Last Updated on November 27, 2025 by Bilal Hasdemir
At Liv Hospital, we are dedicated to giving top-notch care and hope to those with meningioma. The meningioma survival rate is very high for brain tumors. More than 90 percent of adults between 20 and 44 survive at least five years after being diagnosed.
Thanks to modern treatments, the meningioma prognosis has gotten much better. Getting a brain tumor diagnosis can be scary. But we’re here to support and guide you through treatment.
Key Takeaways
- Meningioma has a high survival rate, mostly for adults aged 20 to 44.
- Modern therapies have improved the overall meningioma prognosis.
- The survival rate for benign meningiomas is generally positive.
- Liv Hospital is committed to providing world-class healthcare for international patients.
- Understanding the key facts about meningioma survival rate and prognosis is key for patients.
Understanding Meningiomas: Types and Classifications
Meningiomas are tumors that grow from the meninges. These are protective membranes around the brain and spinal cord. Knowing their types and classifications is key to understanding treatment and prognosis.
What Are Meningiomas?
Meningiomas are usually benign tumors from the meninges. They can grow at different rates. Many are found by chance during scans for other reasons.
The type of meningioma, benign or malignant, affects prognosis and life expectancy. For example, benign meningiomas have a 97 percent 5-year survival rate for younger adults and over 87 percent for adults over 40. Age is a big factor in how well a patient does.
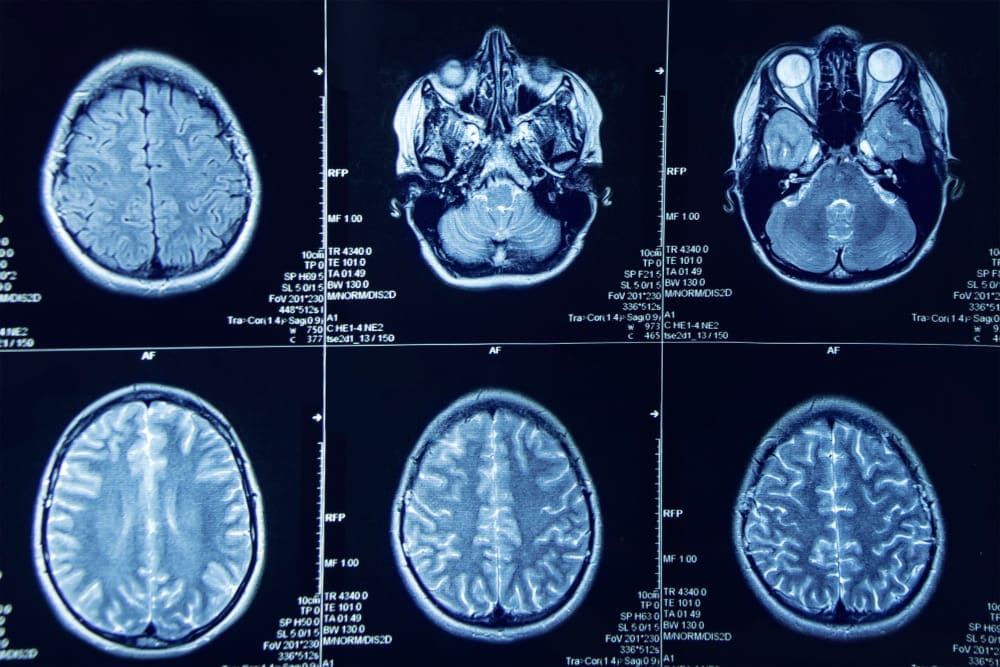
WHO Classification System for Meningiomas
The World Health Organization (WHO) has a system for meningioma grades. This system is based on the tumor’s appearance under a microscope. It helps doctors decide on the best treatment.
The WHO grades meningiomas from I to III. Grade I is the most common and usually benign. Grade II has atypical features and a higher chance of coming back. Grade III is malignant and grows faster.
Benign vs. Malignant Meningiomas
It’s important to know if a meningioma is benign or malignant. Benign ones usually have a good prognosis with surgery. Malignant ones need more aggressive treatment and have a worse outlook.
