At Liv Hospital, we focus on treating abdominal aortic aneurysms (AAA). This serious condition can be deadly if not treated quickly. Timely intervention is key to avoid serious problems and ensure a good outcome.
An abdominal aortic aneurysm is when the aorta in your belly gets bigger. It can grow without any symptoms. Knowing the causes, early signs, and risk factors is important for catching it early and treating it right. We use the latest methods and team up with experts to give our patients the best care.
We put our patients first and keep improving our treatments for triple A aneurysm treatment. Our goal is to give top-notch healthcare and full support to our patients from around the world.
Key Takeaways
- Abdominal aortic aneurysms (AAA) are a serious medical condition requiring timely intervention.
- Liv Hospital uses advanced protocols and multidisciplinary expertise to treat AAA.
- A patient-centered approach enhances the treatment and recovery process.
- Understanding the causes, symptoms, and risk factors is vital for early detection.
- Comprehensive care is provided to prevent complications and ensure successful outcomes.
Understanding Abdominal Aortic Aneurysms (AAA)

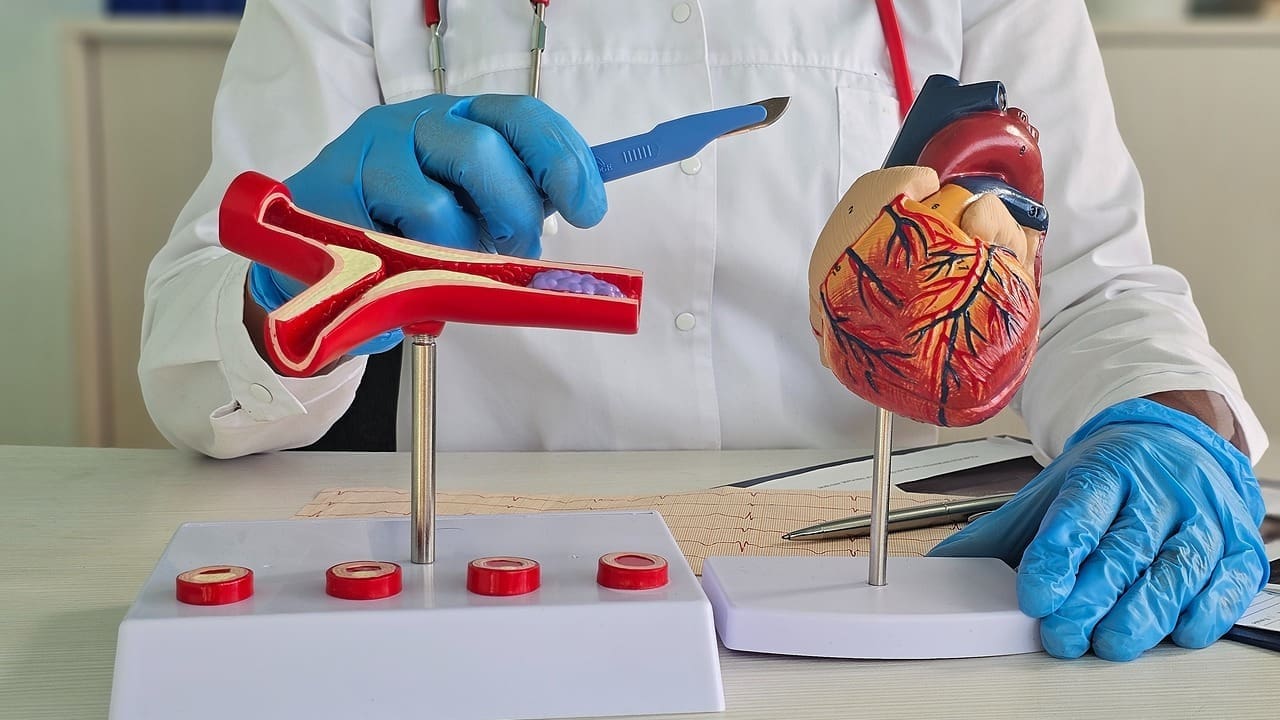
An abdominal aortic aneurysm (AAA) happens when the aorta, the main artery, weakens and bulges in the belly. This is a serious condition that needs quick medical help.
Definition and Anatomy of AAA
The aorta is the biggest blood vessel, carrying blood from the heart to the body. An AAA is when the aorta in the belly gets too big. This happens when the aortic wall gets weak, letting it bulge out under blood pressure.
