Last Updated on November 20, 2025 by Ugurkan Demir
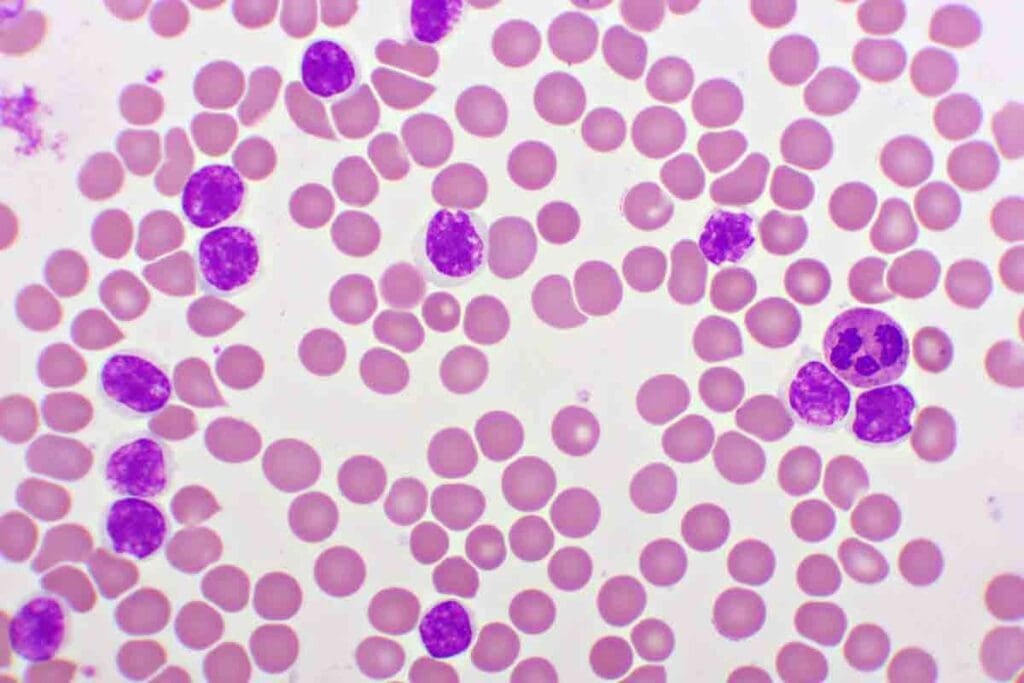
Blast cells in blood are young cells that grow in the bone marrow. Usually, they make up less than 5% of bone marrow cells. They are rarely found in the blood. For more info,
Adult acute myeloid leukemia (AML) is a cancer where the bone marrow makes too many bad blood cells. Knowing about blast cells helps doctors diagnose and treat leukaemia. The number of blast cells in blood and bone marrow shows how the disease is doing.
Key Takeaways
- Blast cells are immature cells that develop into various types of blood cells.
- Normally, blast cells make up less than 5% of bone marrow cells.
- The presence of blast cells in blood is abnormal and may indicate leukaemia.
- Understanding blast cells is key for diagnosing and treating leukaemia.
- Leukaemia remission is closely tied to the blast cell count in bone marrow and blood.
Understanding Blast Cells in Blood

Blast cells are key in making blood cells. They turn into mature cells. These cells help make red blood cells, white blood cells, and platelets.
Definition and Origin of Blast Cells
Blast cells are young cells in the bone marrow. They are the first step to making blood cells. They have a big nucleus and not much cytoplasm.
Origin of Blast Cells: They come from hematopoietic stem cells in the bone marrow. These stem cells can turn into different blood cells. This is important for keeping blood cell counts healthy.
Normal Function in Hematopoiesis
Hematopoiesis is how blood cells are made. Blast cells are important in this process. They grow and change into blood cells.
“The hematopoietic system is a complex and highly regulated system that is responsible for the production of blood cells. Blast cells are an integral part of this process, and their dysregulation can lead to various blood disorders.”
The role of blast cells in hematopoiesis includes:
- Proliferation: Blast cells grow in number.
- Differentiation: They turn into specific blood cell types.
- Maturation: They become functional blood cells.
