Last Updated on November 20, 2025 by Ugurkan Demir
Sickle cell anemia is a genetic disorder that affects how red blood cells How Does the Skeleton Produce Blood Cells? Understanding Blood Cell Formation in Bone Marrowcarry oxygen. It is sickle cell autosomal recessive, caused by a specific mutation in the HBB gene. This gene tells our bodies how to make a part of hemoglobin.
We will look into how this genetic defect causes abnormal hemoglobin S. This leads to red blood cells becoming misshapen.
Medical research shows that sickle cell anemia is inherited in an autosomal recessive pattern. This means a person needs two copies of the mutated gene to have the disorder. Knowing this is key for diagnosing and managing the disease.
Key Takeaways
- Sickle cell anemia is caused by a mutation in the HBB gene.
- The condition is inherited in an autosomal recessive pattern.
- Understanding the genetic basis is key for diagnosis and management.
- The mutation leads to the production of abnormal hemoglobin S.
- Sickle cell anemia results in the sickling of red blood cells.
The Nature and Global Impact of Sickle Cell Anemia

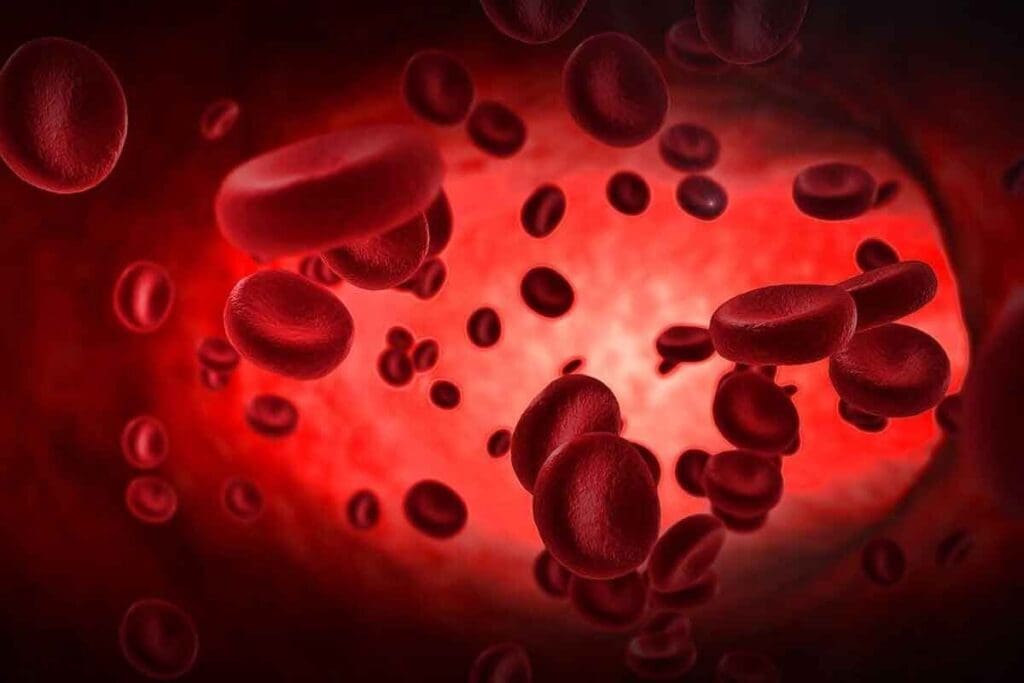
To understand sickle cell anemia, we need to look at its definition, key features, and how common it is worldwide. It’s a genetic disorder that affects how red blood cells carry oxygen. This is because of a problem with hemoglobin, a protein in these cells.
Definition and Characteristic Features
Sickle cell anemia happens when there’s abnormal hemoglobin S. This is due to a gene mutation on chromosome 11. This mutation changes how hemoglobin is made, leading to sickle-shaped red blood cells.
The disease causes pain, anemia, and other issues. These sickle-shaped cells can block blood flow in small vessels. This can lead to many health problems.
Worldwide Prevalence and Distribution Patterns
Sickle cell disease happens when someone gets two bad copies of the β-globin gene, one from each parent. It affects millions worldwide, mostly in places where malaria was common, like sub-Saharan Africa and parts of India.
In these areas, the sickle cell trait is more common. It helps protect against malaria. We’ll look at where sickle cell anemia is most common and its impact.
Knowing how sickle cell anemia spreads and its key features helps us see why we need good healthcare for it.
