Last Updated on November 27, 2025 by Bilal Hasdemir

Cerebral venous thrombosis (CVT) is a rare and serious condition. It happens when the veins in the brain get blocked. At Liv Hospital, we provide trusted, patient-centered care for this complex issue. We make sure you get the latest treatments.
Anticoagulation therapy is the gold-standard treatment for CVT. It works well, even when there are brain bleeds too. Our medical team will walk you through each step. We focus on giving you the best care possible.
It’s important to know about CVT and its treatment options for good care. We explain the process clearly. This way, you get support and understanding every step of the way.
Key Takeaways
- CVT is a rare condition involving blockage of cerebral sinus veins.
- Anticoagulation therapy is the primary treatment for CVT.
- Effective even in cases with concurrent venous brain bleeds.
- Liv Hospital provides patient-centered care for CVT.
- Step-by-step guide ensures clarity and support throughout treatment.
Understanding Cerebral Venous Thrombosis
Venous Thrombosis (CVT)
CVT, or Cerebral Venous Thrombosis, is a unique stroke type needing special care. It happens when a blood clot forms in the brain’s venous sinuses. This can cause serious problems if not treated quickly.
What Is CVT and How Does It Differ from Other Strokes?
CVT is different from other strokes like ischemic or hemorrhagic ones. It’s caused by a blood clot in the brain’s veins, not arteries. This makes treatment and who it affects different.
CVT often hits young adults and kids. This is important for doctors to know. It’s rare and can be tricky to spot.
Common Locations: Central Sinus and Superior Sinus Thrombosis
The central and superior sagittal sinuses are where CVT usually happens. Clots here can cause headaches, high brain pressure, and vision problems. Knowing where it happens helps doctors treat it better.
Risk Factors and Demographics
CVT has its own risk factors and who it affects. For example, thrombophilia, birth control pills, and pregnancy increase the risk. Knowing these helps doctors catch it early.
| Risk Factor | Description | Demographic Most Affected |
|---|---|---|
| Thrombophilia | A condition characterized by an increased tendency to form blood clots. | Young adults |
| Oral Contraceptive Use | The use of hormonal contraceptives can increase the risk of CVT. | Women of childbearing age |
| Pregnancy and Puerperium | The period during and after pregnancy is associated with an increased risk of CVT. | Pregnant women |
It’s a great resource for learning about CVT, its diagnosis, and treatment.
Recognizing the Symptoms of Brain Blood Clots

Knowing the signs of a brain blood clot can greatly improve treatment chances. Cerebral venous thrombosis (CVT) shows different symptoms, making it hard to diagnose.
Common Warning Signs
CVT symptoms vary from person to person. Common signs include:
- Severe headache, often described as the worst headache ever experienced
- Visual disturbances, such as blurred vision or double vision
- Seizures, which can occur in some cases
- Confusion or altered mental status
- Weakness or paralysis of the face, arm, or leg
These symptoms can take hours or days to appear and get worse without treatment. It’s key to know these signs to get medical help fast.
When to Seek Emergency Medical Care
If you or someone you know has any of these symptoms, get emergency care right away:
- Sudden severe headache
- Confusion or difficulty speaking
- Weakness or numbness in the face, arm, or leg
- Vision changes or loss of vision
- Seizures or convulsions
Quick medical check-up is vital for finding CVT and starting the right treatment.
Diagnostic Challenges
Diagnosing CVT is tough because its symptoms are not clear-cut. Doctors must be very careful, especially with people at risk for CVT.
| Symptom | Frequency |
|---|---|
| Headache | 80-90% |
| Visual disturbances | 20-40% |
| Seizures | 10-20% |
It’s important for doctors to understand these challenges to make quick and correct diagnoses.
Diagnosis Process for CVT
Diagnosing CVT needs a mix of clinical checks, advanced imaging, and lab tests. This method helps doctors accurately spot CVT and tell it apart from other issues.
