At Liv Hospital, we know that Acute Disseminated Encephalomyelitis (ADEM) is a rare brain and spinal cord disorder. It causes inflammation and damage to the protective covering of these nerves.
Mostly, ADEM hits kids hard. It can start after they get sick with a virus or after getting vaccinated. This makes it a big worry for families and doctors.
We believe in sharing health info clearly, like Corvelva does. This helps patients and their families learn more about ADEM.
Our team is all about giving the best care for ADEM. We use the latest knowledge and focus on the patient’s needs. This way, we make sure everyone gets the care they need.
Key Takeaways
- ADEM is a rare neurological disorder involving inflammation of the brain and spinal cord.
- It mainly affects kids and often starts after they get sick or get vaccinated.
- Knowing about ADEM is key to managing it well.
- Liv Hospital is committed to giving top-notch care with the latest medical knowledge.
- Putting the patient first is essential in treating ADEM.
What Is ADEM? Definition and Overview
To grasp ADEM, we must explore its complex medical definition and who it usually affects. Acute Disseminated Encephalomyelitis (ADEM) is a rare condition that harms the brain and spinal cord. It causes demyelination and various neurological symptoms.
Medical Definition of Acute Disseminated Encephalomyelitis
ADEM starts with sudden inflammation in the brain and spinal cord. This leads to demyelination, damaging the protective sheath around nerve fibers. This damage hinders normal nerve signal transmission.
The medical term for ADEM highlights its difference from other demyelinating diseases like Multiple Sclerosis (MS). While both involve demyelination, ADEM is usually a monophasic disorder. It happens once, unlike MS, which has recurring episodes.
Prevalence and Demographics
ADEM is rare, with varying incidence rates in different groups. Studies show it mainly affects children and young adults. Some studies also find a slight male bias.
The exact number of ADEM cases is hard to track because of its rarity and the difficulty in diagnosing it. Yet, it often happens after viral infections or vaccinations. This hints at an autoimmune cause.
Understanding ADEM’s medical definition and who it affects helps doctors diagnose and treat it. This can lead to better outcomes for those with the condition.
The History and Discovery of ADEM
The history of ADEM is a journey through decades, filled with discoveries and growth. It shows how medical science has advanced and the hurdles researchers and doctors have faced.
Early Observations and Research
The first ADEM cases were seen in the late 19th and early 20th centuries. Doctors noticed a rare condition after infections or shots. Initial observations were key in spotting the condition, but understanding it was hard.
Research at the start aimed to tell ADEM apart from other diseases like MS. They looked at symptoms, tissue changes, and what might cause ADEM.
Evolution of Understanding ADEM
Our grasp of ADEM has grown a lot over time. New imaging tools, like MRI, help doctors diagnose and understand ADEM better. Studies have also shown how ADEM is linked to the body’s immune system.
It’s now easier to tell ADEM apart from other diseases, but some cases are tricky to diagnose. Below is a table of important moments in ADEM research.
| Year | Milestone | Description |
|---|---|---|
| 1890s | Initial Reports | First cases of ADEM reported in medical literature, associated with post-infectious and post-vaccination neurological complications. |
| 1920s-1950s | Pathological Studies | Detailed histopathological studies helped differentiate ADEM from other neurological conditions. |
| 1980s | Advances in Neuroimaging | The advent of MRI revolutionized the diagnosis and understanding of ADEM. |
Research keeps going, helping us learn more about ADEM, its causes, and treatments. The story of ADEM shows how far medicine has come and our drive to help patients.
Pathophysiology of ADEM Disease
Acute Disseminated Encephalomyelitis (ADEM) is a condition where the central nervous system is inflamed and demyelinated. We will look into how this happens, focusing on myelin, demyelination, and inflammation.
The Role of Myelin in the Nervous System
Myelin is a fatty substance that covers and protects nerve fibers. It helps electrical impulses move quickly through the nervous system. The myelin sheath is key for the nervous system’s function, allowing neurons to communicate fast and well. In ADEM, knowing how myelin works helps us understand how the condition affects the brain.
Demyelination Process in Acute Disseminated Encephalomyelitis
In ADEM, the immune system attacks the myelin sheath, causing it to break down. This attack disrupts nerve signal transmission, leading to various neurological symptoms. The exact reasons for this attack are not known, but infections or vaccinations might start it.