The table below shows what blast cells are and their role in making blood cells:
| Characteristics | Description |
| Origin | Bone marrow hematopoietic stem cells |
| Function | Precursors to mature blood cells |
| Role in Hematopoiesis | Proliferation, differentiation, and maturation into blood cells |
The Normal Range of Blast Cells
Blast cells are immature blood cells important for making new blood cells. Their numbers are closely watched. In a healthy person, the bone marrow and blood have the right amount of blast cells.
Healthy Blast Cell Percentages in Bone Marrow
In a healthy person, blast cells make up less than 5% of bone marrow cells. This is a key sign that the bone marrow is working right. If there are more, it might mean there’s a problem.
The right balance is kept by growth factors and cytokines. Any change can cause blast cell counts to go off track.
Why Blast Cells Are Normally Absent from Peripheral Blood
Blast cells are usually not found in blood when everything is okay. Finding them in blood often means there’s a blood disease, like leukemia. When they’re not in blood, it shows the bone marrow is doing its job well.
The bone marrow is where these cells grow and get ready to enter the blood.
- Normal blast cell percentage in bone marrow is less than 5%.
- Blast cells are typically absent from peripheral blood.
- The presence of blast cells in peripheral blood can indicate a pathological condition.
Knowing about blast cells helps doctors diagnose and keep track of health issues. It shows how important it is to have the right number of blast cells for good health.
When Blast Cells Become Problematic
Elevated levels of blast cells in the blood often signal a serious condition, such as acute myeloid leukemia (AML). Blast cells are important in making blood cells. But, when they grow too much, it can cause big health problems.
Elevated Blast Cell Counts
Elevated blast cell counts are seen in many blood cancers. In AML, too many myeloblasts can harm the bone marrow. This can lead to anemia, infections, and bleeding problems. It’s key to watch blast cell counts to diagnose and treat these issues.
Disruption of Normal Blood Cell Production
Too many blast cells can mess up blood cell making. The bone marrow gets filled with these immature cells. This stops normal blood cells from being made.
This messes up blood cell production. It can cause anemia, leading to tiredness and weakness. It can also cause bleeding problems.
In short, too many blast cells and the mess they cause are big problems in blood cancers like AML. Knowing about these issues helps doctors diagnose and treat these diseases.
Blast Cells in Leukaemia Diagnosis
Blast cells are key in diagnosing AML. Their number in bone marrow is very important. AML diagnosis uses clinical findings, cell look, and specific criteria.
Diagnostic Criteria for Acute Myeloid Leukaemia (AML)
AML diagnosis focuses on genetic changes and blast cell percentage. A 20% blast threshold in bone marrow is a key factor. It helps tell AML apart from other blood disorders.
Tests like bone marrow aspiration and biopsy are used. Flow cytometry and immunophenotyping help identify cell markers. These tests are vital for AML diagnosis.
The Significance of the 20% Blast Threshold
The 20% blast threshold is important. It shows when a patient’s condition is AML. It’s used with other criteria like genetic mutations and cell look.
| Diagnostic Criteria | Description | Significance |
| Blast Cell Percentage | Percentage of blast cells in bone marrow | 20% or more indicates AML |
| Genetic Abnormalities | Presence of specific genetic mutations | Supports AML diagnosis |
| Morphological Examination | Examination of cell morphology | Helps identify AML subtype |
In conclusion, AML diagnosis depends on blast cell count in bone marrow. The 20% blast threshold is critical. Knowing these criteria helps doctors treat AML patients well.
Types of Blast Cells in Different Leukaemias

Leukaemia types differ based on the blast cells they have. Knowing these differences is key for correct diagnosis and treatment.
Myeloid Blasts in AML
Acute Myeloid Leukaemia (AML) is marked by myeloid blasts. These are young cells that could become different blood cells. They often look and act differently than normal cells.
“The presence of myeloid blasts is a diagnostic hallmark of AML, and their characteristics can influence treatment decisions,” as noted by hematology experts. To identify myeloid blasts, doctors look at their shape, how they stain, and specific markers on their surface.
Lymphoid Blasts in Acute Lymphoblastic Leukaemia (ALL)
Acute Lymphoblastic Leukaemia (ALL) is identified by lymphoid blasts. These cells are on their way to becoming lymphocytes, which are vital for our immune system. Lymphoid blasts in ALL can be either B-cell or T-cell types, depending on their markers.
