Last Updated on November 27, 2025 by Bilal Hasdemir

It’s important for patients and their families to know the difference between astrocytoma and glioblastoma. This knowledge helps in making better treatment choices.
At Liv Hospital, we focus on the latest treatments and care for brain tumor patients. Astrocytoma and glioblastoma come from astrocytes. But, they differ a lot in how aggressive they are and how likely they are to be cured.
We believe in giving patients the information they need to understand their conditions. In this article, we’ll look at the main differences between these brain tumors. This will help you feel more confident as you go through your treatment.
Key Takeaways
- Understanding the differences between astrocytoma and glioblastoma is key for making good treatment choices.
- Both tumors start from astrocytes but are not the same in how aggressive they are.
- The outlook for each tumor type is very different.
- Liv Hospital is committed to the newest treatments and caring for patients with brain tumors.
- Helping patients understand their conditions is essential for their treatment journey.
Understanding Brain Tumors: Astrocytic Origins
It’s key to know how brain tumors start from astrocytes to understand the difference between astrocytoma and glioblastoma. Both are gliomas, which come from glial cells in the brain. They start from astrocytes, important cells that help the brain work right.
What Are Astrocytes and Their Function
Astrocytes are star-shaped cells that help neurons. They give nutrients to neurons, keep the blood-brain barrier strong, and control chemicals around neurons. Without them, the brain can’t function well.
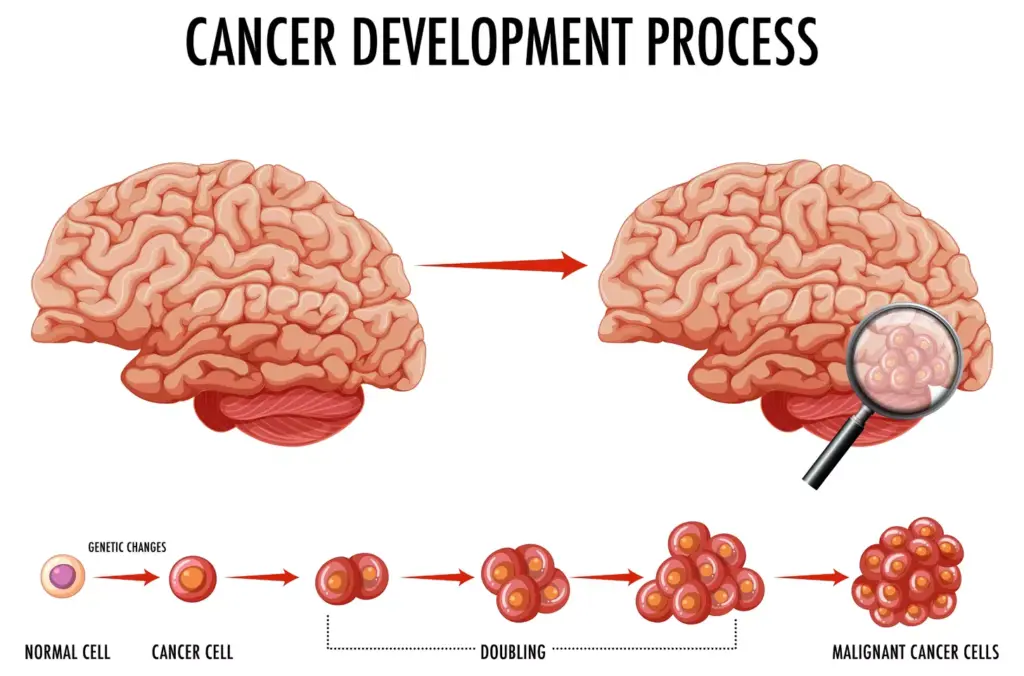
How Astrocytic Tumors Develop
Astrocytic tumors, like astrocytomas and glioblastomas, start when astrocytes grow out of control. This happens because of genetic changes. These changes can come from genes, radiation, or the environment.