Inflammatory Response Mechanisms
The inflammation in ADEM involves immune cells and the release of cytokines and chemokines. This inflammation is a major part of the disease, causing tissue damage and brain problems. Knowing how this works is important for finding treatments.
Understanding ADEM’s complex pathophysiology is key. It involves immune responses and damage to the nervous system. More research is needed to better manage and treat this condition.
Causes and Risk Factors of ADEM
It’s important to know what causes ADEM to treat it early. ADEM can start from many things, so knowing what they are helps a lot.
Viral and Bacterial Infections as Triggers
Viral and bacterial infections can start ADEM. Measles, mumps, and rubella are known to cause it. But, other viruses and bacteria can also trigger it.
Post-Vaccination ADEM
Some people get ADEM after getting vaccinated. But, the chance of getting ADEM from a vaccine is very small. Vaccines are tested a lot for safety.
Genetic and Environmental Risk Factors
Genetics and the environment might also cause ADEM. Scientists are studying how these factors work together. They’re looking for genetic signs or environmental risks to stop ADEM before it starts.
In short, ADEM comes from many things like infections, genetics, and the environment. Knowing these helps treat ADEM better.
Signs and Symptoms of ADEM Syndrome
It’s important to know the signs and symptoms of ADEM syndrome for quick diagnosis and treatment. ADEM shows many neurological and systemic signs that can change in how bad they are and how fast they get worse.
Neurological Symptoms
Neurological symptoms are key signs of ADEM syndrome. These can include:
- Altered mental status: Patients may feel confused, disoriented, and have changes in consciousness.
- Motor deficits: Weakness, paralysis, or trouble moving are common.
- Seizures: Some patients may have seizures, which can be the first sign.
- Visual disturbances: Optic neuritis, leading to vision loss or blurry vision, can happen.
Systemic Symptoms
Patients with ADEM may also have systemic symptoms. These can include:
- Fever: A high body temperature is a common symptom.
- Headache: Patients often have headaches, which can be severe.
- Fatigue: General tiredness and feeling unwell are often seen.
- Nausea and vomiting: These symptoms can happen, leading to dehydration.
Symptom Progression Timeline
The timeline for symptom progression in ADEM can vary. But usually, symptoms get worse quickly over a few days. We see that:
- Acute onset: Symptoms often start within 24-48 hours.
- Peak severity: The condition usually gets the worst within a week.
- Recovery phase: Improvement can start in a few weeks, but full recovery may take longer.
It’s key for healthcare providers to know the signs and symptoms of ADEM syndrome and how they progress. This helps them make quick diagnoses and start the right treatment.
Diagnosing Acute Disseminated Encephalomyelitis
To diagnose ADEM, doctors use a mix of clinical checks, imaging tests, and cerebrospinal fluid analysis. This detailed method is key to correctly identifying ADEM and telling it apart from other diseases.
Clinical Evaluation and Patient History
The first step is a detailed clinical check and looking at the patient’s history. We examine the patient’s symptoms, past health, and any recent infections or shots. This helps us spot possible causes and understand how the disease started and grew.
During the clinical check, we do a neurological exam. This checks the patient’s brain function, motor skills, and senses. We look for signs of brain damage, like weakness, numbness, or trouble with balance and coordination.
