Last Updated on November 26, 2025 by Bilal Hasdemir
When a brain aneurysm threatens a patient’s life, precision and innovation are key. Today, cerebral stent surgery brings new hope. It reinforces weakened blood vessels in the brain through a minimally invasive procedure.
At Liv Hospital, we use advanced technology and put patients first. We ensure every brain aneurysm cerebral stent placement follows the latest evidence and highest ethical standards.
The global market for intracranial stents is expected to hit $500 million by 2025. This shows how important this treatment is becoming. As we look into stent aneurysm surgery, we’ll talk about its benefits and the future of this life-saving technology.
Key Takeaways
- Minimally invasive stent surgery offers new hope for treating brain aneurysms.
- Liv Hospital combines advanced technology with a patient-first approach.
- The global market for intracranial stents is projected to reach $500 million by 2025.
- Stent aneurysm surgery is becoming increasingly important in managing brain aneurysms.
- Our approach ensures the highest ethical standards in every procedure.
Brain Aneurysms and the Evolution of Treatment Approaches

Brain aneurysms are a serious health issue. Their treatment has changed a lot. Thanks to new medical tech and methods, we can now handle this condition better.
What Causes Brain Aneurysms and Who Is at Risk
Brain aneurysms happen when blood vessel walls in the brain get weak. This can be because of genes, high blood pressure, or other health issues. Knowing the risk factors helps catch and prevent them early. People with a family history, smokers, and those with certain health problems are more at risk.
Traditional Surgical Approaches vs. Minimally Invasive Techniques
Oldly, brain aneurysms were treated with open surgery. This involved clipping the aneurysm to stop it from bursting. But now, minimally invasive endovascular techniques are taking over. They are safer and let patients recover faster. These new methods include coiling and stenting, which we’ll look into more.
The Shift Toward Endovascular Treatments
The move to endovascular treatments is because they work well and have fewer side effects than old surgery. These treatments, like using stents for brain aneurysms, are now the first choice. They are less invasive and safer for patients.
As we keep improving in neurovascular medicine, treating brain aneurysms will get even better. This brings new hope to patients all over the world.
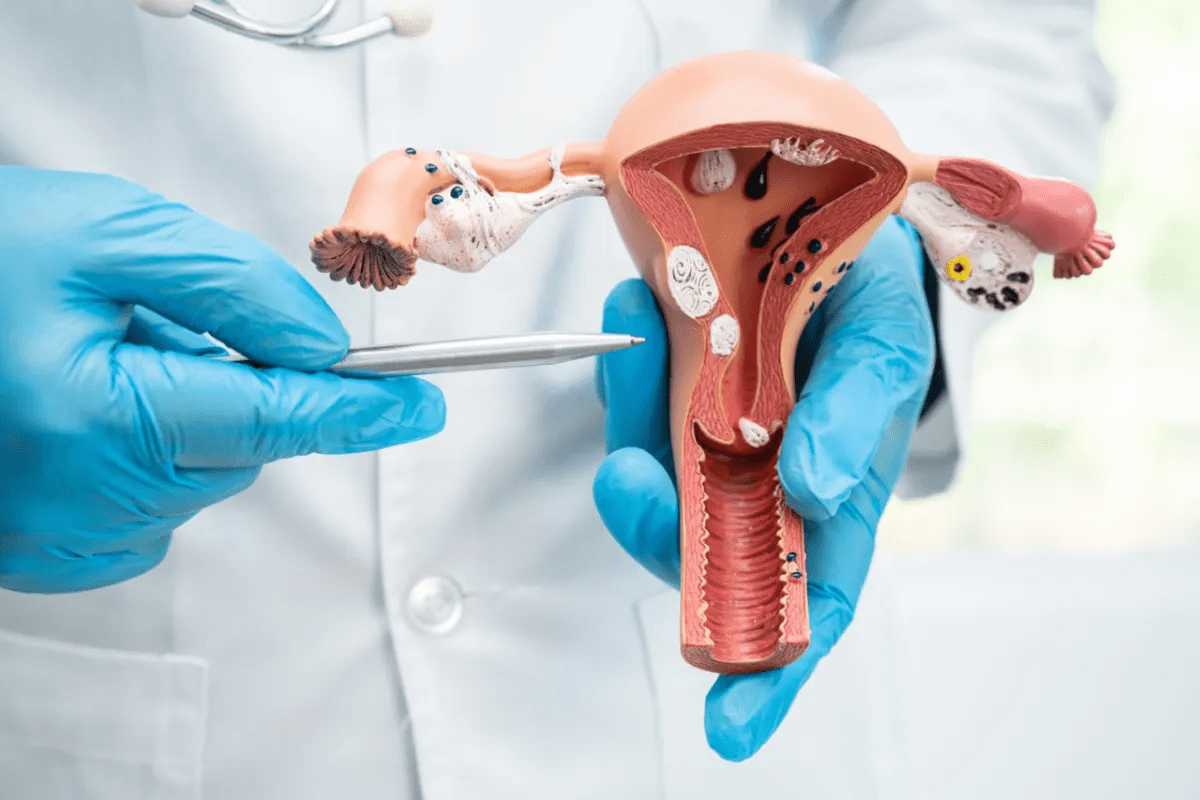
What Is a Cerebral Stent and How Does It Function
A cerebral stent is a medical device used to treat brain aneurysms. It diverts blood flow away from the aneurysm sac. This helps blood to clot inside the aneurysm, eventually closing it off.
