Last Updated on November 20, 2025 by Ugurkan Demir

At Liv Hospital, we understand the complexities of sickle cell disease and its potentially life-threatening complications. A vaso-occlusive crisis is a hallmark of this condition, characterized by severe pain and organ dysfunction.
Understanding the various aspects of sickle cell crisis is key for effective management. Our expert care team is dedicated to providing advanced guidance and support for those facing these challenges. In this article, we will cover the key facts about vaso-occlusive crisis, its types, and the management strategies employed by our medical professionals.
Key Takeaways
- Understanding the definition and types of sickle cell crisis
- The importance of prompt medical attention for vaso-occlusive crises
- Overview of management strategies for sickle cell disease
- The role of expert care in improving patient outcomes
- Liv Hospital’s approach to patient-centered care for sickle cell disease
What Is Sickle Cell Crisis: The Hallmark Complication of Sickle Cell Disease
A sickle cell crisis is a serious problem linked to sickle cell disease. It causes severe pain and can harm organs. It happens when sickle-shaped red blood cells block blood vessels, leading to pain and tissue damage. Knowing about sickle cell crisis is key to helping patients manage their condition better.
Definition and Basic Mechanism
Sickle cell crisis, also known as vaso-occlusive crisis, happens when sickle-shaped red blood cells block small blood vessels. This blockage causes tissue ischemia, leading to severe pain and can harm vital organs. The crisis is caused by hemoglobin S changing shape in low oxygen conditions.
The process involves several key steps:
- Deoxygenation of hemoglobin S
- Polymerization of hemoglobin S
- Red blood cell sickling
- Adhesion to endothelial cells
- Vascular occlusion
Impact on Patient Quality of Life
The effects of sickle cell crisis on a patient’s life are huge. The pain and risk of organ damage hurt both body and mind. Patients often feel anxious and depressed because they never know when a crisis will happen.
| Aspect of Life | Impact of Sickle Cell Crisis |
| Physical Health | Severe pain, organ damage, increased risk of infections |
| Emotional Well-being | Anxiety, depression, stress related to crisis unpredictability |
| Social Life | Frequent hospitalizations, missed work or school days |
It’s important to find ways to manage sickle cell disease well. This can help improve a patient’s life quality a lot.
Key Fact #1: The Pathophysiology of Sickle Cell Crisis
Understanding sickle cell crisis is key to managing it well. It involves many factors that lead to the crisis.
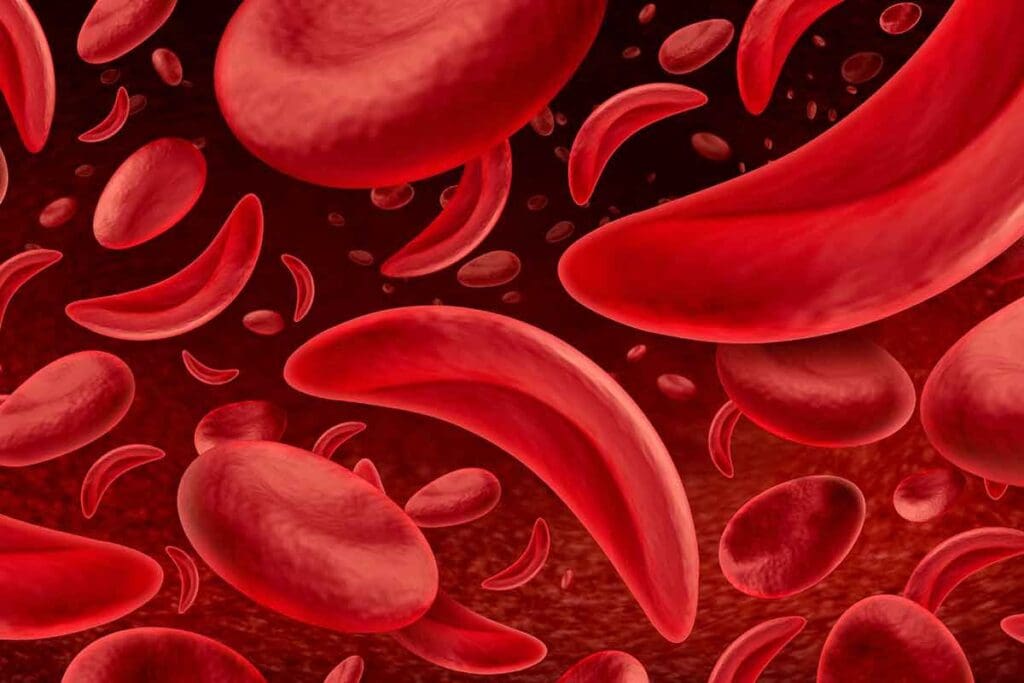
Hemoglobin S Polymerization Process
The main cause of sickle cell crisis is the polymerization of hemoglobin S (HbS) in red blood cells. This happens when there’s not enough oxygen. It causes HbS to form fibers, changing the shape of the red blood cells into a sickle shape.