Diagnosing ALL depends a lot on finding lymphoid blasts. They have specific markers and look a certain way. A leading oncologist says, “Spotting lymphoid blasts is key to diagnosing ALL and planning treatment.”
In short, the blast cells in leukaemia can be very different, like in AML and ALL. Knowing these differences helps doctors create better treatment plans.
White Blood Cell Counts in Leukaemia
Understanding white blood cell counts is key to managing leukaemia well. Leukaemia, a blood and bone marrow cancer, affects these counts. The white blood cell count, or WBC count, shows how well we’re doing health-wise and can be changed by leukaemia.
Understanding AML WBC Count Variations
‘The WBC count at diagnosis can provide valuable information about the disease’s severity and prognosis.’
A high WBC count in AML means the disease might be more aggressive. A low count could mean the bone marrow isn’t working right.
Interpreting High vs. Low WBC Counts
Understanding WBC counts in leukaemia patients is important. A high WBC count might mean leukaemic cells are present, leading to problems like leukostasis. But, a low WBC count can make infections more likely because of neutropenia. Effective management means watching these counts closely and changing treatment as needed.
Laboratory Methods for Blast Cell Detection
Finding blast cells is key to diagnosing and treating leukaemia. Many lab tests are used to spot and count these cells in blood and bone marrow. This is vital for making the right diagnosis and treatment plan.
Blood Smear Analysis
Blood smear analysis is a basic test for finding blast cells. It spreads a blood sample on a slide, stains it, and looks at it under a microscope. A skilled hematologist can spot different cell types and find abnormalities that might mean leukaemia.
“The blood smear is a key tool in hematology,” say experts. It’s a fast and affordable way to check blood cell shapes and find problems.
Bone Marrow Aspiration and Biopsy
Bone marrow tests are vital for diagnosing and tracking leukaemia. These tests take bone marrow samples to look for blast cells. Bone marrow aspiration gets a sample of the liquid part of the marrow, while a biopsy takes a bone tissue core. They give a full view of the marrow’s cells.
- Bone marrow aspiration checks the blast cell percentage.
- A biopsy shows the marrow’s structure and cell density.
Flow Cytometry and Immunophenotyping
Flow cytometry and immunophenotyping are advanced tests for identifying and studying blast cells. Flow cytometry looks at cell characteristics as they pass through a laser. Immunophenotyping uses antibodies to find specific proteins on cell surfaces, helping to classify blast cells and diagnose leukaemia types.
These methods are great for diagnosing acute leukaemias like AML and ALL. They help tell leukaemia types apart and guide treatment choices.
“Flow cytometry has changed hematopathology by making fast and accurate cancer diagnosis possible.”
In summary, tests like blood smear analysis, bone marrow tests, and flow cytometry are key for finding blast cells and diagnosing leukaemia. These tests give vital info for treatment plans and better patient care.
The Role of Blast Cells in Leukaemia Remission
Getting to leukaemia remission is a big win in treatment. It means fewer or no blast cells are seen. Remission means the disease is controlled, and the bone marrow and blood show little to no leukaemic cells.
Doctors check for remission by looking at the bone marrow. They count the blast cells. Complete remission is when the bone marrow has less than 5% blast cells and no leukaemia in the blood or body.
Complete Remission Criteria
To be in complete remission, patients must meet certain criteria. These include:
- Bone marrow blast cell percentage less than 5%
- Absence of leukaemic cells in the blood
- No evidence of extramedullary leukaemia (leukaemia outside the bone marrow)
- Recovery of normal blood cell production
A leading haematologist says, “Complete remission is not just about reducing blast cells; it’s about restoring normal hematopoiesis.”
“The goal of induction therapy is to achieve complete remission, which is a critical step towards long-term survival in leukaemia patients.”
Minimal Residual Disease (MRD)
Even with complete remission, some leukaemic cells might remain. This is called minimal residual disease (MRD). MRD is key in managing leukaemia because it can show the risk of relapse.