Going from normal astrocytes to tumor cells takes several steps. These include losing control, growing too much, and spreading to other brain areas. Knowing these steps helps doctors find better treatments.
| Characteristics | Astrocytes | Astrocytic Tumors |
|---|---|---|
| Cell Shape | Star-shaped | Variable, often irregular |
| Function | Support and nourish neurons | Uncontrolled growth, invasive |
| Genetic Stability | Normal genetic regulation | Genetic mutations, instability |
The WHO Classification System: From Astrocytoma to Glioblastoma

The World Health Organization (WHO) has a system for classifying astrocytomas. This system helps doctors know how aggressive a tumor is. It also helps decide the best treatment for patients.
The WHO grading system goes from grade 1 to grade 4. Grade 1 is the least aggressive, and grade 4 is the most aggressive.
Grade 1-2: Low-Grade Astrocytomas
Low-grade astrocytomas are slow-growing and less aggressive. Grade 1 astrocytomas are often benign and can be cured with surgery alone.
Grade 2 astrocytomas are also low-grade but can turn into more aggressive tumors over time.
Grade 3: Anaplastic Astrocytoma
Anaplastic astrocytoma, or grade 3 astrocytoma, is more malignant. These tumors have more cells, more cell division, and abnormal cells compared to lower-grade tumors.
Patients with anaplastic astrocytoma need aggressive treatments like radiation, chemotherapy, and surgery.
Grade 4: Glioblastoma Multiforme (GBM)
Glioblastoma multiforme (GBM), classified as grade 4 astrocytoma, is the most aggressive. GBM grows fast, has dead cells, and lots of blood vessels.
Even with new treatments like surgery, radiation, and chemotherapy, GBM is hard to treat and has a poor prognosis.
Knowing the WHO classification system is key for doctors to choose the right treatment. It also helps patients understand their diagnosis and what to expect.
Key Difference #1: Cellular Structure and Histology
Distinguishing astrocytoma from glioblastoma starts with their unique cells and tissue patterns. These differences help us understand the unique nature of each brain tumor.
We will look at the cells in astrocytoma and glioblastoma. We’ll see how their cells and tissues differ.
Astrocytoma Cell Characteristics
Astrocytomas have different cell types. Their cells can look like normal astrocytes or be more abnormal. The key features of astrocytomas include:
- Cellular atypia
- Mitotic activity
- Microvascular proliferation
- Necrosis (in higher grades)
The grade of an astrocytoma shows how aggressive it is. Higher grades mean the tumor is more aggressive.
Glioblastoma’s Distinctive Features
Glioblastoma, or glioblastoma multiforme (GBM), is very aggressive. It has unique features that make it stand out. The main characteristics of glioblastoma are:
- Necrosis with pseudopalisading nuclei
- Microvascular proliferation
- High mitotic activity
- Significant cellular pleomorphism
These traits make glioblastoma the most aggressive type of astrocytic tumor.
Key Difference #2: Growth Rate and Invasiveness
It’s important to know how astrocytomas and glioblastomas grow and spread. This helps doctors choose the best treatment. The way these tumors grow affects how well a patient does.
Astrocytoma’s Slower Growth Pattern
Astrocytomas, like low-grade ones, grow slower than glioblastomas. This slower growth means symptoms come on more gradually. This can lead to earlier treatment and better results.
A leading neuro-oncologist says, “The slower growth of low-grade astrocytomas gives us a chance to act early. This can prevent serious brain damage.”
Lower-grade astrocytomas usually have clear edges. This makes surgery easier. But, they can grow unpredictably. So, doctors need to keep a close eye on them and adjust treatment plans as needed.
Glioblastoma’s Rapid and Infiltrative Nature
Glioblastomas, on the other hand, grow fast and spread into the brain. Their aggressive nature makes them hard to treat. Their edges blend with normal brain tissue, making surgery tricky.
A study found, “Glioblastoma’s fast growth leads to many recurrences, even after treatment seems to work.” This shows the need for strong, multi-faceted treatments for glioblastoma.
Glioblastomas need quick and strong treatment. Despite the challenges, new research and treatments give hope for better outcomes for glioblastoma patients.
Key Difference #3: Genetic and Molecular Profiles
It’s important to know the genetic and molecular differences between astrocytomas and glioblastomas. We’ll look at IDH mutations, chromosomal changes, and MGMT methylation status. These factors help us tell these brain tumors apart.