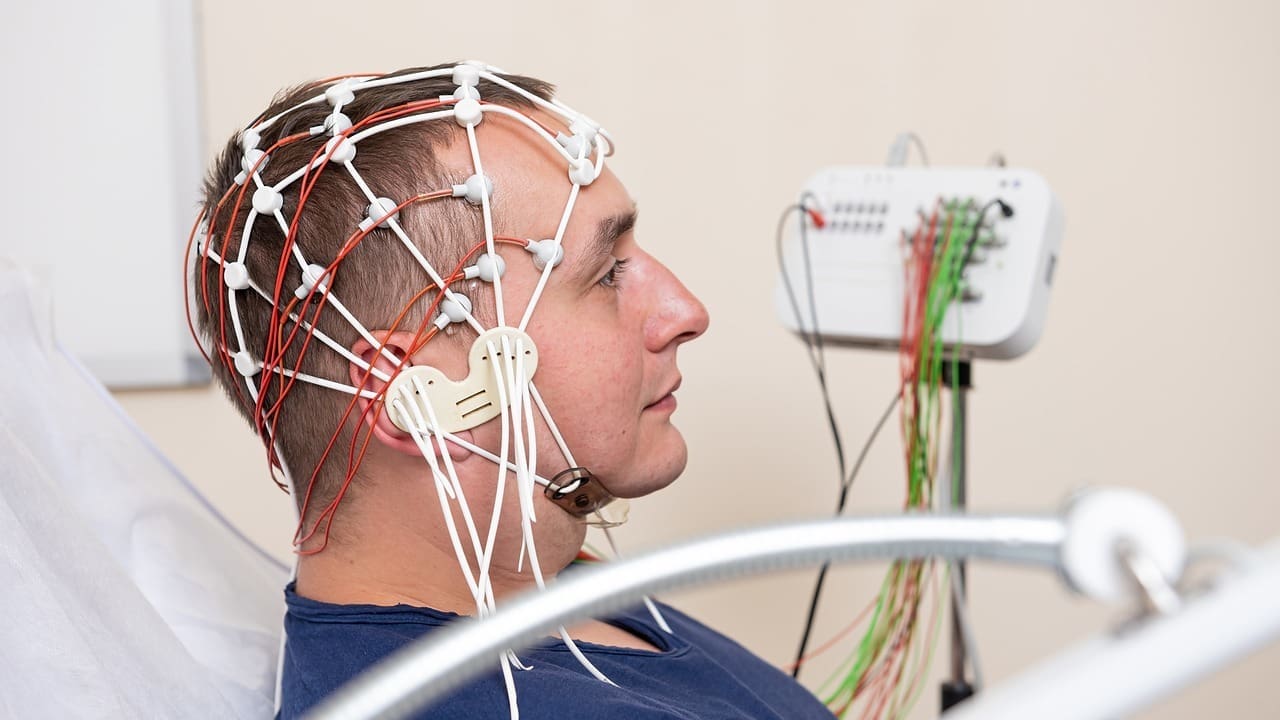
Neuroimaging: MRI and CT Scans
Neuroimaging is vital for diagnosing ADEM. MRI is the top choice because it’s great at finding brain and spinal cord lesions. It shows the white matter lesions typical of ADEM.
CT scans are sometimes used, mainly in urgent cases. But they’re not as good as MRI at spotting demyelinating lesions. We might use CT scans to check for other issues like bleeding or tumors.
Laboratory Tests and Cerebrospinal Fluid Analysis
Lab tests, including cerebrospinal fluid (CSF) analysis, are key for diagnosing ADEM. CSF analysis looks for signs of inflammation, infection, or other issues. In ADEM, the CSF might show high protein levels and lymphocytic pleocytosis, showing inflammation.
Other lab tests help rule out other conditions, like infections or autoimmune diseases. We might do blood tests to check for inflammation or immune system activity.
| Diagnostic Tool | Purpose | Key Findings in ADEM |
|---|---|---|
| Clinical Evaluation | Assess neurological symptoms and history | Neurological deficits, recent infections or vaccinations |
| MRI | Detect lesions in the brain and spinal cord | White matter lesions characteristic of ADEM |
| CSF Analysis | Examine cerebrospinal fluid for inflammation | Elevated protein, lymphocytic pleocytosis |
By using these different methods, we can accurately diagnose ADEM. This ensures patients get the right treatment and care.
ADEM Treatment Approaches
Healthcare providers use different methods to treat ADEM. They aim to manage symptoms and help patients recover. The treatment choice depends on the condition’s severity and the patient’s health.
Corticosteroids as First-Line Treatment
Corticosteroids are often the first treatment for ADEM. These drugs are strong anti-inflammatory agents. They help reduce swelling in the brain and spinal cord.
We give high-dose corticosteroids, like methylprednisolone, through an IV for a few days. This method is effective in managing ADEM symptoms and aiding recovery.
Benefits of Corticosteroids: They reduce inflammation, ease symptoms, and can be used in high doses for severe cases.
Alternative Treatments: IVIG and Plasma Exchange
For those who don’t respond to corticosteroids or have severe ADEM, other treatments are considered. Intravenous Immunoglobulin (IVIG) and plasma exchange are options. IVIG gives antibodies to help control the immune system. Plasma exchange removes harmful antibodies from the blood.
- IVIG is used to modulate the immune response and reduce inflammation.
- Plasma exchange is employed to remove pathogenic antibodies from the circulation.