The anatomy of AAA means the aortic wall gets too big. This can lead to a rupture if not treated. Knowing the anatomy is key for diagnosing and treating it right.
Causes and Risk Factors
Many things can make the aortic wall weak, leading to AAA. These include:
- Atherosclerosis, or the buildup of plaque in the arteries
- High blood pressure, which can strain the aortic wall
- Smoking, a big risk factor for vascular diseases
- Genetic factors, as people with a family history are more likely to get AAA
- Infections or inflammation that can harm the aortic wall
Knowing these causes and risk factors is key to preventing problems and managing the condition well.
| Risk Factor | Description | Impact on AAA Development |
|---|---|---|
| Atherosclerosis | Buildup of plaque in the arteries | Increases the risk of AAA by weakening the aortic wall |
| High Blood Pressure | Strains the aortic wall | Contributes to the enlargement of the aneurysm |
| Smoking | Damages the vascular system | Significantly increases the risk of developing AAA |
By knowing these risk factors, doctors can give special help to those at risk. This might stop AAA from happening or getting worse.
Diagnosis of Abdominal Aortic Aneurysms

Abdominal aortic aneurysms often don’t show symptoms, making them hard to find. Many people find out they have an AAA by chance during a scan for something else.
Symptoms and Warning Signs
Even though AAA often doesn’t show symptoms, some signs are very important. These include deep, constant pain in the belly or back, a pulsating feeling near the navel, sudden severe pain in the belly or lower back, and dizziness or fainting. These signs mean you need to see a doctor right away because they could mean a serious rupture.
Key Symptoms to Watch For:
- Deep, constant abdominal or back pain
- Pulsating sensation near the navel
- Sudden, severe pain in the abdomen or lower back
- Dizziness or fainting spells
Diagnostic Imaging Techniques
Doctors use imaging studies to find AAA. The main tools are ultrasound, CT scans, and MRI. Each has its own benefits and is chosen based on the patient’s situation.
Diagnostic Imaging Options:
| Imaging Technique | Advantages | Use Case |
|---|---|---|
| Ultrasound | Non-invasive, quick, and cost-effective | Initial screening, monitoring AAA size |
| CT Scan | High accuracy, detailed images | Preoperative planning, assessing rupture risk |
| MRI | High-resolution images without radiation | Detailed assessment, alternative to CT for some patients |
The right imaging method depends on many things. This includes the patient’s health, the aneurysm’s size and location, and the need for detailed plans before surgery. Knowing about these methods is key to treating AAA well and on time.
When Is AAA Repair Surgery Necessary?
Deciding if AAA repair surgery is needed looks at the aneurysm’s size, how fast it’s growing, and if symptoms are present. We use these details to figure out the best treatment for each patient.
Size Considerations for Intervention
The size of the abdominal aortic aneurysm (AAA) is key in deciding if surgery is needed. Small aneurysms (less than 5 cm in diameter) are often watched with tests like ultrasounds or CT scans. This is because the risk of rupture is low, and surgery’s risks might be too high.
But, for medium to large aneurysms, surgery is considered. Aneurysms 5 cm or larger are at higher risk of rupture. Prompt surgery can prevent rupture and save lives. We look at growth rate, patient health, and other factors when deciding.
Emergency vs. Elective Repair
AAA repair surgery can be planned or emergency. Planned surgery is for aneurysms at high risk of rupture. Emergency surgery is for ruptured aneurysms, which is a life-threatening situation.
Planned surgery is usually better because it allows for better preparation. Patients have lower risks of complications compared to emergency surgery.
In summary, the choice to have AAA repair surgery depends on the aneurysm’s size and the patient’s health. Understanding these factors helps patients prepare for surgery and recovery.
Types of AAA Repair Surgery Procedures
Patients with AAA face two main surgery options: open repair and endovascular aneurysm repair (EVAR). We’ll look at both to help patients understand their choices.
Open Surgical Repair Overview
Open repair means making a big cut in the belly to reach the aorta. The weak part is swapped with a man-made graft. This method has been around for a long time and works well for many.
Key aspects of open surgical repair include:
- A larger incision is made to access the aorta.
- The procedure is performed under general anesthesia.
- The recovery time can be longer compared to EVAR.
Endovascular Aneurysm Repair (EVAR) Basics
EVAR is a less invasive method. A stent graft is put in through small cuts in the groin. It’s guided to the aorta and expands to block the aneurysm.
The benefits of EVAR include:
- Smaller incisions, resulting in less tissue damage.