Initial Assessment and Medical History
The first step is a detailed clinical check and looking at the patient’s medical history. We search for signs like headaches, seizures, and brain problems. These signs might point to CVT. Knowing the patient’s medical history helps us find out if they have any risks, like recent infections or head injuries.
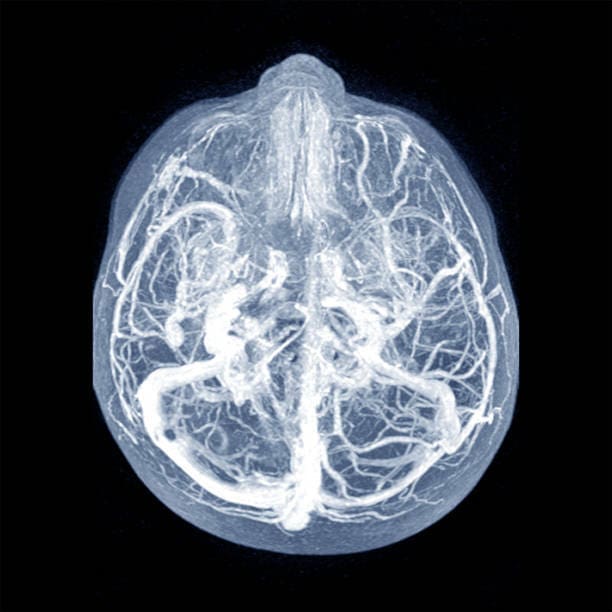
Imaging Techniques: MRI, MRV, and CT Venography
Imaging is key in finding CVT. MRI and MRV are top choices because they show the brain’s veins clearly. MRI spots clots in the brain’s veins or sinuses. MRV is great for seeing the brain’s veins. CT venography is quick and good for emergency cases, showing the brain’s veins fast.
Which imaging to use depends on the situation, what’s available, and the patient. MRI and MRV are usually better for finding CVT. But, CT venography is useful when MRI isn’t an option.
Laboratory Tests and Biomarkers
Lab tests help find conditions that might lead to CVT, like blood clotting problems or inflammation. Biomarkers like D-dimer levels can help diagnose CVT. But, D-dimer levels can be tricky to use.
Lab tests check for blood clotting issues, inflammation, and other possible causes. Together with clinical and imaging results, we can make a clear diagnosis and plan treatment.
What Is the Treatment for Blood Clot in Brain: Medical Approaches
Anticoagulation therapy is key in treating CVT, even with brain bleeds. It might seem odd to use it with bleeding, but studies show it’s safe and works well.
First-Line Treatments
The main goal is to stop the clot from getting worse and to open up the blocked veins. We start anticoagulation therapy right after we find out it’s CVT.
Anticoagulation therapy uses medicines to stop new clots and help dissolve the old ones. It’s safe for people with brain bleeds too, as research proves.
Anticoagulation Therapy Overview
For CVT, we first use low-molecular-weight heparin (LMWH) or unfractionated heparin. Then, we switch to oral meds like warfarin or DOACs. The choice depends on the patient’s health, kidney function, and other meds they take.
Managing CVT with Concurrent Venous Brain Bleeds
Dealing with CVT and brain bleeds at the same time is tricky. We stick to anticoagulation therapy but watch closely for bleeding or worsening symptoms.
| Treatment Aspect | Considerations | Clinical Approach |
|---|---|---|
| Anticoagulation Therapy | Risk of bleeding, renal function | Initiate with LMWH or unfractionated heparin |
| Monitoring | Neurological status, signs of bleeding | Regular clinical assessments and imaging |
| Long-term Management | Transition to oral anticoagulants | Warfarin or DOACs, based on patient factors |
Understanding CVT treatment helps us care for patients better. We manage the risk of clotting and bleeding to get the best results for them.
Anticoagulation Therapy: The Gold Standard
In treating CVT, anticoagulation therapy is the top choice, backed by strong evidence. It’s key in managing cerebral venous thrombosis. It stops the clot from growing and lowers the chance of more problems.