Doctors use flow cytometry or PCR to check for MRD. These tests can find leukaemic cells at very low levels. This helps understand the patient’s risk of relapse.
| MRD Status | Implication | Typical Action |
| MRD Negative | Low risk of relapse | Continue with consolidation therapy |
| MRD Positive | Higher risk of relapse | Consider intensification of therapy or targeted treatment |
MRD is a big factor in treatment plans. It shows the need for more or different treatments. Managing MRD is key to better outcomes for leukaemia patients.
In conclusion, blast cells play a big role in leukaemia remission. Getting and keeping complete remission, and watching for MRD, are key to managing leukaemia well.
Monitoring Blast Cells Throughout Treatment
The success of leukaemia treatment depends on monitoring blast cells regularly. This helps check how well the treatment is working and if the disease might come back. Doctors can then adjust the treatment to help patients get better.
Assessment of Treatment Response
Checking how well the treatment is working is key in managing leukaemia. Doctors watch blast cells to see if they’re getting fewer. A study shows this is very important for AML patients.
Good treatment results mean fewer blast cells. But, even a few can mean the disease might come back. So, doctors keep a close eye on blast cells.
Predicting Relapse Through Blast Cell Monitoring
Spotting when the disease might come back is also important. Blast cell counts help doctors see if the disease is coming back early. Studies show that more blast cells often mean the disease is coming back soon.
- Regular monitoring helps catch relapse early.
- Blast cell counts help change treatment plans.
- It also helps manage minimal residual disease (MRD).
In summary, watching blast cells during treatment is key. It helps doctors see how well the treatment is working and if the disease might come back. This way, doctors can make the treatment better and help patients more.
Conclusion
Knowing about blast cells and their part in leukaemia is key for good care. Finding and watching blast cells in blood is vital for treating leukaemia.
We’ve looked at what blast cells are, where they come from, and their role in blood making. We’ve also seen how they play a big part in diagnosing leukaemia, like in AML and ALL.
Blast cells are very important for seeing if leukaemia treatment is working. Watching them helps doctors know if the treatment is a success or if the leukaemia might come back.
Understanding blast cells helps doctors give better care to leukaemia patients. This leads to better treatment results and a better life for patients. Spotting and tracking blast cells is essential for beating leukaemia.
FAQ
What are blast cells in blood?
Blast cells are young cells that can grow into different blood cells. They are key in making blood cells, a process called hematopoiesis.
What is the normal range of blast cells in bone marrow?
In bone marrow, blast cells should be less than 5%. More than this can mean a serious problem, like leukaemia.
Why are blast cells normally absent from peripheral blood?
Blast cells are usually found in the bone marrow. They are young and need to mature into blood cells there.
What is the significance of the 20% blast threshold in AML diagnosis?
For Acute Myeloid Leukaemia (AML), having 20% or more blast cells in blood or bone marrow is key. It’s a sign of AML.
How are blast cells detected in leukaemia diagnosis?
Tests like blood smears, bone marrow aspiration, and flow cytometry find blast cells. These tests help diagnose and track leukaemia.
What is the role of blast cells in leukaemia remission?
Blast cells are important in beating leukaemia. To achieve remission, their numbers must drop a lot. Keeping an eye on them is vital to catch any signs of relapse.
How are WBC counts used in leukaemia diagnosis and treatment?
WBC counts help doctors watch over leukaemia patients. High or low counts can show if the disease is getting worse or if treatment is working.
What is minimal residual disease (MRD) in leukaemia?
Minimal Residual Disease (MRD) means small leukaemia cells stay after treatment. Watching for MRD is key to spotting relapse and planning more treatment.
How are blast cells monitored throughout treatment?
Tests like bone marrow aspiration and flow cytometry keep an eye on blast cells. They help see how well treatment is working and if the disease might come back.
What is the significance of myeloid and lymphoid blasts in leukaemia?
Myeloid and lymphoid blasts are different kinds of cells linked to different leukaemias. Knowing which ones are present helps doctors figure out the type of leukaemia and plan the best treatment.
References
- Cancer.Net Editorial Board. (2023, June 16). Leukemia – Acute Myeloid (AML): Diagnosis. Cancer.Net. American Society of Clinical Oncology (ASCO) via Cancer.Net: https://www.cancer.net/cancer-types/leukemia-acute-myeloid-aml/diagnosis