- Shorter recovery times compared to open repair.
- Less risk of complications in some patient groups.
Comparing Surgical Approaches
Choosing between open repair and EVAR depends on several things. These include the patient’s health, the aneurysm’s shape, and personal preferences.
| Criteria | Open Surgical Repair | EVAR |
|---|---|---|
| Incision Size | Larger | Smaller |
| Recovery Time | Longer | Shorter |
| Anesthesia | General | Local or General |
The right choice between open repair and EVAR depends on the patient. It should be decided with a healthcare provider’s advice.
The Open AAA Repair Surgery Process
The open surgical repair of abdominal aortic aneurysms (AAA) is a detailed process. It starts with preparation and ends with recovery. This traditional method is effective and requires a skilled team.
Preoperative Preparation
Before surgery, patients go through a lot of preparation. They have tests to check their health and find any risks. Cardiovascular assessment is key to see if they can handle the surgery. We also look at their medical history, medications, and allergies.
Patients are told to stop smoking and avoid certain medicines. Nutritional counseling helps them get ready for the surgery.
Surgical Technique and Graft Placement
In open AAA repair surgery, the aneurysm is removed and replaced with a synthetic graft. The surgeon makes an incision in the abdomen to reach the aorta. The aorta is clamped to stop blood flow into the aneurysm.
The aneurysm is opened, and the old aorta is replaced with a synthetic graft. This graft is made to last long and ensure blood flow. It’s securely sutured in place to prevent leaks.
Immediate Post-Operative Care
After surgery, patients are watched closely in the ICU for at least a day. Pain management is a big focus, and they get medicine for pain. We also watch for complications like bleeding or infection.
Patients usually stay in the hospital for 5 to 7 days. We help them recover and get stronger. Before they go home, they get instructions on care and follow-up appointments.
Endovascular Triple A Repair Operation (EVAR)
For many, endovascular aneurysm repair (EVAR) is a less invasive option for abdominal aortic aneurysms (AAA). It’s popular because it may lead to quicker recovery and fewer complications.
Patient Selection Criteria
Not every patient is right for EVAR. The choice to do EVAR depends on the aneurysm’s size, shape, and where it is. It also depends on the patient’s health and blood vessel structure.
Key considerations for patient selection include:
- Aneurysm morphology and its suitability for endovascular repair
- Presence of adequate sealing zones for the stent graft
- Patient’s vascular access suitability
- Overall health status and presence of comorbidities
A leading vascular surgeon says, “Choosing the right patients for EVAR is key. It’s about looking closely at the patient’s body and health.” This careful approach helps patients get the best results from EVAR.
EVAR Procedure Steps
The EVAR procedure has several important steps:
- Accessing the femoral arteries through small incisions in the groin
- Guiding a stent graft through the arteries to the aneurysm site using imaging
- Deploying the stent graft to block blood flow to the aneurysm
- Checking that the stent graft is in place and working right
Advanced imaging is key for placing the stent graft accurately. This is vital for EVAR’s success.
“Modern imaging has greatly improved EVAR outcomes.”
Advantages Over Open Surgery
EVAR has several benefits over open surgery:
- Less recovery time because of smaller cuts
- Less pain after surgery
- Shorter hospital stays
- Less chance of complications for the right patients
EVAR is appealing to many with AAA because of these benefits. But, it’s important to think about the risks and each patient’s situation.
Risks and Complications of AAA Surgical Repair
AAA repair surgery is a lifesaving procedure. But, it’s important to know the risks and complications. Both open repair and endovascular aneurysm repair (EVAR) have their own issues.
Common Complications of Open Repair
Open AAA repair is more invasive. This means it has a higher risk of complications. These can include:
- Infection: As with any surgery, there’s a risk of infection with open repair.
- Bleeding: Significant bleeding can happen during or after surgery.
- Cardiac Complications: Patients with heart problems are at higher risk of heart issues.
- Respiratory Issues: Some patients may face breathing problems after surgery.
Potential EVAR Complications
EVAR is less invasive but has its own risks. These include:
- Endoleak: A condition where blood leaks back into the aneurysm sac.
- Graft Migration: The graft can sometimes move from its original position.
- Stent Occlusion: The stent or graft can become blocked, leading to serious issues.
EVAR generally has fewer immediate complications than open repair. But, it needs careful patient selection and precise technique to reduce risks.