Low-Molecular-Weight Heparin (LMWH) Protocols
LMWH is often chosen for CVT treatment because it’s safe and works well. Its dose is based on the patient’s weight and given under the skin.
LMWH is easy to use and doesn’t need constant checks like some other drugs. But, the dose must be adjusted for kidney function and watch for bleeding signs.
| LMWH Protocols | Dosing | Monitoring |
|---|---|---|
| Standard Protocol | 1 mg/kg twice daily | Anti-Xa levels |
| Renal Impairment | Adjusted dose | Regular renal function tests |
Unfractionated Heparin Administration
Unfractionated heparin is also used in CVT treatment. It’s given through an IV and needs close watch on aPTT levels.
It’s good for patients with kidney problems because it doesn’t rely on kidneys for clearance. But, it needs more careful monitoring and dose changes.
Monitoring Treatment Effectiveness and Safety
Keeping an eye on treatment is key to its success and safety. Regular checks on the patient and lab tests are essential.
For LMWH, anti-Xa levels are checked. For unfractionated heparin, aPTT is monitored. These checks help adjust doses to avoid clotting and bleeding issues.
| Monitoring Parameters | LMWH | Unfractionated Heparin |
|---|---|---|
| Laboratory Test | Anti-Xa levels | aPTT |
| Frequency | Initially daily, then as needed | Every 6 hours until therapeutic, then daily |
| Target Range | 0.5-1.0 IU/mL | 1.5-2.5 times control |
Long-Term Anticoagulation Management
Managing long-term anticoagulation is key to prevent CVT from coming back. After starting with heparin, patients often need ongoing treatment. This helps lower the chance of more blood clots.
Transitioning from Heparin to Oral Anticoagulants
Switching from heparin to oral anticoagulants is a big step in managing CVT. We start oral anticoagulants while the patient is still on heparin. This ensures they stay covered with anticoagulation.
Oral anticoagulant options include warfarin and direct oral anticoagulants (DOACs). The choice depends on the patient’s health, potential drug interactions, and what they prefer.
Warfarin vs. Direct Oral Anticoagulants
The debate between warfarin and DOACs is ongoing. Warfarin has been used for years and works well. But, it needs regular INR checks and has a higher risk of bleeding.
DOACs, however, are easier to use and don’t need regular checks. Studies show they are non-inferior to warfarin in preventing blood clots. They might also have a lower risk of major bleeding.
| Anticoagulant | Monitoring Required | Bleeding Risk |
|---|---|---|
| Warfarin | Yes | Higher |
| DOACs | No | Lower |
Treatment Duration: 3-12 Month Protocols
The right length of anticoagulation therapy for CVT patients varies. Guidelines suggest treatment for 3 to 12 months. This depends on the patient’s risk factors and any underlying conditions.
We look at the risk of recurrence and bleeding to decide the treatment length. For some, longer treatment might be needed.
Surgical Interventions for Severe CVT Cases
In severe cases of Cerebral Venous Thrombosis (CVT), surgery is often needed. CVT can cause serious problems if not treated quickly and well.
Surgical intervention may be necessary when CVT leads to big brain bleeds or swelling. This can cause high pressure in the brain and even brain herniation. The choice to have surgery depends on the patient’s health, how bad their symptoms are, and the brain damage.
Indications for Surgical Treatment
Patients with severe CVT who don’t get better with medicine might need surgery. Surgery is considered when:
- There’s a big brain bleed with pressure effects
- There’s a lot of swelling in the brain causing high pressure
- There’s a risk of brain herniation
- Despite the best medicine, the patient gets worse
Studies show that decompressive craniectomy helps with severe CVT. This surgery removes part of the skull to let the brain expand and lower pressure.
Decompressive Craniectomy Procedure
Decompressive craniectomy is a surgery that helps with severe CVT. It involves:
- Removing a big part of the skull to take pressure off the brain
- Doing a duroplasty to make the dural envelope bigger
- Watching the brain pressure closely after surgery
This surgery can prevent more brain damage and improve how patients do.