Supportive Care and Symptom Management
Supportive care is key in managing ADEM symptoms and aiding recovery. This includes physical, occupational, and speech therapy, as needed. We also offer emotional support and counseling to patients and their families.
Supportive care is tailored to each patient’s needs, ensuring complete management of ADEM.
ADEM vs. Multiple Sclerosis: Key Differences
It’s important to know the difference between ADEM and multiple sclerosis for the right diagnosis and treatment. Both affect the central nervous system but show different symptoms and progress differently.
Clinical Presentation Differences
ADAM often shows up as a single episode of neurological symptoms. This can include encephalopathy, seizures, and various neurological problems. On the other hand, multiple sclerosis has episodes of symptoms that come and go, without encephalopathy.
Key differences in clinical presentation:
- ADEM: Monophasic, often with encephalopathy and seizures
- Multiple Sclerosis: Relapsing-remitting, typically without encephalopathy
Encephalopathy is a big difference between ADEM and multiple sclerosis. ADEM is more likely to have this symptom.
Disease Course and Prognosis Comparison
ADAM and multiple sclerosis have different courses and outcomes. ADEM is usually a one-time illness, with most people getting better in weeks to months. Multiple sclerosis, on the other hand, is a long-term condition with ups and downs, and its future is harder to predict.
| Disease Characteristic | ADEM | Multiple Sclerosis |
|---|---|---|
| Disease Course | Monophasic | Relapsing-remitting or progressive |
| Prognosis | Generally good, with full recovery in most cases | Variable, with possible long-term disability |
While ADEM usually has a good outcome, multiple sclerosis can lead to serious disability for some.
Diagnostic Differentiation
To tell ADEM and multiple sclerosis apart, doctors look at symptoms, brain scans, and lab tests. MRI scans are key, showing big, widespread brain lesions in ADEM and smaller, scattered lesions in multiple sclerosis.
Diagnostic criteria:
- ADEM: Large, diffuse lesions on MRI; presence of encephalopathy
- Multiple Sclerosis: Multiple, smaller lesions on MRI; dissemination in time and space
Getting the right diagnosis means looking at these criteria, symptoms, and how the disease progresses.
Complications and Long-term Effects of ADEM Medical Condition
After ADEM, many people face long-term effects and complications. These need careful management. It’s important to understand these impacts to help patients after diagnosis.
Potential Neurological Sequelae
People with ADEM might have lasting neurological problems. These can include persistent motor deficits like weakness or paralysis. They might also have sensory disturbances like numbness or tingling.
The severity and how long these problems last can vary. Some might also get seizures or epilepsy later. This can depend on how severe their ADEM was and the treatment they got.
Cognitive and Behavioral Impacts
ADEM can also affect thinking and behavior. Some might have cognitive difficulties like memory or attention problems. These can make daily life harder.
Behavioral changes are common too. Some might show mood swings, irritability, or depression. The emotional toll of ADEM is significant, and support is key for recovery.
Studies on ADEM patients have shown the importance of ongoing care. Knowing the possible long-term effects helps healthcare teams support patients better.
Prognosis and Recovery from Acute Demyelinating Encephalomyelitis
Recovering from ADEM is a journey that depends on many things. These include how bad the first episode was, how well treatment works, and the patient’s health. Knowing about the prognosis and recovery time helps patients and their families plan and make choices about care.
Typical Recovery Timeline
The time it takes for ADEM patients to get better varies a lot. Usually, people start to feel better a few weeks after starting treatment. Some may take months to fully recover. Most patients see big improvements in the first six months.
Key milestones in the recovery timeline include:
- Initial improvement: 2-4 weeks after starting treatment
- Significant recovery: 3-6 months
- Continued improvement: up to 1-2 years in some cases
Factors Affecting Prognosis
Many things can change how well someone with ADEM will do. These include how bad the first attack was, any other health problems, and how fast treatment started. Starting treatment with corticosteroids early can really help.
| Factor | Impact on Prognosis |
|---|---|
| Severity of initial attack | More severe attacks may have a slower or less complete recovery |
| Underlying health conditions | Presence of other health issues can complicate recovery |
| Timeliness of treatment | Early treatment initiation is associated with better outcomes |
Rehabilitation Strategies
Rehabilitation is key for ADEM patients to get better. A good rehab plan might include physical, occupational, and speech therapy. Each part is customized for the person’s needs. A team approach helps tackle all aspects of recovery.