Understanding a meningioma’s specific traits is vital for the right treatment. The prognosis depends a lot on the type and the patient’s health. Accurate diagnosis and classification are essential for better treatment and benign meningioma life expectancy.
Meningioma Survival Rate: Detailed Statistics

Meningioma survival rates vary based on age and tumor grade. Knowing these stats is key for patients and doctors to make smart treatment choices.
Overall 5-Year Survival Rates
The 5-year survival rate for meningioma patients is quite good. Studies show that benign meningiomas have a 90% or higher survival rate. But, malignant meningiomas have a much lower rate, between 50% to 70%.
Key Statistics:
- Benign Meningiomas (Grade I): 91% 5-year survival rate
- Atypical Meningiomas (Grade II): 70-80% 5-year survival rate
- Anaplastic Meningiomas (Grade III): 50-60% 5-year survival rate
Survival Rates by Age Group
Age greatly affects meningioma survival rates. Younger patients usually have better chances than older ones. Research shows that those under 40 tend to do better than those older.
Age-Specific Survival Rates:
- Patients under 40: Higher survival rates, often above 90% for benign meningiomas
- Patients between 40-60: Average survival rates, typically ranging from 80-90%
- Patients over 60: Lower survival rates, often due to comorbidities and more aggressive tumor behavior
Comparing Survival Rates to Other Brain Tumors
Meningiomas, and benign ones in particular, have very high survival rates. They are among the top in brain tumor survival rates. This means meningioma patients usually have a better outlook than those with other brain tumors.
“The survival rate for meningioma patients is among the highest for brain tumors, with benign meningiomas having a 5-year relative survival rate of over 90%.” – Source: American Brain Tumor Association
By grasping these detailed statistics, patients and doctors can better handle meningioma diagnosis and treatment. This leads to better outcomes for everyone involved.
Benign Meningioma Life Expectancy
Knowing how long people with benign meningiomas can live is key. These tumors, usually Grade I, have a good outlook for those who get them. This makes choosing the right treatment very important.
Grade I Meningioma Survival Statistics
Grade I meningiomas grow slowly and rarely turn cancerous. This makes the future look bright for those with them. Research shows that about 90% of people with these tumors live for five years or more.
Removing these tumors completely greatly boosts survival chances. How well the surgery goes is a big deal for how long someone can live after surgery.
Long-term Outlook After Diagnosis
For most people with benign meningiomas, the outlook is very good. With the right treatment, many can live for years after finding out they have the tumor.
Factors Influencing Long-term Survival:
- Completeness of surgical removal
- Patient’s overall health and age
- Tumor location and accessibility
Factors That Improve Survival for Benign Meningiomas
Several things help people with benign meningiomas live longer. Early detection, good surgery, and watching closely after surgery are all key.
| Factor | Impact on Survival |
|---|---|
| Complete Surgical Removal | Significantly improves long-term survival |
| Patient Age | Younger patients tend to have better outcomes |
| Tumor Location | Tumors in accessible locations have better prognosis |
By knowing these factors and teaming up with doctors, patients can make their treatment plans better. This can help them live longer with benign meningiomas.
Malignant Meningioma Prognosis
Understanding the prognosis of malignant meningiomas is key for patients and doctors. Malignant meningiomas, like atypical and anaplastic types, have a different outlook than benign ones.
Atypical (Grade II) Meningioma Survival Rates
Atypical meningiomas, classified as Grade II by the WHO, tend to come back more often than benign ones. The 5-year survival rate for these patients varies a lot.
- Recurrence Rates: They have higher recurrence rates, from 29% to 41% at 5 years.
- Survival Rates: The 5-year survival rate is generally lower, from 70% to 80%.
Anaplastic (Grade III) Meningioma Survival Rates
Anaplastic meningiomas, or Grade III, are the most aggressive. They have a poor outlook due to high recurrence rates and fast growth.
- Survival Rates: The 5-year survival rate for anaplastic meningioma patients is much lower, between 30% to 50%.
- Prognostic Factors: How much of the tumor is removed, patient age, and tumor location are key in determining the prognosis.