We use cerebral stents in endovascular treatments. These treatments are minimally invasive. They guide through blood vessels to reach the brain aneurysm.
Definition and Purpose in Aneurysm Management
Cerebral stents are made for the brain’s blood vessels. Their main job is to stop aneurysm rupture by changing blood flow. This reduces pressure on the aneurysm wall, lowering rupture risk.
We often pair these stents with other treatments like coiling. This combination helps achieve the best results.
The stents are designed to be flexible and easy to navigate through the brain’s blood vessels. They are made from materials that are safe and last long.
How Stents Prevent Aneurysm Rupture
Cerebral stents prevent rupture by diverting blood flow. This reduces pressure on the aneurysm wall. It also promotes clotting inside the aneurysm.
Over time, this can lead to the aneurysm being completely closed off. This greatly reduces the risk of rupture.
| Mechanism | Effect on Aneurysm |
| Diverts blood flow away from aneurysm sac | Reduces pressure on aneurysm wall |
| Promotes clotting within aneurysm | Leads to eventual occlusion of aneurysm |
“The use of cerebral stents has revolutionized the treatment of complex aneurysms, providing a safe and effective solution for patients at risk of rupture.” Medical expert
Visual Guide: What Does a Cerebral Stent Look Like
They have a mesh-like structure. This allows blood to flow to other vessels while diverting it from the aneurysm.
Deploying a cerebral stent requires precise navigation. We use real-time imaging for this. Once in place, the stent expands to fit the vessel securely.
Key Fact #1: Types of Brain Stents and Their Applications
Brain aneurysm treatment has changed a lot with new stent technologies. We now have balloon-expandable and flow-diverting stents. These have made endovascular procedures much better.
Balloon-Expandable Stent Technology
Balloon-expandable stents are key in treating brain aneurysms. They are put on a balloon catheter and expanded in the brain vessel. Their main benefits are:
- Precise placement and deployment
- Ability to navigate through complex vascular anatomy
- Immediate expansion to support the vessel wall
This tech is great when exact stent placement is needed.
Self-Expanding Stent Innovations
Self-expanding stents are another way to treat brain aneurysms. They expand on their own after being deployed. Their advantages are:
- Flexibility and conformability to complex vessel geometries
- Reduced risk of vessel injury during deployment
- Potential for improved long-term patency rates
Flow-Diverting Stents Like the Tubridge
Flow-diverting stents are a big step forward in treating complex brain aneurysms. They redirect blood flow away from the aneurysm. This helps the aneurysm to close off. The Tubridge is a flow-diverting stent that has shown good results in studies.