Long-term Surveillance Requirements
Both open repair and EVAR need long-term monitoring. For EVAR, this is key to watch for endoleaks or graft migration. Regular imaging studies, like CT scans, are recommended to check the graft’s position and function.
Long-term monitoring is vital for catching and managing complications early. This improves patient outcomes. We create a follow-up plan that fits each patient’s needs.
Recovery After AAA Repair Surgery
AAA repair surgery is just the beginning. A good recovery plan is key for healing well. We’ll guide you through the recovery process, covering important steps for a smooth recovery.
Hospital Stay Duration
The time you spend in the hospital after AAA repair surgery varies. It depends on the surgery type and your health. Patients who have open surgical repair usually stay longer than those with endovascular aneurysm repair (EVAR).
Patients are watched closely in the ICU for at least 2 days after surgery. They typically stay in the hospital for 5 to 7 days. During this time, the medical team manages pain and watches for complications.
| Type of Surgery | Average Hospital Stay | ICU Stay |
|---|---|---|
| Open Surgical Repair | 7-10 days | 2-3 days |
| Endovascular Aneurysm Repair (EVAR) | 2-5 days | 1-2 days |
Physical Limitations and Activity Guidelines
It’s important to follow a gradual recovery plan after AAA repair surgery. This helps avoid complications and ensures healing. Patients are advised to avoid heavy lifting, bending, and strenuous activities for several weeks.
Immediate Post-Surgery Period: In the first few weeks, patients should do light tasks like short walks and gentle stretching. Driving and returning to work usually happen after a doctor’s approval, often in 4-6 weeks.
- Avoid heavy lifting (>10 lbs) for 6-8 weeks
- Gradually increase walking distance and frequency
- Avoid strenuous activities, including exercise and sports, for 6-12 weeks
Follow-up Care and Monitoring
Follow-up care is vital after AAA repair surgery. Regular check-ups with your healthcare provider are important. They help monitor healing and catch any issues early.
For patients who had EVAR, regular imaging tests are needed. They check if the stent graft is working right and if there are no complications.
Stick to the follow-up schedule your healthcare team gives you. This ensures the best recovery outcome.
Conclusion
An abdominal aortic aneurysm can grow quietly. But, finding it early and getting the right care is key. We talked about why it’s important to know the causes, watch for signs, and get screened on time to avoid serious problems.
As we wrap up our talk on AAA repair surgery, it’s clear how critical early action is. We’ve seen how doctors and the healthcare system play a big role in helping AAA patients. They work hard to get the best results for everyone.
In the end, knowing the risks and acting early can greatly help patients. By giving top-notch healthcare and full support, we can really change lives. This is true for international patients looking for advanced medical care.
What is AAA repair surgery?
AAA repair surgery fixes a bulge in the aorta, the main blood vessel. It runs from the heart through the abdomen. This surgery stops the bulge from bursting, which could be deadly.
What are the risks of not treating an abdominal aortic aneurysm?
Not treating an aneurysm can lead to a rupture. This causes severe bleeding, shock, and can be fatal. We advise regular checks and surgery for large or growing aneurysms.
How is AAA diagnosed?
We use ultrasound, CT scans, and MRI to find AAA. These tests show the size and location of the bulge. This helps us decide the best treatment.
What are the symptoms of AAA?
AAA often doesn’t show symptoms until it bursts. But, some may feel abdominal pain, back pain, or a pulsating mass. If you notice these, see a doctor right away.
What are the types of AAA repair surgery?
We do two main types of surgery: open repair and EVAR. Open repair needs a big cut to reach the aorta. EVAR is less invasive, using a stent graft.
What is the recovery process like after AAA repair surgery?
After surgery, we watch patients closely in the hospital. They need to follow physical limits and activity guidelines. We also check up on them later to see how they’re doing.
What are the possible complications of AAA surgical repair?
AAA repair surgery can have risks like bleeding, infection, and graft failure. We do our best to avoid these and care for our patients well.
How is EVAR different from open surgical repair?
EVAR is less invasive, leading to quicker recovery, less pain, and fewer problems. We choose EVAR for certain aneurysm sizes and locations.
What is the role of long-term surveillance after AAA repair?
We keep an eye on patients after repair for graft failure or endoleak. Regular check-ups and tests help catch issues early, ensuring the best care.
Can AAA be prevented?
We can’t prevent AAA, but a healthy lifestyle can lower the risk. Eating right, exercising, and not smoking help. Regular check-ups are also important for those at risk.