Improvements in Survival with Modern Therapies
Modern treatments have shown promise in improving survival for malignant meningiomas. Advances in surgery, radiation therapy, and new treatments are leading to better outcomes.
- Advanced Surgical Techniques: New surgical methods and tools help remove more tumor safely.
- Radiation Therapy: Stereotactic radiosurgery has become more precise, controlling tumor growth better.
- Emerging Treatments: Research into targeted and immunotherapies may further improve survival rates.
Thanks to these advancements, the outlook for malignant meningioma patients is slowly getting better. While there are challenges, the future looks more hopeful.
Factors Affecting Meningioma Prognosis
It’s important to know what affects meningioma prognosis. This includes both the tumor itself and the patient’s health. Understanding these factors helps both patients and doctors.
Tumor Location and Accessibility
The location of a meningioma greatly affects its prognosis. Tumors near important brain areas or big blood vessels are harder to treat. Accessibility is key for surgery success. Tumors that are easy to reach usually have better results than those in hard-to-reach places.
Patient Age and Overall Health
Patient age and health are big factors in meningioma prognosis. Younger patients with fewer health problems usually do better. Older patients or those with serious health issues might face more risks and slower recovery.
We look at these factors when planning treatment and predicting results.
Genetic and Molecular Markers
New research has found genetic and molecular markers that affect meningioma prognosis. Some genetic changes or expressions mean a tumor might come back or grow faster. Knowing these markers helps us make treatment plans that fit each patient’s needs better.
By looking at tumor location, patient age and health, and genetic markers, we can give more accurate prognoses. This helps us create better treatment plans for meningioma patients.
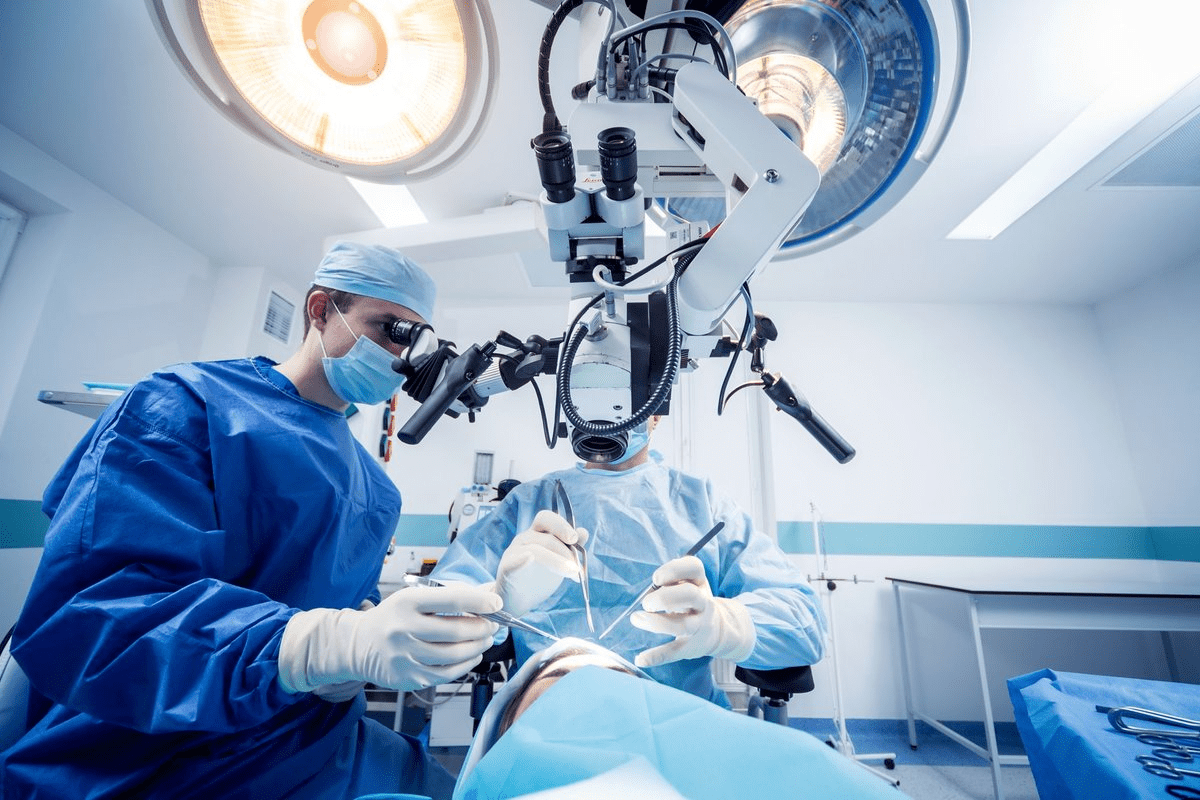
Meningioma Surgery Success Rate
Meningioma surgery has a high success rate, thanks to complete resection. This leads to fewer recurrences and better patient results. The field has grown, with new techniques and technology improving care.