The main benefits of flow-diverting stents are:
- Effective treatment of complex and large aneurysms
- Potential for reduced need for coiling procedures
- Improved outcomes in cases with challenging anatomy
Knowing about the different brain stents helps doctors choose the best treatment for each patient.
Key Fact #2: The $500 Million Brain Stent Market
The brain stent market is expected to reach $500 million by 2025. This growth comes from new technology, more brain aneurysms, and a preference for less invasive treatments.
Current Market Size and Growth Projections Through 2025
The market for cerebral aneurysm covered stents has grown over the years. We predict it will keep growing, with a 10% annual increase until 2025. This is because more doctors are using intracranial stents for tough aneurysms.
Technological Advancements Driving Adoption
New technology is key to brain stent adoption. Improvements in stent design, materials, and delivery systems have made them safer and more effective. For example, flow-diverting stents have changed how we treat complex aneurysms.
These stents direct blood flow away from the aneurysm, helping it clot and reducing rupture risk. Better imaging technologies also help diagnose and treat brain aneurysms. They allow for more precise stent placement, lowering complication risks.
Regional Differences in Cerebral Stent Utilization
Brain stent use varies by region, due to healthcare systems, trained professionals, and treatment guidelines. In the U.S. and Europe, intracranial stent use is high thanks to strong healthcare and good insurance coverage.
In contrast, Asia and Latin America are seeing more demand for brain stents. This is because of growing awareness of minimally invasive treatments and better healthcare. These regions will play a big role in the global brain stent market’s growth.
Key Fact #3: Clinical Success Rates of Intracranial Stent Procedures
Intracranial stent procedures have changed how we treat brain aneurysms. They offer high success rates. These advancements help manage complex aneurysms better.
Occlusion Rates for Complex Aneurysms (80% Success)
Research shows intracranial stenting works well for complex aneurysms, with an 80% occlusion rate. This is a big improvement over older methods. Stents help stop the aneurysm from rupturing by promoting clotting.
A study in a top medical journal found that flow-diverting stents closed aneurysms in 78% of cases after a year.
“The use of flow-diverting stents has revolutionized the treatment of complex aneurysms, providing high occlusion rates with few complications.”
Impact on Branch Vessels and Blood Flow
Stent placement affects branch vessels and blood flow. Modern stents, like the Tubridge stent, are designed to avoid blocking these vessels. This leads to better patient outcomes and fewer complications.
| Stent Type | Branch Vessel Occlusion Rate | Blood Flow Preservation |
| Tubridge Stent | 5% | 95% |
| Flow-Diverting Stent | 7% | 93% |
Complication Rates Compared to Traditional Surgery
Intracranial stent procedures have fewer complications than traditional surgery. They have lower rates of brain damage, morbidity, and mortality. This means patients recover faster.
- Reduced risk of brain damage
- Lower morbidity rates
- Shorter recovery times
In conclusion, intracranial stent procedures are a highly effective treatment for brain aneurysms. They have high success rates and fewer complications than traditional surgery. As technology improves, we can expect even better results for patients with brain aneurysms.
Key Fact #4: The Brain Stent Surgery Procedure
Learning about brain stent surgery is key for those thinking about it. This method, also known as stent placement, is a complex treatment for brain aneurysms.