Hemoglobin Structure and Function in Normal Red Blood Cells

In normal red blood cells, hemoglobin works well to carry oxygen. It’s a protein in red blood cells that moves oxygen from the lungs to the body’s tissues.
The Role of Hemoglobin in Oxygen Transport
Hemoglobin is key to carrying oxygen. Humans usually have hemoglobin A, made of two alpha and two beta chains. This setup lets hemoglobin grab oxygen in the lungs and let it go in the tissues. The beta-globin chains are very important because they help cause sickle cell anemia.
Normal Beta-Globin Chain Production
Producing normal beta-globin chains is vital for hemoglobin to work right. The beta-globin chains come from the HBB gene on chromosome 11. In healthy people, the HBB gene makes a beta-globin protein that pairs with alpha-globin chains to form hemoglobin A.
| Component | Function |
| Alpha-globin chains | Part of the hemoglobin structure |
| Beta-globin chains | Crucial for oxygen binding and release |
| Hemoglobin A | Normal adult hemoglobin |
People with one mutated gene and one normal gene are carriers (sickle cell trait). They usually don’t show symptoms because the normal gene makes enough functional hemoglobin to prevent the disease.
Is Sickle Cell Anemia Autosomal Recessive? Understanding the Inheritance Pattern
Sickle cell anemia is caused by a mutation in a gene on an autosome. This is known as an autosomal recessive inheritance pattern. For someone to have the disease, they need to get two copies of the mutated gene, one from each parent.
Principles of Autosomal Recessive Inheritance
Autosomal recessive inheritance means a person needs two copies of the mutated gene to show the disease. Those with one normal and one mutated gene are carriers. They don’t show the disease, but can pass the mutated gene to their kids.
Let’s look at the chances in autosomal recessive inheritance with a simple example:
| Parent 1 / Parent 2 | Normal Gene | Mutated Gene |
| Normal Gene | Normal | Carrier |
| Mutated Gene | Carrier | Affected |
This table shows the possible genotypes of kids when both parents are carriers. There’s a 25% chance a child will be affected, a 50% chance they’ll be a carrier, and a 25% chance they won’t be affected or a carrier.
Genetic Transmission of Sickle Cell Anemia
The genetic transmission of sickle cell anemia follows the autosomal recessive pattern. If both parents are carriers, there’s a high risk their kids could be affected. Genetic counseling is key for families with sickle cell anemia history to understand their risks.
“Sickle cell disease is a significant public health problem in many parts of the world, and understanding its genetic basis is critical for effective management and treatment strategies.”
The inheritance pattern of sickle cell anemia is complex. It involves understanding the chances of genetic transmission. By understanding these principles, families can better manage the risks of this condition.
The HBB Gene Mutation on Chromosome 11
Sickle cell anemia comes from a mutation in the HBB gene on chromosome 11. This gene is key for making the beta-globin subunit of hemoglobin. Hemoglobin is a vital part of red blood cells.
Location and Normal Function of the HBB Gene
The HBB gene is found on the short arm of chromosome 11 (11p15.4). It tells our bodies how to make the beta-globin subunit of hemoglobin. Hemoglobin is made of two alpha-globin chains and two beta-globin chains.
The beta-globin chains help hemoglobin work right. It carries oxygen from the lungs to our body’s tissues.
The Specific Point Mutation in Sickle Cell Anemia
Sickle cell anemia is caused by a point mutation in the HBB gene. This mutation changes glutamic acid to valine at the sixth position of the beta-globin chain. It happens because of a single nucleotide change (GAG to GTG).
This change makes hemoglobin S (HbS), an abnormal form of hemoglobin. Hemoglobin S causes red blood cells to sickle under low oxygen. This sickling leads to pain, infections, and other problems.
Molecular Mechanism: From Gene Mutation to Abnormal Protein
The cause of sickle cell anemia is a gene mutation. This mutation changes the structure of hemoglobin, making it abnormal. The mutation affects the beta-globin subunit of hemoglobin.
We will look at how the HBB gene mutation leads to HbS production. This causes red blood cells to become sickle-shaped.
Single Nucleotide Substitution (GAG to GTG)
The genetic defect behind sickle cell anemia is a single nucleotide substitution in the HBB gene. The codon GAG changes to GTG due to a point mutation.
This change happens at the DNA level. It is then transcribed into mRNA. This leads to an incorrect amino acid being added during protein synthesis.
Amino Acid Change: Glutamic Acid to Valine at Position 6
The single nucleotide substitution changes glutamic acid to valine at the sixth position of the beta-globin chain.