Outcomes Based on Extent of Resection
The success of meningioma surgery depends on how much of the tumor is removed. Complete resection means lower chances of the tumor coming back. It also means better survival rates compared to removing only part of the tumor.
| Extent of Resection | 5-Year Recurrence Rate | 10-Year Survival Rate |
|---|---|---|
| Complete Resection | 10% | 85% |
| Partial Resection | 30% | 60% |
Simpson Grading System and Its Implications
The Simpson Grading System helps predict how likely a meningioma will come back. It rates the surgery from I (complete removal) to V (just a simple decompression).
- Grade I: Complete removal including affected dura and bone
- Grade II: Complete removal with coagulation of dural attachment
- Grade III: Complete removal without coagulation or resection of dural attachment
- Grade IV: Partial removal
- Grade V: Simple decompression
Surgical Complications and Mortality
Meningioma surgery is usually safe, but complications can happen. These include infection, nerve damage, and fluid leaks. Thanks to better techniques, death rates have gone down.
Advancements in Surgical Techniques
New tools like intraoperative MRI and neuronavigation have made surgery better. They help doctors find and remove tumors more accurately. This reduces the risk of problems during surgery.
Thanks to these advancements, meningioma surgery is getting even better. New techniques and technology are improving patient care and our understanding of meningioma treatment.
Life Expectancy After Meningioma Surgery
Patients often wonder about their life expectancy after meningioma surgery. The prognosis depends on the meningioma type, surgery success, and overall health.
Short-term Recovery and Survival
Recovery after meningioma surgery is key for long-term health. Most patients see symptom improvement in weeks to months. But, there’s a risk of complications and death, mainly right after surgery.
Factors influencing short-term survival include:
- The extent of tumor resection
- The patient’s age and overall health
- The presence of any surgical complications
Long-term Survival After Complete Resection
Complete removal of the meningioma leads to better long-term survival. Studies show patients with gross total excision have a high five-year survival rate.
For example, the five-year survival rate for atypical meningiomas after complete removal is over 90 percent. This offers patients a hopeful outlook.
Survival After Subtotal Resection with Adjuvant Therapy
When complete removal isn’t possible, subtotal resection with adjuvant therapy is a good option. Adjuvant therapies, like radiation, help control tumor growth, improving survival chances.
The table below shows survival rates for different meningioma treatments:
| Treatment Type | 5-Year Survival Rate | 10-Year Survival Rate |
|---|---|---|
| Complete Resection | 95% | 85% |
| Subtotal Resection with Adjuvant Therapy | 80% | 65% |
| Subtotal Resection Alone | 60% | 40% |
Knowing these survival rates helps patients and families make informed treatment choices. It gives them a better idea of what to expect after surgery.
Non-Surgical Treatment Outcomes
Non-surgical treatments are now key in managing meningiomas. They offer patients options other than surgery. Thanks to new medical tech and treatment methods, these non-surgical options are playing a bigger role in meningioma care.
Radiation Therapy Success Rates
Radiation therapy is a big help for meningiomas that can’t be removed or have leftover disease after surgery. Research shows it can control tumors well, with success rates depending on the tumor’s type and where it is. For benign meningiomas, radiation therapy often gets over 90% control at 5 years.
New radiation methods like IMRT and proton therapy are making treatments more precise. This helps protect healthy tissues around the tumor.