Patient Preparation and Anesthesia Considerations
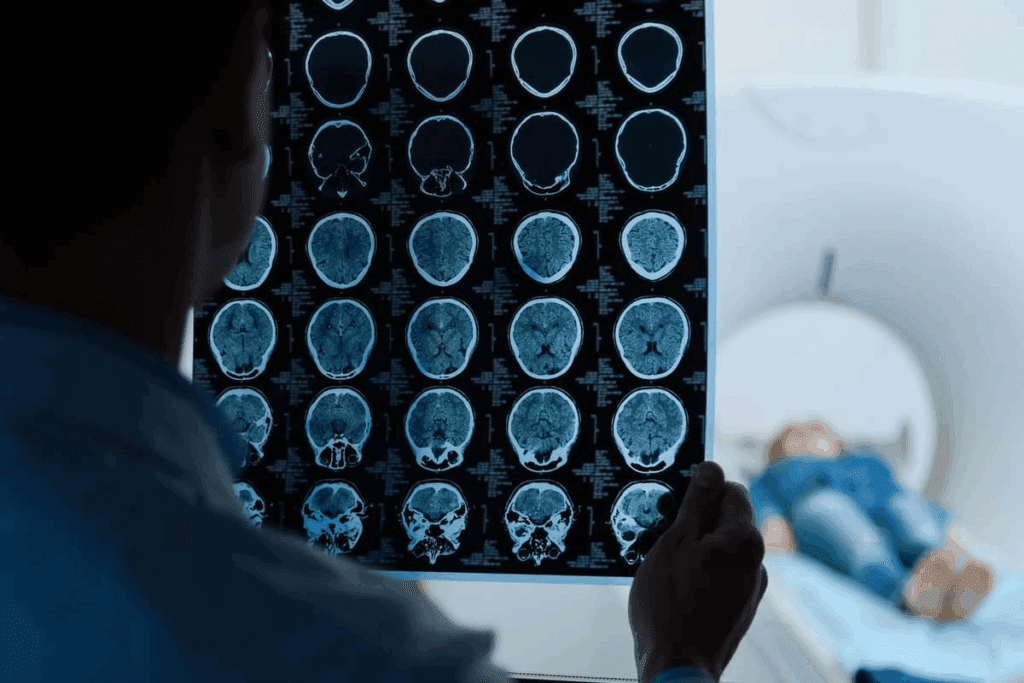
Before brain stent surgery, patients get ready in many ways. They have a full medical check-up, imaging tests like angiography, and talk about the surgery’s risks and benefits. They also need general anesthesia to stay comfortable and calm during the surgery.
- Pre-procedure imaging tests to assess the aneurysm’s size and location
- Discussion of medical history and current medications
- Administration of general anesthesia
Step-by-Step Procedure Walkthrough
The brain stent operation has several important steps:
- A small incision is made in the groin to access the femoral artery.
- A catheter is guided through the artery to the brain, using real-time imaging.
- The stent is deployed across the aneurysm neck to prevent blood flow into the aneurysm.
- The catheter is removed, and the incision is closed.
Post-Procedure Recovery Timeline
After the stent in brain procedure, patients are watched closely in a recovery unit. The recovery time can differ, but most stay for a few hours to overnight. Some might feel sore or bruised at the catheter site, which usually goes away in a few days.
Key aspects of post-procedure recovery include:
- Monitoring for possible complications
- Managing any discomfort after the procedure
- Follow-up imaging to check the stent and aneurysm
By knowing about the brain stent surgery process, patients can better get ready for treatment and what to expect during recovery.
Key Fact #5: Combining Stenting with Coiling for Enhanced Outcomes
Stenting with coiling is a top choice for treating some brain aneurysms. This method, called stent-assisted coiling, boosts results by adding support to the aneurysm wall. It also helps in closing the aneurysm completely.
The Stent-Assisted Coiling Technique Explained
Stent-assisted coiling starts with placing a stent across the aneurysm’s neck. Then, coils are put into the aneurysm sac through the stent’s mesh. This method makes coil packing more stable and lowers the chance of coils getting into the main blood vessel.
The stent acts as a support, keeping the coils in place. This improves the treatment’s stability. By using both stenting and coiling, doctors can get better closure rates and lower the chance of the aneurysm coming back.
Ideal Aneurysm Characteristics for Combined Approach
Not every aneurysm is right for stent-assisted coiling. The best candidates usually have wide necks or complex shapes. Aneurysms at high risk of bursting or those that have come back after treatment also benefit from this method.
- Aneurysms with wide necks (>4 mm)
- Complex or irregular aneurysm morphology
- Aneurysms with a high risk of rupture
- Recurrent aneurysms after previous coiling
Comparative Outcomes with Single-Modality Treatments
Research shows stent-assisted coiling works better for complex or wide-necked aneurysms. It leads to higher closure rates and fewer comebacks than coiling alone. Though it might have a bit higher risk of problems, the benefits usually outweigh the risks.