This change is key. It changes hemoglobin’s properties, making it more likely to polymerize under low oxygen conditions.
Structural Consequences on the Beta-Globin Chain
The substitution of glutamic acid with valine at position 6 has big structural consequences for the beta-globin chain.
The altered beta-globin chains form long fibers under low oxygen. This distorts red blood cells into a sickle shape.
| Mutation Type | Amino Acid Change | Structural Consequence |
| Single Nucleotide Substitution | Glutamic Acid to Valine at Position 6 | Polymerization of Hemoglobin S, Sickling of Red Blood Cells |
Hemoglobin S: The Abnormal Protein in Sickle Cell Anemia
Hemoglobin S is the abnormal protein found in sickle cell anemia. It has unique properties that set it apart from normal hemoglobin A. We will look into how these properties cause red blood cells to sickle.
Biochemical Properties of Hemoglobin S
Hemoglobin S comes from a mutation in the HBB gene. This mutation changes glutamic acid to valine at position 6 of the beta-globin chain. This single change makes Hemoglobin S more likely to polymerize when oxygen levels are low.
The polymerization of Hemoglobin S is key to sickle cell anemia’s effects. When it polymerizes, it forms long, stiff fibers inside red blood cells. This makes the cells take on a sickle shape, which harms their flexibility and structure.
Polymerization of Hemoglobin S Under Low Oxygen Conditions
When oxygen levels are low, Hemoglobin S turns into long strands inside red blood cells. This causes the cells to sickle. This process can damage the red blood cell membrane over time, leading to hemolysis and vaso-occlusive crises.
The polymerization of Hemoglobin S is influenced by several factors. These include the amount of Hemoglobin S, the presence of other hemoglobins, and oxygen levels. Understanding these factors is key to finding treatments that prevent or reduce sickling.
By studying Hemoglobin S’s biochemical properties and how it behaves under different conditions, we can learn more about sickle cell anemia. This knowledge is vital for creating effective treatments to lessen the disease’s impact.
Pathophysiology: From Genetic Defect to Clinical Manifestations
Sickle cell anemia’s pathophysiology is complex. It starts with a genetic mutation and ends with clinical symptoms. We’ll see how the genetic defect changes red blood cells and causes health problems.
The Sickling Process and Red Blood Cell Deformation
The sickling process is key in sickle cell anemia. Red blood cells with hemoglobin S change shape when oxygen levels are low. They become sickle-shaped due to hemoglobin S polymerization.
This change makes red blood cells rigid and less flexible. They are damaged more easily, leading to anemia. Their shape also makes it hard for them to move through small blood vessels, causing vascular problems.
Vascular Occlusion and Tissue Damage Mechanisms
Vascular occlusion is a big problem in sickle cell anemia. Sickled red blood cells block small blood vessels, stopping blood flow. This causes tissue damage and pain.
Not just the blockage is a problem. Inflammation and damage to the blood vessel walls also play a role. These factors make sickle cell anemia a complex disease with many symptoms.
Triggers That Exacerbate Sickling Events
Some things can make sickling events worse. Low oxygen, dehydration, infections, and extreme temperatures are examples. Knowing these triggers is key to managing the disease.
By avoiding these triggers, people with sickle cell anemia can have fewer and less severe sickling events. This improves their life quality. We stress the need for good care and education for those with this disease.
Sickle Cell Trait: The Heterozygous State
Carrying the sickle cell trait means having one mutated HBB gene and one normal gene. This leads to making both hemoglobin A and hemoglobin S. It’s called being heterozygous for the sickle cell gene. We’ll look at the genetic profile, health effects, and how it protects against malaria.
Genetic Profile and Hemoglobin Composition in Carriers
People with sickle cell trait have a special genetic makeup. They have one normal HBB gene and one mutated one. This makes them produce both normal and sickle hemoglobin.
This mix of hemoglobins affects their health and how they feel.
Health Implications and Rare Complications
Mostly, carriers of sickle cell trait don’t show symptoms or have mild ones. But, extreme situations like flying at high altitudes or intense workouts can cause problems. They might rarely get hematuria or splenic infarction in extreme cases, as studies show.
It’s important for carriers to know about these risks. But, severe sickling crises are not common.
Malaria Resistance in Sickle Cell Trait Carriers
Carrying the sickle cell trait helps fight off malaria, mainly the severe kind by Plasmodium falciparum. The sickle hemoglobin makes it hard for the parasite to grow. So, carriers are more likely to survive in areas where malaria is common.