Post-Surgical Care and Recovery
After decompressive craniectomy for CVT, patients need close care in a neuro-intensive care unit. This includes:
- Watching the brain pressure
- Checking how the brain is working
- Managing blood thinners
- Starting rehab to help with any brain problems
It’s key to have a team of experts working together to help these patients get better.
Endovascular Treatments for Refractory Cases
In cases where standard treatments fail, endovascular therapies can help manage CVT. For those not helped by initial treatments, these interventions offer hope.
Catheter-Directed Thrombolysis Techniques
Catheter-directed thrombolysis delivers clot-busting drugs directly to the clot. This method targets the clot more precisely than general treatments. It might lead to better results by clearing the clot more effectively.
Benefits of catheter-directed thrombolysis include:
- Lower risk of bleeding problems
- More concentrated treatment at the clot site
- Clot might dissolve faster
Mechanical Thrombectomy Procedures
Mechanical thrombectomy removes clots with special devices. It’s great for big clots or when other treatments can’t be used.
Mechanical thrombectomy techniques have evolved significantly, offering various options for clot removal:
- Aspiration thrombectomy
- Stent retriever devices
- Combined approaches using both aspiration and stent retrievers
Patient Selection and Timing of Intervention
Choosing the right patients for endovascular treatment is key. We look at how severe their symptoms are, how big the clot is, and if other treatments didn’t work.
| Patient Characteristics | Considerations for Endovascular Treatment |
|---|---|
| Severe symptoms or deteriorating condition | Early consideration for endovascular intervention |
| Extensive thrombosis | May benefit from mechanical thrombectomy |
| Failure of anticoagulation therapy | Indicates potential need for endovascular treatment |
Deciding when to do endovascular treatment depends on each patient. We consider their health and how they’ve reacted to first treatments.
By choosing the right patients and using the best endovascular methods, we can help CVT patients who didn’t get better with first treatments.
Special Considerations in CVT Treatment
Dealing with cerebral venous thrombosis (CVT) means looking at many factors. This includes pregnancy and other health issues. We know that each patient is different. So, we tailor treatment to fit each person’s needs for the best results.
Treatment Approaches for Pregnant Women
Pregnant women with CVT face a special challenge. They need to balance anticoagulation therapy with safety for both mom and baby. Anticoagulation therapy is usually recommended. It helps treat CVT without too much risk during pregnancy.
A study in the Stroke journal found that low-molecular-weight heparin (LMWH) is safe for pregnant women with CVT. It helps protect the baby while treating the mom’s condition.
| Treatment Aspect | Considerations for Pregnant Women |
|---|---|
| Anticoagulant Choice | LMWH preferred due to safety profile |
| Monitoring | Regular assessment of anti-Xa levels |
| Duration | Typically continued until delivery and postpartum |
Pediatric CVT Management
Children with CVT need a different plan. This plan considers their age, weight, and health. Pediatric CVT management often includes anticoagulation therapy. This is done with careful dosing and monitoring to avoid risks.
“The management of CVT in children should be individualized, considering the etiology, severity, and presence of risk factors for poor outcome.”
For kids, the choice of anticoagulant might change. Sometimes, unfractionated heparin or warfarin is used. Close watch is needed for bleeding or clotting signs.
Managing CVT in Patients with Underlying Conditions
Patients with other health issues, like cancer or blood disorders, need a careful approach. Comorbidities can make anticoagulation therapy tricky. It’s important to manage risks and benefits carefully.
- Assessing the underlying condition’s impact on CVT treatment
- Adjusting anticoagulation therapy according to the patient’s risk profile
- Monitoring for potential drug interactions and side effects
Understanding these special needs helps healthcare providers create better treatment plans. This improves outcomes and quality of life for CVT patients with unique needs.
Rehabilitation and Recovery Process
CVT recovery is a complex process. It needs a holistic approach, including physical therapy, cognitive rehabilitation, and supportive care. Each patient’s needs are met with a personalized plan, tackling their unique challenges.
