
Recovering from a coma after a severe head injury is complex and unpredictable.
At Liv Hospital, our teams use advanced tools like the Glasgow Coma Scale (GCS) and the Disorder of Consciousness Scale (DOCS) to check patient progress.
The odds of waking up depend on many things. This includes how bad the brain hemorrhage was and the patient’s health.
Knowing these factors is key for those dealing with coma recovery.
Key Takeaways
- Recovery from a coma is influenced by multiple factors, including the severity of the initial injury.
- The Glasgow Coma Scale (GCS) and Disorder of Consciousness Scale (DOCS) are used to assess patient outcomes.
- Brain hemorrhage is a significant complication that affects coma recovery.
- Patient overall health plays a critical role in determining the chances of awakening.
- Liv Hospital’s expert teams provide compassionate support and cutting-edge care for patients and families.
The Science Behind Traumatic Brain Injuries and Consciousness

Head trauma’s effect on brain function is a key area of study, mainly when it causes coma. Traumatic brain injuries (TBI) happen from a violent blow or jolt to the head or body. This can change how the brain works or its structure. We’ll look at how head trauma impacts brain function and the various types of TBI.
How Head Trauma Affects Brain Function
Head trauma can severely damage brain cells and disrupt normal brain function. When the brain is injured, it can start a chain of events leading to coma or other consciousness disorders. The injury’s severity and location are key in determining the outcome.
Primary brain damage happens right at the injury, while secondary brain damage can develop over time. This can be due to swelling, bleeding, or infection. Knowing these mechanisms is vital for understanding recovery chances.
Different Types of Traumatic Brain Injuries
Traumatic brain injuries can be categorized based on the injury’s nature and severity.
Closed Head Injuries
Closed head injuries don’t break the skull. They happen when the brain hits the skull’s inside due to a violent blow or jolt. Concussions are a type of closed head injury. They can cause immediate symptoms like confusion and disorientation.
Penetrating Head Injuries
Penetrating head injuries involve an object entering the brain, damaging specific areas. These injuries are usually more severe. They carry a higher risk of complications like infection and long-term cognitive issues.
Knowing the type and severity of TBI is key for the right treatment and recovery chances from coma. We’ll dive deeper into coma and brain injury complexities in the next sections.
Understanding Coma from Head Trauma
Coma from head trauma is complex. It involves how the brain works and the effects of severe injury. We’ll look at what coma is, how it’s classified, and how it differs from other consciousness disorders.
Definition and Classification of Coma States
A coma is a deep sleep-like state that lasts a long time. People in a coma don’t respond to their surroundings. Knowing the type of coma helps doctors plan the best care.
The Glasgow Coma Scale (GCS) is used to measure coma severity. It checks how well a person can talk, move, and open their eyes. Scores range from 3 to 15, with lower scores showing more severe injuries.
Distinguishing Coma from Other Consciousness Disorders
It’s important to tell coma apart from other states like vegetative or minimally conscious states. Each state has its own care needs and outlook.
Vegetative State vs. Minimally Conscious State
A vegetative state means a person is awake but not aware. They might open their eyes and show reflexes but don’t think or understand. A minimally conscious state is when a person shows some awareness, like reacting to their environment.
To understand the differences, let’s look at a table:
| Characteristics | Coma | Vegetative State | Minimally Conscious State |
|---|---|---|---|
| Eye Opening | No | Yes | Yes |
| Awareness | No | No | Minimal |
| Response to Stimuli | No | Reflexive | Purposeful |
| Prognosis | Variable | Poor to Fair | Fair to Good |
Knowing the differences is key to helping patients with consciousness disorders. Accurate diagnosis and classification help doctors plan better care and give families a clearer picture of what to expect.
Assessment Tools for Predicting Recovery
Predicting recovery in coma patients is a complex task. We use various scales to evaluate their condition and recovery chances. These scales help us understand how well a patient might do after a coma from head trauma.
The Glasgow Coma Scale (GCS) Explained
The Glasgow Coma Scale is a tool to measure a person’s consciousness. It looks at three main areas: eye opening, verbal response, and motor response. This scale helps doctors assess a patient’s state of mind.
Scoring System and Interpretation
The GCS scores range from 3 to 15, with higher scores showing better brain function. Scores are divided into three levels: severe (3-8), moderate (9-12), and mild (13-15) brain injury. A lower score means a more severe brain injury and a worse prognosis.
| GCS Score | Category | Prognosis |
|---|---|---|
| 3-8 | Severe | Poor |
| 9-12 | Moderate | Variable |
| 13-15 | Mild | Good |
The Disorder of Consciousness Scale (DOCS)
The Disorder of Consciousness Scale is for patients with disorders of consciousness, like coma. It checks if patients can follow commands and react to stimuli.