The trait gives a survival edge against malaria, which is why it’s more common in malaria areas, showing how genetics and environment interact.
Genetic Testing, Diagnosis, and Family Planning
Genetic testing has greatly improved how we diagnose and manage sickle cell anemia. It’s key for diagnosing the disease and planning families. We’ll look at the different ways to test for sickle cell anemia, including prenatal and newborn screenings.
Prenatal and Newborn Screening Methods
Prenatal testing checks the fetus for sickle cell mutations, usually through amniocentesis or CVS. Newborn screening tests babies soon after birth with a blood sample from a heel prick.
Early diagnosis helps prevent complications and educates families about the condition. Below is a table that outlines the main features of prenatal and newborn screening.
| Screening Method | Timing | Sample Type | Key Benefits |
| Prenatal Screening | 16-20 weeks gestation | Amniotic fluid or chorionic villus | Early diagnosis, family planning |
| Newborn Screening | Shortly after birth | Blood from heel prick | Early intervention, parental education |
Genetic Counseling for Affected Families
Genetic counseling is vital for families with sickle cell anemia history. Counselors explain the disease’s inheritance, transmission risks, and carrier implications.
For families with sickle cell anemia history, counseling helps understand risks. It aids in making reproductive choices. Healthcare teams, including geneticists and counselors, provide this guidance.
Emerging Technologies in Sickle Cell Mutation Detection
New technologies like next-generation sequencing (NGS) and non-invasive prenatal testing (NIPT) are changing sickle cell anemia detection. NGS quickly and affordably analyzes genes, including the HBB gene.
NIPT analyzes fetal DNA in the mother’s blood, a non-invasive prenatal test. These advancements improve diagnosis and management, giving families new options.
Conclusion: The Genetic Basis of Sickle Cell Anemia and Future Directions
Understanding sickle cell anemia’s genetic basis is key to finding better treatments. This disease is caused by a mutation in the HBB gene, leading to abnormal hemoglobin. Research has greatly improved our knowledge and opened doors to new treatments.
The mutation in sickle cell anemia changes a single nucleotide in the β-globin gene. This change substitutes glutamic acid with valine. It’s inherited in an autosomal recessive pattern. For more details, check out studies on the National Center for Biotechnology Information website.
Looking ahead, research focuses on gene therapy, new medicines, and better diagnostic tools. These efforts aim to better manage sickle cell anemia and improve life for those affected. Our goal is to advance healthcare and support, ensuring top-notch care for all.
FAQ
What type of genetic mutation causes sickle cell anemia?
Sickle cell anemia is caused by a specific point mutation in the HBB gene on chromosome 11. This mutation leads to abnormal hemoglobin S production.
Is sickle cell anemia an autosomal recessive condition?
Yes, sickle cell anemia is an autosomal recessive condition. This means an individual must inherit two copies of the mutated HBB gene to express the disease.
What is the role of the HBB gene in normal hemoglobin production?
The HBB gene encodes the beta-globin subunit of hemoglobin. It’s vital for red blood cells to function properly and transport oxygen.
How does the mutation in the HBB gene lead to sickle cell anemia?
The mutation changes a single nucleotide (GAG to GTG). This change alters the beta-globin chain, leading to abnormal hemoglobin S production.
What are the biochemical properties of hemoglobin S?
Hemoglobin S tends to polymerize under low oxygen conditions. This causes red blood cells to sickle, damaging the membrane over time.
What are the clinical manifestations of sickle cell anemia?
The disease causes episodes of pain and anemia. It also leads to red blood cell deformation and premature destruction.
Are carriers of the sickle cell trait at risk of developing the disease?
Generally, carriers of the sickle cell trait are asymptomatic. They can pass the mutated gene to their offspring and may face health issues, including a known resistance to malaria.
What genetic testing methods are available for diagnosing sickle cell anemia?
Prenatal and newborn screening methods diagnose sickle cell anemia. Genetic counseling is recommended for affected families to understand risks and probabilities of disease transmission.
What is the significance of understanding the genetic basis of sickle cell anemia?
Understanding the genetic defect is key for diagnosis, management, and new treatments. It highlights the need for ongoing research and advancements in genetic testing and counseling.
Reference
- Rees, D. C., Williams, T. N., & Gladwin, M. T. (2010). Sickle-cell disease. Lancet, 376(9757), 2018-2031.
https://www.sciencedirect.com/science/article/pii/S0140673610607072