IDH Mutations in Astrocytomas
IDH mutations are more common in lower-grade astrocytomas. These changes in the IDH1 and IDH2 genes are linked to a better outlook. Knowing about IDH mutations helps doctors decide on treatments.
Chromosomal Alterations in Glioblastomas
Glioblastomas have different genetic changes. These changes, like amplifications and deletions, make glioblastomas aggressive. Understanding these genetic shifts is key to finding new treatments.
MGMT Methylation Status
The MGMT gene is important for fixing DNA damage. Methylation of the MGMT promoter affects how well some treatments work, like temozolomide. The MGMT methylation status differs between astrocytomas and glioblastomas, impacting treatment success.
To show the genetic and molecular differences, let’s look at a table:
| Genetic/Molecular Feature | Astrocytomas | Glioblastomas |
|---|---|---|
| IDH Mutations | More common in lower-grade astrocytomas | Less frequent, more often in secondary glioblastomas |
| Chromosomal Alterations | Fewer alterations, often with different patterns | Multiple amplifications, deletions, and translocations |
| MGMT Methylation Status | Variable, can influence treatment response | Often associated with treatment resistance if unmethylated |
By studying the genetic and molecular profiles, we can better understand these tumors. This knowledge helps us create more effective treatments.
Key Difference #4: Age Demographics and Risk Factors
Astrocytomas and glioblastomas have different age groups, affecting risk and treatment. Knowing these differences is key for diagnosis and care.
Typical Age Range for Astrocytoma Diagnosis
Astrocytomas can happen in anyone from kids to adults in their 40s and 50s. Low-grade astrocytomas often strike in the 30s and 40s. Grade 3 astrocytomas appear a bit later, in the 40s and 50s.
Genetic factors and some environmental exposures can increase the risk of getting an astrocytoma. But, the exact environmental links are not as clear as they are for other cancers.
Glioblastoma’s Prevalence in Older Adults
Glioblastoma, or grade 4 astrocytoma, mainly hits older adults. It’s most common between 50 and 80 years old, with most cases in those over 65. This age pattern sets glioblastoma apart from lower-grade astrocytomas.
Older age and certain genetic changes raise the risk of glioblastoma. Ionizing radiation is also a known risk factor. The astrocytic glioma group, which includes glioblastoma, has a mix of genetic and environmental causes.
In summary, astrocytomas can happen at any age, but glioblastomas mainly affect older adults. This age difference is vital for diagnosing and treating these tumors.
- Astrocytomas can occur in children and young adults, with a peak incidence in the third to fourth decade.
- Glioblastoma is more common in older adults, typically between 50 and 80 years old.
- Age is a significant risk factor for glioblastoma, with incidence increasing with age.
Understanding these age-related differences helps doctors tailor treatments. This approach can lead to better outcomes for those with these brain tumors.
Astrocytoma vs Glioblastoma: Key Difference #5 – Clinical Presentation
The symptoms of astrocytoma and glioblastoma are quite different. This is because of their unique growth patterns and levels of cancer. Knowing these symptoms is key to diagnosing these brain tumors. It helps doctors decide on the right tests and treatments.
Common Symptoms of Lower-Grade Astrocytomas
Lower-grade astrocytomas (Grade 1-2) show symptoms that are not as obvious. These symptoms come on slowly. Some common signs include:
- Seizures
- Mild headaches
- Nausea and vomiting
- Changes in personality or mood
- Weakness or numbness in parts of the body
The symptoms depend on where the tumor is and how it affects the brain. For example, tumors near motor areas can cause weakness. Tumors in the frontal area might change a person’s personality.
Distinctive Signs of Glioblastoma
Glioblastoma (Grade 4 astrocytoma) shows symptoms that are more severe and happen quickly. Some common signs are:
- Severe headaches that worsen over time
- Confusion and disorientation
- Memory loss
- Personality changes
- Vision problems
- Seizures (more frequent and severe than in lower-grade astrocytomas)
Glioblastoma grows fast, which can lead to increased pressure in the brain. This causes the symptoms to be more noticeable.
| Symptom | Lower-Grade Astrocytoma | Glioblastoma |
|---|---|---|
| Onset | Gradual | Rapid |
| Headaches | Mild to moderate | Severe |
| Seizures | Less frequent | More frequent and severe |
| Cognitive Symptoms | Mild changes | Confusion, memory loss |
It’s important for doctors to know these differences. This helps them make the right diagnosis and treatment plan. The symptoms of astrocytoma and glioblastoma show their different types and how they grow. This highlights the need to look at both the tumor’s grade and location when assessing a patient.