Stereotactic Radiosurgery Outcomes
Stereotactic radiosurgery (SRS) is a non-surgical choice for treating meningiomas, mainly for small to medium-sized ones. SRS gives a focused radiation dose to the tumor, saving the brain around it. Results for SRS are good, with high tumor control and low complication rates.
Our data shows SRS works well for meningiomas near important brain areas. Surgery there could be risky.
Emerging Treatments and Clinical Trials
New treatments for meningiomas are being tested in clinical trials. These include targeted therapies, immunotherapies, and new radiation methods. Targeted therapies target specific weaknesses in meningioma cells, aiming for better and safer treatments.
We’re excited about the progress in clinical trials. They’re giving us new views on meningioma biology and possible treatments. As research keeps moving forward, we expect these new therapies to improve patient outcomes.
Recurrence Rates and Management
The chance of meningioma coming back depends on several things. These include how surgery is done and the tumor’s characteristics. Knowing these helps in making better treatment plans and improving results for patients.
Recurrence After Complete Surgical Removal
Even if a meningioma is fully removed, it can come back. The rate of coming back depends on the tumor’s grade and how much of it was removed. Studies show that Grade I meningiomas have a lower chance of coming back than higher-grade ones.
A study in the Journal of Neurosurgery found that Grade I meningiomas have a 5-year recurrence rate of about 7-20%. But, Grade II and III meningiomas have much higher rates, at 30-50% and 50-80%, respectively.
Recurrence After Partial Resection
When only part of a meningioma is removed, the risk of it coming back is higher. The leftover tumor can grow, leading to recurrence. Adjuvant therapies like radiation therapy might be suggested to lower this risk.
| Tumor Grade | Recurrence Rate After Complete Resection | Recurrence Rate After Partial Resection |
|---|---|---|
| Grade I | 7-20% | 30-60% |
| Grade II | 30-50% | 50-80% |
| Grade III | 50-80% | 80-100% |
Factors Increasing Recurrence Risk
Several things can make meningioma more likely to come back, including:
- Tumor Location: Tumors near important structures are harder to remove fully.
- Tumor Grade: Higher-grade tumors are more likely to come back.
- Surgical Technique: How much of the tumor is removed and the surgical methods used can affect recurrence rates.
Treatment Approaches for Recurrent Meningiomas
Handling recurrent meningiomas needs a team effort. Treatment choices might include:
- Reoperation: Removing the coming-back tumor surgically.
- Radiation Therapy: To slow down tumor growth and ease symptoms.
- Stereotactic Radiosurgery: A precise radiation therapy focusing on the tumor.
We stress the need for aggressive surgery and additional treatments to reduce recurrence and better patient outcomes. By knowing what affects recurrence, doctors can tailor treatments to manage meningioma recurrence well.
Quality of Life and Functional Outcomes
Medical technology keeps getting better, and so does our focus on life quality after meningioma treatment. We know patients with meningiomas can live well after treatment. Our goal is to care for them fully, covering their physical, emotional, and mental needs.
Research shows that after treatment, many patients see better neurological and cognitive function. This lets them get back to their usual lives. But, how much they recover can depend on the meningioma type, treatment success, and their health.
Neurological Function After Treatment
Neurological function is key to a patient’s recovery after meningioma treatment. Many see big improvements in their neurological function after surgery or radiation. For example, those who have successful surgery often feel better from symptoms like seizures or weakness.
- Improved symptom management: Many patients see their symptoms lessen after treatment.
- Enhanced neurological function: Some regain strength or feel sensations they lost.
- Variability in outcomes: Recovery can differ a lot from one patient to another.
Cognitive Outcomes and Recovery
Cognitive function after meningioma treatment is also very important. Studies show many patients get better mentally after treatment. But, how much they improve can depend on the tumor’s location, the patient’s age, and any mental health issues they had before.
A good rehab program can really help with mental recovery. This might include therapy, physical therapy, and other support tailored to the patient.
Return to Normal Activities
Getting back to normal after meningioma treatment is a big concern for patients. While it’s tough, many can get back to their daily lives, including work and hobbies.