Improving Prediction Accuracy Over Time
The DOCS helps predict recovery better over time. By checking changes in a patient’s condition, we get insights into their recovery path. This lets healthcare providers adjust treatment plans to meet the patient’s needs.
Both the GCS and DOCS are key in assessing coma patients and predicting their recovery. By using these scales and other clinical tools, we can give a more accurate prognosis. This helps us develop effective treatment plans for patients.
Statistical Outlook for Coma Recovery
We look into the stats on coma recovery. This includes survival rates and how well patients can get better. These numbers help doctors and families know what to expect when someone is in a coma from head trauma.
Survival Rates for Severe Traumatic Brain Injury
People with severe brain injuries have different chances of getting better. Some make big strides, while others may stay in a coma or have a tough time. Thanks to better medical care, more people with severe TBI are surviving.
Survival Rate Statistics:
| Time Frame | Survival Rate |
|---|---|
| 1 Year | 60-70% |
| 5 Years | 40-50% |
| 10 Years | 30-40% |
Short-term Recovery Statistics (First Two Weeks)
The first two weeks after a coma are very important. Doctors watch closely for any signs of getting better or worse. Early signs of recovery might include better scores on the Glasgow Coma Scale or certain brain signals.
Patients who show signs of getting better early on usually do better in the long run. But, how much they get better can vary a lot.
Long-term Recovery Prospects (One Year and Beyond)
How well coma patients recover long-term depends on many things. These include how bad the injury was, if there were any complications, and the patient’s overall health. Some patients make big progress in the first year, while others keep getting better over years.
Studies show that recovery slows down after the first year. But, with the right rehab, patients can keep getting better. Specialized rehab programs play a big role in helping patients recover fully.
Knowing the stats on coma recovery helps doctors and families understand the journey ahead. By looking at survival rates, early recovery signs, and long-term prospects, we can better support patients and their families.
Factors Influencing Recovery Chances
Knowing what affects coma recovery is key for patients and their families. The path to getting better from a coma is complex. It depends on many things, like the patient and the injury.
Patient-Specific Factors
Things about the patient can greatly affect recovery from a coma. These are personal traits that can influence how well someone heals and responds to treatment.
Age and Pre-existing Health Conditions
Age matters a lot, as older people often face tougher recovery paths. Pre-existing health conditions, like diabetes or heart disease, can make recovery harder. They weaken the body’s healing power.
Genetic and Biological Factors
Genetic predispositions and biological factors also play a role. Studies show that genes can affect how the brain heals after an injury.
Injury-Specific Factors
The type and severity of the head trauma are key to recovery chances. Knowing these details helps doctors give better predictions.
Severity and Location of Brain Damage
The severity and location of brain damage are very important. More serious injuries or those in critical areas usually have worse outcomes.
Duration of Unconsciousness
The duration of unconsciousness is also a big factor. The longer someone is in a coma, the less likely they are to fully recover.
Understanding these factors helps doctors give more tailored care. This can improve recovery chances for patients and their families.
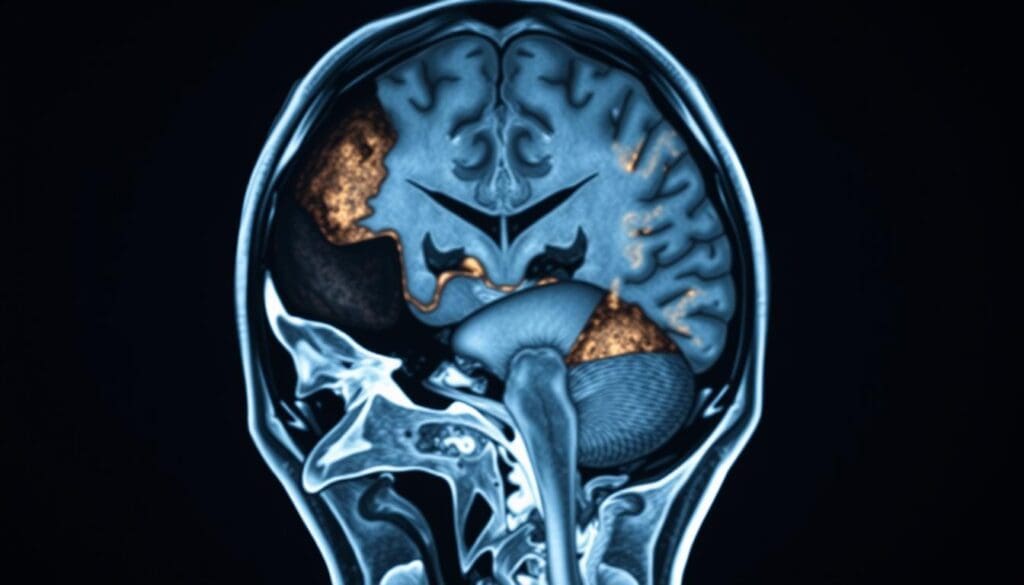
Brain Hemorrhage Complications in Coma Recovery
Brain hemorrhage is a serious issue that can happen after head trauma. It makes recovery from coma harder. When someone gets head trauma, they are more likely to get a brain hemorrhage. This makes their future look uncertain.