Key Difference #6: Prognosis and Survival Rates
Astrocytoma and glioblastoma have different survival rates. These rates are influenced by many factors. Knowing these differences helps patients and doctors make better treatment plans.
Survival Statistics for Different Grades of Astrocytoma
The outlook for astrocytoma changes with the tumor grade. Low-grade astrocytomas (Grade 1-2) often have a better chance of long-term survival. Studies show that the 5-year survival rate for these tumors can be between 50% and 90%. This depends on age, where the tumor is, and how much of it is removed.
On the other hand, higher-grade astrocytomas face a tougher road. As the grade goes up, survival chances go down. Grade 3 astrocytomas fall somewhere in between low-grade ones and glioblastoma in terms of survival.
| Tumor Grade | 5-Year Survival Rate |
|---|---|
| Grade 1 | 70-90% |
| Grade 2 | 50-70% |
| Grade 3 | 20-50% |
Glioblastoma’s 15-Month Median Survival
Glioblastoma multiforme (GBM), or Grade 4 astrocytoma, has a very poor outlook. Despite aggressive treatment, the median survival is about 15 months. The 5-year survival rate for GBM is under 10%. This poor prognosis is due to the tumor’s fast growth, its spread into surrounding brain tissue, and its resistance to treatments.
Factors Affecting Prognosis
Many factors affect the outlook for astrocytoma and glioblastoma. These include IDH mutation status, MGMT promoter methylation, age, how well the patient is doing, and how much of the tumor is removed. Patients with IDH-mutant tumors tend to do better than those without. For more on how molecular factors impact prognosis, see this research paper on glioblastoma’s molecular traits.
Grasping these prognostic factors is key to creating personalized treatment plans. It also helps in setting realistic hopes for outcomes.
Key Difference #7: Treatment Approaches and Effectiveness
It’s important to know how astrocytomas and glioblastomas are treated. The treatment plans differ based on the tumor’s grade, location, and other factors.
Standard Treatment Protocols for Astrocytoma
Lower-grade astrocytomas often start with surgery to remove as much of the tumor as possible. Adjuvant therapies like radiation and chemotherapy might be suggested based on the tumor and patient’s health.
If the tumor can’t be fully removed or is in a sensitive area, partial resection or biopsy followed by radiation might be chosen. The goal is to slow the tumor’s growth and ease symptoms.
Aggressive Treatment Strategies for Glioblastoma
Glioblastoma, the most aggressive astrocytic tumor, needs a more intense treatment. The usual treatment is maximal safe surgical resection followed by concurrent chemoradiation with temozolomide, a chemotherapy drug.
After chemoradiation, patients usually get adjuvant temozolomide for months. This aggressive method tries to slow the tumor’s growth and increase survival chances.
Recurrence Patterns and Management
Glioblastomas often come back, even with aggressive treatment. Managing recurrence depends on the tumor’s features, the patient’s health, and past treatments. Options include re-resection, re-irradiation, or different chemotherapy plans.
For astrocytomas, recurrence is less common, mainly for lower-grade ones. When it does happen, treatment choices are based on the initial treatment and the tumor’s current state.
Knowing about these treatments and their success is key for managing patient hopes and making informed care decisions.
Diagnostic Methods: Differentiating Between Tumor Types
Diagnosing astrocytomas and glioblastomas requires a detailed approach. We use the latest imaging and molecular analysis. Accurate diagnosis is key to finding the best treatment and improving patient care.
Advanced Imaging Techniques
Advanced imaging is essential for diagnosing these tumors. Magnetic Resonance Imaging (MRI) is a main tool in neuro-oncology. It shows where the tumor is, how big it is, and what it looks like.
We use MRI with different sequences to get detailed information. This helps us understand the tumor better.
Positron Emission Tomography (PET) and Computed Tomography (CT) scans also help. They show how active the tumor is and if it has spread.
