoglobin types by their charge and other traits. It works by applying a sample to a medium like gel or cellulose acetate. Then, an electric field is applied, causing different hemoglobins to move at different speeds.
Elevated HbF and HbA2 Patterns
In beta thalassemia, the test shows more HbF and HbA2. HbF is a sign of fetal hemoglobin, which stays in adults with beta thalassemia. High HbA2 levels are also common, mainly in beta thalassemia minor.
Interpreting Thalassemia Electrophoresis Results
Understanding hemoglobin electrophoresis results is key. For example, beta thalassemia major shows very high HbF levels. It often has little to no HbA.
Thalassemia Major Hemoglobin Electrophoresis Findings
Beta thalassemia major shows almost all HbF, sometimes up to 100%. HbA is usually very low or missing. HbA2 levels might be high or normal.
Diagnosing beta thalassemia with hemoglobin electrophoresis is essential. It helps doctors create the right treatment plans. Knowing the different hemoglobin patterns helps in managing the condition.
Diagnostic Feature #4: Skeletal and Physical Manifestations
Skeletal abnormalities are a key sign of beta thalassemia major. They help doctors diagnose the condition. Bone marrow grows more to make up for anemia, causing various skeletal issues.
Thalassemia Frontal Bossing Development
Thalassemia frontal bossing is a common sign of beta thalassemia major. It happens when the bone marrow in the skull grows too much. This results in a more prominent forehead and can lead to other facial problems.
Facial and Skeletal Deformities
Facial and skeletal issues are common in beta thalassemia major. Bone marrow growth can cause facial asymmetry and other skeletal problems. These issues can greatly affect a person’s quality of life.
Growth Retardation Patterns
Growth retardation is another big issue in beta thalassemia major. Chronic anemia and bone marrow growth can slow down growth and development in kids. This requires careful management and monitoring.
In summary, the skeletal and physical signs of beta thalassemia major are very important. They include thalassemia frontal bossing, facial and skeletal issues, and growth retardation. These signs are key for managing the condition.
Advanced Diagnostic Approaches for Beta Thalassemia
New diagnostic methods have changed how we find and treat beta thalassemia. These modern tools make diagnosis more accurate and quicker. This helps doctors give better treatment plans.
Genetic Testing and DNA Analysis
Genetic testing is key in diagnosing beta thalassemia. It looks at the HBB gene for mutations. DNA analysis can spot thalassemia carriers and find other genetic issues. This helps with family planning and genetic advice.
Prenatal Diagnosis Methods
Prenatal tests are vital for managing beta thalassemia, mainly for families with a history. Tests like chorionic villus sampling (CVS) and amniocentesis can find beta thalassemia major early. This gives parents the chance to make informed choices.
Emerging Diagnostic Technologies
The world of beta thalassemia diagnosis is always getting better. New technologies promise even more precise and non-invasive tests. Advances in next-generation sequencing (NGS) and other molecular tests will help manage beta thalassemia better.
Conclusion: Importance of Early Diagnosis and Management
Early diagnosis and management are key for those with beta thalassemia. Healthcare providers can create effective plans by understanding the causes and signs of this disorder. This helps improve patient outcomes.
Early diagnosis is very important. It can greatly improve the life quality of those with beta thalassemia. Managing the condition involves regular blood transfusions, iron chelation therapy, and watching for complications.
With a proactive approach, people with beta thalassemia can live full and meaningful lives. New medical technologies and treatments are making a big difference. This shows how vital early diagnosis and ongoing care are.
FAQ
What is beta thalassemia?
Beta thalassemia is a genetic disorder. It affects how red blood cells carry oxygen. This is because of a problem with hemoglobin, a key protein in these cells.
What causes beta thalassemia?
It’s caused by changes in the HBB gene. This gene is important for making the beta-globin part of hemoglobin.
What are the different types of beta thalassemia?
There are a few types. Beta thalassemia major is the most severe. Beta thalassemia minor is milder. There’s also intermediate thalassemia.
How is beta thalassemia diagnosed?
Doctors use several tests to diagnose it. These include a complete blood count and genetic testing.
What is hemoglobin electrophoresis in beta thalassemia?
It’s a test that checks the types of hemoglobin in the blood. It helps doctors diagnose beta thalassemia.
What are the characteristic features of beta thalassemia blood smear findings?
The blood smear shows certain signs. These include small, pale red cells and other abnormalities.
How does beta thalassemia major differ from beta thalassemia minor?
Beta thalassemia major is more severe. It causes serious anemia and other problems. Beta thalassemia minor is milder, with fewer symptoms.
What is thalassemia frontal bossing?
It’s a facial deformity that can happen in beta thalassemia major. It’s due to bone marrow expansion.
Can beta thalassemia be diagnosed prenatally?
Yes, it can be diagnosed before birth. Genetic testing and DNA analysis are used.
What is the role of genetic testing in beta thalassemia diagnosis?
Genetic testing finds the exact cause of beta thalassemia. It helps in accurate diagnosis and planning for families.
How does ineffective erythropoiesis contribute to beta thalassemia?
Ineffective erythropoiesis means red blood cells don’t mature properly. This leads to anemia and other complications in beta thalassemia.
What is the pathophysiology of beta thalassemia?
The imbalance between alpha and beta globin chains is key. This imbalance causes ineffective erythropoiesis and chronic hemolysis, leading to complications.
Reference
- National Center for Biotechnology Information (NCBI): Guidelines for the Clinical Management of Thalassaemia
https://www.ncbi.nlm.nih.gov/books/NBK173968/