Types of Intracranial Bleeding
Intracranial bleeding, or hemorrhage, can happen in different ways. Each type affects coma recovery differently. Knowing about these types helps doctors choose the right treatment.
Subdural vs. Epidural Hematomas
Subdural and epidural hematomas are two kinds of bleeding. Subdural hematomas happen under the dura mater, a brain protector. Epidural hematomas happen between the dura mater and the skull. Both can raise pressure inside the skull, making coma recovery harder.
Intracerebral hemorrhage is bleeding right into the brain. It can damage brain cells and structures. This affects brain functions and makes coma recovery more challenging.
How Bleeding Location and Extent Affect Prognosis
The place and size of bleeding are key in coma patient outcomes. How severe the bleeding is and where it is in the brain matters a lot. It affects how well a patient can recover.
Patients with bleeding in important brain areas might have a tougher time. Those with bleeding in less critical spots might have a better chance. Also, bigger bleeds usually mean a worse outcome.
Doctors use this knowledge to make treatment plans that fit each patient. This helps improve recovery chances.
The Critical Timeline of Coma from Head Trauma
Recovering from a coma due to head trauma takes a long time and varies for everyone. Doctors know that the road to getting better is complex. It depends on how bad the injury was and the patient’s health.
The First 72 Hours After Injury
The first 72 hours after a head injury are very important. Doctors watch the patient closely to see if they’re getting better or worse. They use the Glasgow Coma Scale (GCS) to check how awake the patient is and guess how they might do.
It’s key to act fast. The medical team works hard to keep the patient stable, control brain pressure, and stop more damage.
Weeks 1-4: Early Recovery Indicators
After the first 72 hours, weeks 1-4 are key for seeing if the patient is getting better. Some might start to wake up, respond to voices, or move on their own.
Rehabilitation efforts start here. A team of experts works together to help the patient get back what they lost and live better.
Months 1-12: Continued Recovery Potencial
The first year after the injury is a time of big chances for getting better. Patients can make big strides in their brain function and might even become more independent.
Keeping up with rehabilitation therapy is key. This includes physical, occupational, and speech therapy. It helps the patient reach their full recovery.
Beyond One Year: Late Recoveries
Even after a year, some people can keep getting better. The pace might slow down, but with more therapy, they can keep improving.
It’s important for families and caregivers to stay hopeful but also realistic. They should be open to the chance of more progress.
Signs of Emerging Consciousness
Recovering from a coma is a complex journey. It shows through physical and neurological signs. We’ll look at these signs, like physical recovery, neurological markers, and reflexive vs. purposeful movements.
Physical Indicators of Recovery
Physical signs are key in checking if coma patients are getting better. A big sign is moving from reflexive to purposeful actions.
Reflexive vs. Purposeful Movements
At first, patients might just react to things without thinking. For example, they might pull their hand back when it’s pinched. But as they get better, they start doing things on purpose, like reaching for something or answering when spoken to.
Doctors watch for these changes closely. A patient might start by reacting to pain, then to touch, and eventually to commands.
Neurological Markers of Improvement
Neurological signs are very important for tracking recovery. They include changes in brain activity, better thinking skills, and the return of reflexes.
One important sign is a better score on the Glasgow Coma Scale (GCS). The GCS checks how well a patient can open their eyes, talk, and move. It shows how awake and aware they are.
| Neurological Marker | Description | Significance |
|---|---|---|
| Glasgow Coma Scale (GCS) | Assesses eye-opening, verbal, and motor responses | Improvement indicates emerging consciousness |
| Brain Activity | Changes in EEG or other brain activity measures | Reflects recovery of brain function |
| Cognitive Function | Improvement in attention, memory, and other cognitive domains | Indicates return of higher brain functions |
Common Misinterpreted Signs
It’s important for caregivers and doctors to know about signs that might look like recovery but aren’t. For example, some patients might act agitated or restless. This could be mistaken for getting better, but it could also mean they’re in pain or uncomfortable.
It’s vital to tell the difference between real signs of getting better and other behaviors. Understanding the patient’s situation and watching them closely helps.
By knowing the signs of getting better, doctors can make treatment plans that really help patients recover.