Biopsy and Histopathological Analysis
Imaging gives us clues, but a biopsy is needed for a final diagnosis. We look at a tissue sample under a microscope. This helps us see the tumor’s structure and specific features.
Looking at the tissue sample, we can see things like how abnormal the cells are and if there’s cell death. These details help us grade the tumor and tell it apart from others.
Molecular and Genetic Testing
Molecular and genetic testing are also key. We check tumor samples for specific genetic changes. For example, IDH1 and IDH2 mutations are often found in lower-grade astrocytomas.
We also look at MGMT promoter methylation status. This gives us important information about the tumor’s behavior. By combining this with what we see under the microscope, we get a full picture of the tumor.
By using advanced imaging, biopsy, histopathology, and molecular testing, we can accurately diagnose and tell apart astrocytomas and glioblastomas. This helps us create personalized treatment plans.
Conclusion: Navigating the Spectrum of Astrocytic Tumors
It’s important to know the difference between astrocytomas and glioblastomas. We’ve looked at how they differ, from their cells to how they grow and their treatment options.
When comparing astrocytoma vs glioblastoma multiforme, we see big differences. Astrocytomas can be mild or severe, but glioblastoma is the most aggressive. This affects how long a patient might live.
Knowing about astrocytoma vs GBM helps patients make better choices. Our team offers top-notch care and support. We help patients through every step of their treatment.
Understanding each tumor’s unique traits helps us improve care. Whether it’s astrocytoma or glioblastoma, our team is here to help. We guide patients to the best treatment plans.
FAQ
What is the main difference between astrocytoma and glioblastoma?
Astrocytoma and glioblastoma are brain tumors from astrocytes. Astrocytomas vary in aggressiveness and growth rate. Glioblastoma is the most aggressive, with a poor prognosis.
How are astrocytomas and glioblastomas classified?
The World Health Organization (WHO) classifies these tumors. They grade them from 1 to 4. Grade 1 is the least aggressive, and grade 4 is the most.
What are the typical symptoms of astrocytoma and glioblastoma?
Symptoms vary by tumor location and grade. Lower-grade astrocytomas may cause seizures and headaches. Glioblastoma symptoms are more severe, including cognitive decline and increased pressure.
How do IDH mutations affect the prognosis of astrocytoma and glioblastoma?
IDH mutations are genetic changes in these tumors. Tumors with IDH mutations have a better prognosis. They are more common in lower-grade astrocytomas and secondary glioblastomas.
What are the treatment options for astrocytoma and glioblastoma?
Treatment varies by tumor grade, location, and genetics. Low-grade astrocytomas may be treated with surgery or observation. High-grade tumors require surgery, radiation, and chemotherapy.
How do the genetic and molecular profiles of astrocytoma and glioblastoma differ?
Astrocytomas and glioblastomas have different genetic and molecular profiles. Glioblastomas often have chromosomal changes like EGFR amplification. Astrocytomas, with IDH mutations, have a distinct molecular profile.
What is the significance of MGMT methylation status in glioblastoma?
MGMT methylation status predicts a glioblastoma’s response to chemotherapy. Tumors with MGMT methylation are more likely to respond to temozolomide.
Can astrocytoma become glioblastoma?
Yes, lower-grade astrocytomas can progress to glioblastoma. This is called secondary glioblastoma. Primary glioblastoma arises without a lower-grade tumor.
What is the role of advanced imaging techniques in diagnosing astrocytoma and glioblastoma?
Advanced imaging, like MRI and PET scans, is key in diagnosis. They help identify tumor characteristics, such as location and size.
How do age demographics impact the risk of developing astrocytoma and glioblastoma?
Age is a big risk factor. Glioblastoma is common in older adults, 50 to 80 years old. Astrocytoma can occur at any age, depending on the grade.
References
- Seifert, M., et al. (2015). Comparative transcriptomics reveals similarities and differences between glioma progression. [Article]. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4682229/ PMC
- J. Zhang, Y. Feng, W. Hua, et al. (2023). Distinct aneuploid evolution of astrocytoma and glioblastoma during recurrence. npj Precision Oncology, 7, Article 97. Retrieved from https://www.nature.com/articles/s41698-023-00453-1 Nature