Physical and Cognitive Rehabilitation Strategies
Physical therapy for CVT patients aims to restore motor function and improve mobility. Cognitive rehabilitation focuses on memory, attention, and executive function issues.
We use physical therapy, occupational therapy, and cognitive training to help patients regain independence. This improves their quality of life.
Lifestyle Modifications and Supportive Care
Lifestyle changes are key in recovery. Patients are encouraged to eat healthy, exercise, and manage stress well.
- Eat a diet full of fruits, vegetables, and whole grains
- Do regular physical activity, like walking or swimming
- Try stress-reducing activities, such as meditation or yoga
Preventing Recurrence and Follow-up Protocols
Preventing recurrence is vital in managing CVT. We help patients create a follow-up care plan. This includes regular check-ups and monitoring for complications.
| Follow-up Care Component | Description | Frequency |
|---|---|---|
| Clinical Evaluation | Assessment of neurological status and overall health | Every 3-6 months |
| Imaging Studies | Repeat MRI or MRV to monitor for resolution or recurrence | As needed, typically every 6-12 months |
| Anticoagulation Monitoring | Regular blood tests to adjust anticoagulant dosage | Regularly, as prescribed by the healthcare provider |
By taking a comprehensive approach to rehabilitation and recovery, CVT patients can achieve the best outcomes. This reduces the risk of recurrence.
Conclusion
Effective treatment of Cerebral Venous Thrombosis (CVT) needs a detailed and multi-faceted approach. We’ve covered the main points of CVT treatment. This includes the importance of care tailored to each patient and a team effort to better their health.
A thorough care plan is key in managing CVT. It includes anticoagulation therapy, surgery, endovascular treatments, and rehabilitation. Studies show that this team effort leads to better results for patients.
Understanding CVT’s complexities and creating a detailed treatment plan can greatly improve patient outcomes. Our discussion has shown the importance of a comprehensive CVT treatment plan. It highlights the role of anticoagulation therapy and the need for a complete care approach.
FAQ
What is cerebral venous thrombosis (CVT) and how does it differ from other types of stroke?
CVT is a rare condition where a blood clot forms in the brain’s venous sinuses. It’s different from other strokes, which usually involve blockages in arteries. CVT often affects younger people and has its own risk factors.
What are the common symptoms of CVT?
Symptoms of CVT include headache, visual disturbances, and other neurological issues. It’s important to recognize these symptoms to get medical help quickly.
How is CVT diagnosed?
Diagnosing CVT involves several steps. First, a doctor will assess you clinically. Then, imaging studies like MRI, MRV, and CT venography are used. Lab tests also confirm the presence of a blood clot in the brain’s venous sinuses.
What is the primary treatment for CVT?
The main treatment for CVT is anticoagulation therapy. This is effective even when there’s a brain bleed. Anticoagulation prevents more clots and helps dissolve existing ones.
What are the different types of anticoagulation therapy used for CVT?
For CVT, anticoagulation therapy includes low-molecular-weight heparin (LMWH) and unfractionated heparin. Then, oral anticoagulants like warfarin or direct oral anticoagulants are used. The choice depends on the patient’s needs and medical history.
How long does anticoagulation treatment last for CVT patients?
Treatment for CVT lasts from 3 to 12 months. It depends on the patient’s risk factors and any complications. Long-term management is key to prevent recurrence.
When is surgical intervention required for CVT?
Surgery, like decompressive craniectomy, might be needed for severe CVT cases. This is when there’s significant brain swelling or hemorrhage. The decision for surgery depends on the patient’s condition and medical judgment.
What are endovascular treatments for CVT?
Endovascular treatments, like catheter-directed thrombolysis and mechanical thrombectomy, are for CVT patients not responding to initial treatment. These procedures aim to dissolve or remove the blood clot directly.
How is CVT managed in special populations, such as pregnant women or children?