The secret to getting back to normal is a good rehab plan and support from healthcare. We help our patients create recovery plans that meet their specific needs and goals.
Psychological Impact and Support
The emotional impact of a meningioma diagnosis is huge. Patients often feel anxious, depressed, or face other emotional challenges. It’s vital to offer strong psychological support.
We provide counseling, support groups, and other resources to help patients deal with their emotional struggles. By recognizing the emotional toll of meningioma and supporting them, we can improve their overall quality of life.
Conclusion: Advances in Meningioma Treatment and Survival
There have been big steps forward in treating meningiomas. This has led to better survival rates and outlooks for patients. New surgical methods and radiation therapy have made a big difference.
The future for meningioma treatment is bright. Research and new treatments are giving patients new hope. Advances in surgery, like less invasive methods, have cut down recovery times and made life better for patients.
As we keep exploring new medical frontiers, survival rates for meningiomas will likely get even better. It’s key for patients to get the best care, including the newest treatments and support. This helps them get the best results.
By leading in meningioma research and treatment, we can make a big difference in patients’ lives. We aim to give them the best chance to survive and live normally again.
FAQ
What is the overall survival rate for meningioma patients?
Most meningioma patients have a good chance of survival. For those aged 20 to 44, the 5-year survival rate is about 95% or higher.
How does the survival rate vary by age for meningioma patients?
Survival rates change with age. Younger patients (20-44 years) have better 5-year survival rates. Older patients face lower survival rates.
What is the difference between benign and malignant meningiomas?
Benign meningiomas (Grade I) grow slowly and have a better prognosis. Malignant meningiomas (Grade II and III) grow faster and have a worse prognosis.
How does the WHO classification system impact meningioma prognosis?
The WHO system grades meningiomas based on their features. Higher grades mean more aggressive tumors and worse outcomes.
What is the life expectancy for patients with benign meningiomas?
Patients with benign meningiomas (Grade I) usually have a normal life expectancy. This is true if the tumor is completely removed.
What are the survival rates for atypical and anaplastic meningiomas?
Atypical meningiomas (Grade II) have a 5-year survival rate of about 70-80%. Anaplastic meningiomas (Grade III) have a 5-year survival rate of around 30-50%.
How does tumor location affect meningioma prognosis?
Where the tumor is located greatly affects the prognosis. Tumors in easy-to-reach areas have better outcomes. Tumors in hard-to-reach areas may have poorer outcomes due to higher surgical risks.
What is the success rate of meningioma surgery?
Surgery for meningiomas is usually successful, mainly for benign tumors. Complete removal of the tumor leads to a high cure rate and low recurrence rates.
How does the Simpson Grading System correlate with survival?
The Simpson Grading System rates how well a meningioma is removed. Higher grades mean less complete removal and potentially worse survival.
What are the outcomes of radiation therapy for meningiomas?
Radiation therapy, like stereotactic radiosurgery, can control meningioma growth. It’s effective for residual or recurrent tumors. Success rates depend on the tumor and treatment specifics.
How common is meningioma recurrence after treatment?
Recurrence rates vary by how well the tumor was removed and its grade. Benign meningiomas recur less often, while malignant ones recur more.
What factors increase the risk of meningioma recurrence?
Factors that increase recurrence risk include incomplete removal, higher tumor grade, and certain molecular markers. Aggressive surgery and adjuvant therapies can reduce recurrence risk.
What is the quality of life for meningioma patients after treatment?
Quality of life for meningioma patients varies. It depends on the tumor, treatment, and individual factors. Many patients regain normal activities and have good functional outcomes.
How do neurological and cognitive outcomes vary after meningioma treatment?
Outcomes vary by tumor location, treatment, and individual factors. Good care and rehabilitation can improve outcomes.
What is the psychological impact of meningioma diagnosis and treatment?
Diagnosis and treatment can deeply affect patients psychologically. Support from healthcare, family, and support groups is key to addressing these challenges.
References
National Center for Biotechnology Information (NCBI). Regional Variability in Survival for Patients Diagnosed with Selected Central Nervous System Tumours in Canada. https://www.ncbi.nlm.nih.gov/books/NBK560538/