Modern Treatment Approaches and Rehabilitation
Medical technology has changed how we treat coma patients, giving them new hope. We now better understand brain injuries and have effective treatments.
Acute Medical Interventions
Right after a head trauma, doctors focus on keeping the patient stable. They might do surgery to ease brain pressure, stop bleeding, or fix blood vessels. They also use medicines to control seizures, reduce swelling, and keep blood and oxygen levels right.
Specialized Rehabilitation Programs
When the patient is stable, special rehab programs start. These programs are made just for the patient. They might include physical, occupational, speech, and cognitive therapy. The goal is to help patients get back lost skills and adjust to changes.
- Physical therapy works on moving better, being stronger, and more coordinated.
- Occupational therapy helps with daily tasks and being independent.
- Speech therapy deals with talking and understanding.
- Cognitive rehabilitation focuses on memory, attention, and solving problems.
Emerging Therapies and Clinical Trials
New treatments and trials are always coming up in coma recovery. Two big areas are neurostimulation and new medicines.
Neurostimulation Techniques
Techniques like TMS and tDCS might help by making brain activity better. These methods are safe and can help with thinking and moving better.
Pharmacological Approaches
New medicines are being looked at to help coma recovery. Some drugs might help with symptoms, wakefulness, or brain healing. Research is ongoing to see if these medicines work well.
As we learn more about coma and brain injuries, we’ll find even better treatments. By using the latest medical care and rehab, coma patients have a good chance of getting better.
Conclusion: Navigating the Uncertainty of Coma Recovery
Coma recovery is a tough journey for patients, families, and doctors. We’ve looked into coma from head trauma, including what affects outcomes and treatment options. This includes the severity of the injury and the patient’s health.
The path to recovery from coma is full of unknowns. Many things can influence it, like the injury’s severity and the patient’s health. Knowing these factors helps doctors and families make better care choices.
Even though coma recovery is hard, there’s hope for better results. With advanced care and a team effort, patients can face the challenges of recovery. This way, they can get the best possible outcome.
What are the chances of waking up from a coma caused by head trauma?
Waking up from a coma caused by head trauma is not guaranteed. It depends on the injury’s severity, any complications like brain hemorrhage, and the patient’s health.
How does head trauma affect brain function and lead to coma?
Head trauma can damage brain areas that control consciousness. This damage can lead to coma.
What is the difference between coma, vegetative state, and minimally conscious state?
Coma is a deep unconsciousness. Vegetative state means patients are awake but not aware. Minimally conscious state shows some awareness.
How do assessment tools like the Glasgow Coma Scale (GCS) and Disorder of Consciousness Scale (DOCS) help predict patient outcomes?
The GCS and DOCS assess consciousness levels. They help predict recovery chances by looking at neurological responses.
What are the survival rates for severe traumatic brain injury?
Survival rates for severe TBI vary. They depend on injury severity and overall health. Mortality rates are high in the first two weeks.
How do patient-specific factors influence recovery chances from a coma?
Factors like age and health conditions before the coma can affect recovery chances.
What is the impact of brain hemorrhage on coma recovery?
Brain hemorrhage complicates coma recovery. The location and extent of bleeding affect the prognosis.
What are the signs of emerging consciousness in coma patients?
Signs include purposeful movements and neurological improvement. These may indicate recovery.
Is coughing in a coma a good sign?
Coughing in a coma suggests neurological improvement. It shows some brainstem function.
What are the modern treatment approaches for coma patients?
Modern treatments include acute medical care, rehabilitation, and new therapies. These include neurostimulation and pharmacological approaches.
Can someone wake up from a coma after a long time?
Yes, some patients wake up after a long time. Late recoveries beyond one year are possible.
How long does it take to regain consciousness after brain surgery?
Regaining consciousness after brain surgery varies. It depends on surgery type, patient health, and complications.
References
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC4771229/
- PubMed/NCBI : https://pubmed.ncbi.nlm.nih.gov/7242878/
- Harvard Medical School (Recovery May Take Time) : https://hms.harvard.edu/news/recovery-may-take-time
- Palliative Care Now (Prognostication in Severe Traumatic Brain Injury in Adults) : https://www.mypcnow.org/fast-fact/prognostication-in-severe-traumatic-brain-injury-in-adults/
- JAMA Neurology : https://jamanetwork.com/journals/jamaneurology/fullarticle/2781523
- Centers for Disease Control and Prevention (CDC) (Moderate to Severe TBI Lifelong Effects) : https://www.cdc.gov/traumaticbraininjury/pdf/moderate_to_severe_tbi_lifelong-a.pdf



