Managing CVT in special populations requires tailored approaches. For example, pregnant women may need adjusted anticoagulation therapy to ensure safety for both mother and fetus.
What is the role of rehabilitation in CVT recovery?
Rehabilitation is crucial for CVT recovery. It focuses on physical and cognitive rehabilitation, lifestyle changes, and supportive care. These help patients regain their abilities and prevent recurrence.
What is cerebral sinus vein thrombosis?
Cerebral sinus vein thrombosis is another term for CVT. It refers to the formation of a blood clot in the cerebral sinuses or veins.
What is central sinus thrombosis?
Central sinus thrombosis is a type of CVT affecting the central venous sinuses of the brain. It can cause various neurological symptoms and complications.
What is the difference between CVT and other types of cerebral thrombosis?
CVT is different from other cerebral thrombosis because it involves the venous system, not the arterial system. This requires different diagnostic and treatment approaches.
FAQ
What is cerebral venous thrombosis (CVT) and how does it differ from other types of stroke?
CVT is a rare condition where a blood clot forms in the brain’s venous sinuses. It’s different from other strokes, which usually involve blockages in arteries. CVT often affects younger people and has its own risk factors.
What are the common symptoms of CVT?
Symptoms of CVT include headache, visual disturbances, and other neurological issues. It’s important to recognize these symptoms to get medical help quickly.
How is CVT diagnosed?
Diagnosing CVT involves several steps. First, a doctor will assess you clinically. Then, imaging studies like MRI, MRV, and CT venography are used. Lab tests also confirm the presence of a blood clot in the brain’s venous sinuses.
What is the primary treatment for CVT?
The main treatment for CVT is anticoagulation therapy. This is effective even when there’s a brain bleed. Anticoagulation prevents more clots and helps dissolve existing ones.
What are the different types of anticoagulation therapy used for CVT?
For CVT, anticoagulation therapy includes low-molecular-weight heparin (LMWH) and unfractionated heparin. Then, oral anticoagulants like warfarin or direct oral anticoagulants are used. The choice depends on the patient’s needs and medical history.
How long does anticoagulation treatment last for CVT patients?
Treatment for CVT lasts from 3 to 12 months. It depends on the patient’s risk factors and any complications. Long-term management is key to prevent recurrence.
When is surgical intervention required for CVT?
Surgery, like decompressive craniectomy, might be needed for severe CVT cases. This is when there’s significant brain swelling or hemorrhage. The decision for surgery depends on the patient’s condition and medical judgment.
What are endovascular treatments for CVT?
Endovascular treatments, like catheter-directed thrombolysis and mechanical thrombectomy, are for CVT patients not responding to initial treatment. These procedures aim to dissolve or remove the blood clot directly.
How is CVT managed in special populations, such as pregnant women or children?
Managing CVT in special populations requires tailored approaches. For example, pregnant women may need adjusted anticoagulation therapy to ensure safety for both mother and fetus.
What is the role of rehabilitation in CVT recovery?
Rehabilitation is crucial for CVT recovery. It focuses on physical and cognitive rehabilitation, lifestyle changes, and supportive care. These help patients regain their abilities and prevent recurrence.
What is cerebral sinus vein thrombosis?
Cerebral sinus vein thrombosis is another term for CVT. It refers to the formation of a blood clot in the cerebral sinuses or veins.
What is central sinus thrombosis?
Central sinus thrombosis is a type of CVT affecting the central venous sinuses of the brain. It can cause various neurological symptoms and complications.
What is the difference between CVT and other types of cerebral thrombosis?
CVT is different from other cerebral thrombosis because it involves the venous system, not the arterial system. This requires different diagnostic and treatment approaches.
References
- Updated guidelines cerebral venous thrombosis. Retrieved from: https://www.jwatch.org/na57140/2024/02/26/updated-guidelines-cerebral-venous-thrombosis
- Cerebral Venous Thrombosis: Current Status and Challenges. Retrieved from: https://pmc.ncbi.nlm.nih.gov/articles/PMC12417975/