Understanding ADEM’s recovery process helps patients and their families face the challenges. While it’s a tough road, many people make great progress with the right care and support.
Current Research and Future Directions in ADEM
Research into ADEM is growing, leading to new treatments. Studies aim to understand the disease better, improve diagnosis, and find better treatments.
Emerging Treatment Approaches
New treatments for ADEM are being researched. Immunomodulatory therapies try to control the immune system’s response. Stem cell therapies might repair damaged myelin and improve function.
Clinical trials are testing targeted therapies. These aim to reduce inflammation and help myelin grow back. Early results are promising for ADEM patients.
Biomarker Development for Early Diagnosis
Finding reliable biomarkers for ADEM is key. Biomarkers help diagnose early, track disease, and guide treatment. Researchers are looking for proteins, genetic markers, and imaging signs of ADEM.
High-resolution MRI and other imaging are being studied. They might spot early brain changes in ADEM. Proteomic and genomic studies aim to find unique ADEM markers.
Biomarker progress will improve ADEM diagnosis and care. This will lead to better patient results.
Conclusion
Understanding Acute Disseminated Encephalomyelitis (ADEM) is key for doctors and patients. ADEM is a rare condition that affects the brain and can be hard to diagnose. It causes neurological symptoms that need careful attention.
We’ve looked at how ADEM’s definition, causes, symptoms, and treatment are all connected. We’ve talked about what can trigger it, like infections and vaccines. The steps to diagnose ADEM include clinical checks, brain scans, and lab tests.
Treatment options like steroids and IVIG have been discussed. Early treatment is vital. We’ve also talked about ADEM’s long-term effects and the need for ongoing care and rehabilitation. This summary shows how important it is to keep researching ADEM to help patients better.
What is Acute Disseminated Encephalomyelitis (ADEM)?
ADEM is a rare condition that quickly affects the brain and spinal cord. It’s caused by the immune system attacking the brain. This can happen after a virus, a vaccine, or other reasons.
What are the symptoms of ADEM?
Symptoms include weakness, numbness, vision issues, and seizures. Fever and headache are also common. These symptoms can start quickly, within hours or days.
How is ADEM diagnosed?
Doctors use several methods to diagnose ADEM. They look at the patient’s history and do MRI and CT scans. They also test the cerebrospinal fluid. These steps help tell ADEM apart from other conditions.
What is the treatment for ADEM?
The main treatment is corticosteroids to reduce inflammation. For severe cases, doctors might use IVIG or plasma exchange. They also help manage symptoms to aid recovery.
How does ADEM differ from Multiple Sclerosis (MS)?
Both ADEM and MS affect the brain’s covering, but they are different. ADEM usually happens once, while MS can happen many times. Knowing the difference is key to proper treatment.
What is the prognosis for ADEM patients?
Most people with ADEM get better significantly. The severity of symptoms and treatment response affect the outcome. Some may need rehabilitation to overcome lasting effects.
Can ADEM be prevented?
Preventing ADEM is hard because it can be triggered by many things. Vaccines help protect against infections, but ADEM is a rare side effect. It’s important to be aware of this risk.
What are the long-term effects of ADEM?
Some people may face lasting effects like cognitive or behavioral problems. Ongoing care and rehabilitation are needed to manage these effects.
Is there ongoing research into ADEM?
Yes, research is ongoing to find better treatments and early diagnosis methods. We aim to improve understanding and management of ADEM through research and clinical trials.
What is the role of myelin in the nervous system, and how is it affected in ADEM?
Myelin helps the nervous system work right by sending signals. In ADEM, damage to myelin disrupts these signals. This leads to the symptoms seen in ADEM.
Are there any genetic or environmental risk factors for ADEM?
The exact causes of ADEM are not known, but genetics and environment might play a part. Infections and vaccines could be factors. More research is needed to understand these risks.
References:
- https://www.brainfacts.org/diseases-and-disorders/neurological-disorders-a-z/diseases-a-to-z-from-ninds/acute-disseminated-encephalomyelitis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3152158
- https://wearesrna.org/living-with-myelitis/disease-information/acute-disseminated-encephalomyelitis/long-term-care
- https://www.nationalmssociety.org/understanding-ms/what-is-ms/related-conditions/adem