In summary, combining stenting with coiling is a key treatment for some brain aneurysms. Knowing its advantages and limits helps doctors make the best choices for their patients.
Key Fact #6: Patient Selection and Risk Assessment for Brain Aneurysm Stenting
Choosing the right patients for brain aneurysm stenting is key. It’s important to carefully check each candidate. This helps reduce risks and improve results.
Ideal Candidates for Cerebral Stent Procedures
Looking for the best candidates for cerebral stent procedures is a detailed process. We consider the patient’s health, the aneurysm’s size and location, and their medical history. Patients with complex or wide-necked aneurysms are often good for stenting. We also look at those who have tried other treatments without success.
Aneurysm Size and Location Considerations
The size and location of the aneurysm are very important. Aneurysms in certain spots, like the basilar artery or posterior communicating artery, are harder to treat. We look at the aneurysm’s shape and size to choose the best treatment.
Contraindications and High-Risk Scenarios
While stenting can help many, some shouldn’t try it. This includes those with severe vascular tortuosity or calcification, bleeding disorders, or serious health issues. We check each patient’s risk to find the safest treatment.
By carefully looking at these factors, we can make sure cerebral stenting works best for brain aneurysm treatment. This helps improve patient results.
Conclusion: The Future of Brain Aneurysm Stent Technology
The way we treat brain aneurysms has changed a lot thanks to new stent technology. Stents are now a key part of endovascular treatments. They offer a less invasive option compared to old surgical methods.
There are different stents for various aneurysms, like balloon-expandable and self-expanding ones. The market for these stents is expanding. This is because of new technologies and more doctors using them.
Studies show that stent treatments are working well. They have high success rates for complex aneurysms. They also have fewer complications than traditional surgery.
The future of brain aneurysm stents looks bright. We’ll see better stent designs and materials soon. This will lead to even better results for patients.
Stent-assisted coiling and other treatments will also improve care. Intracranial stents will keep being a key part of treating aneurysms. They will offer safe and effective options for patients everywhere.
FAQ
What is a cerebral stent?
A cerebral stent is a small, mesh-like device. It’s used to treat brain aneurysms. It prevents blood flow into the aneurysm, reducing the risk of rupture.
How does a cerebral stent prevent aneurysm rupture?
A cerebral stent is placed across the aneurysm’s neck. It changes blood flow patterns. This reduces pressure on the aneurysm wall and promotes clotting inside.
What does a cerebral stent look like?
A cerebral stent is a tiny, tubular structure. It’s made of metal mesh. It’s designed to be flexible and fit the blood vessel’s shape.
What are the different types of brain stents available?
There are several types. These include balloon-expandable stents, self-expanding stents, and flow-diverting stents. Each has unique characteristics and uses.
How is brain stent surgery performed?
Brain stent surgery is done through a minimally invasive procedure. A catheter is guided through the blood vessels. The stent is deployed to treat the aneurysm.
What is stent-assisted coiling?
Stent-assisted coiling combines a cerebral stent with coiling. It treats complex aneurysms more effectively. Tiny coils are used to fill the aneurysm.
Who are ideal candidates for cerebral stent procedures?
Ideal candidates have complex or wide-necked aneurysms. They are difficult to treat with coiling alone. Candidates are assessed based on aneurysm size, location, and health.
What are the risks associated with brain stent surgery?
Risks include stroke, stent thrombosis, and aneurysm rupture. These are rare with modern technology and techniques.
How successful are intracranial stent procedures?
Intracranial stent procedures have high success rates. Complex aneurysm occlusion rates are around 80%. Success can vary based on individual factors.
What is the recovery process like after brain stent surgery?
Recovery involves a short hospital stay for monitoring. It includes rest and follow-up appointments. These ensure the stent works correctly and the aneurysm is resolving.
References
- Alkhalili, K., et al. (2018). The effect of stents in cerebral aneurysms: A Review. Translational Neuroscience, 9(1), 1-10. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5898080/