Polymerization of HbS makes red blood cells more rigid and prone to breaking down. This process is reversible at first but becomes permanent as the cells go through cycles of sickling and unsickling.
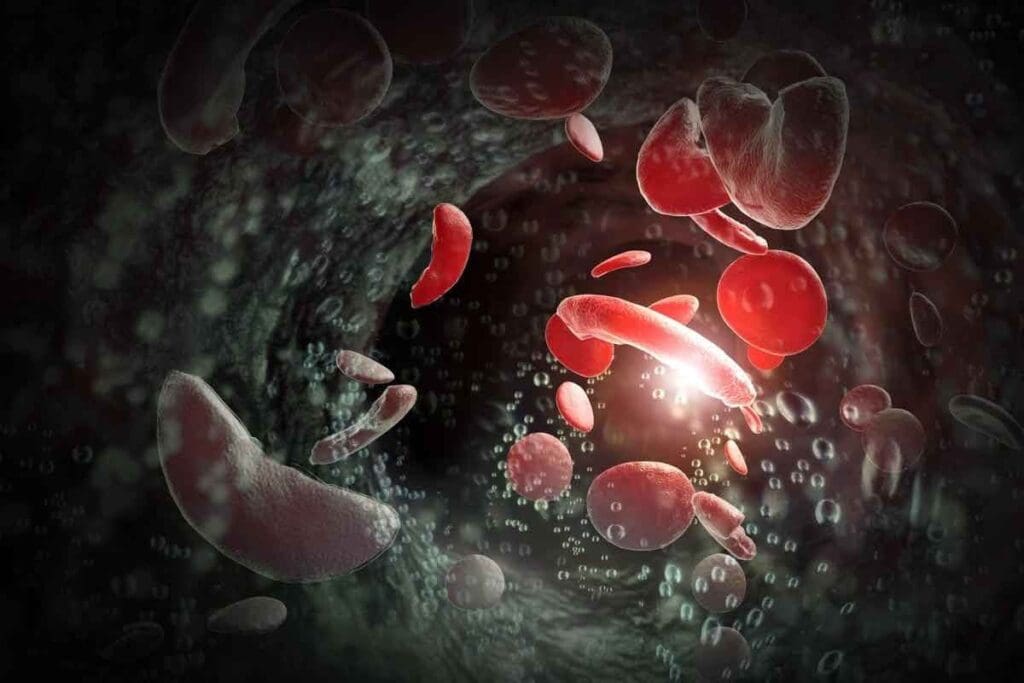
Endothelial Dysfunction and Inflammation
Endothelial dysfunction is a big part of sickle cell crisis. Sickled red blood cells stick to the blood vessel walls. This causes inflammation and starts many cellular and molecular pathways.
This sticking and inflammation lead to the release of pro-inflammatory cytokines. The interaction between sickled red blood cells and endothelial cells is a major factor in vaso-occlusive crises.
Microvascular Occlusion Development
The final step in sickle cell crisis is microvascular occlusion. Sickled red blood cells block small blood vessels. This causes tissue ischemia and pain.
The blockage of blood flow leads to the buildup of metabolic byproducts. This makes the crisis worse. Knowing this is key to finding new treatments.
| Pathophysiological Mechanism | Description | Clinical Impact |
| Hemoglobin S Polymerization | Aggregation of HbS under low oxygen conditions | Sickling of red blood cells, hemolysis |
| Endothelial Dysfunction | Adhesion of sickled RBCs to endothelial cells, inflammation | Vaso-occlusion, pain crises |
| Microvascular Occlusion | Obstruction of small blood vessels by sickled RBCs | Tissue ischemia, organ damage |
Key Fact #2: Vaso-Occlusive Crisis Accounts for Most Sickle Cell Emergencies
Sickle cell emergencies mostly come from vaso-occlusive crises. These crises need quick medical help. They are a big problem for people with sickle cell disease, causing a lot of pain and affecting their life quality.
Mechanism of Vascular Obstruction
Vaso-occlusive crisis happens when small blood vessels get blocked by sickled red blood cells. This blockage causes pain and tissue damage. It’s a complex issue involving sickled red blood cells, endothelial cells, and inflammatory mediators.
Key factors contributing to vascular obstruction include the abnormal adhesion of sickled red blood cells to the endothelium, increased blood viscosity, and the release of pro-inflammatory cytokines.
Progression from Acute to Chronic Pain
Acute vaso-occlusive episodes can turn into chronic pain. This is because of repeated tissue ischemia and inflammation. Managing chronic pain is hard and needs a detailed plan. This includes medicines, physical therapy, and support for the mind.
Experts say,
“Chronic pain in sickle cell disease is a complex condition that requires a multifaceted treatment plan to address the physical, emotional, and social aspects of pain.”
Key Fact #3: Different Types of Sickle Cell Crisis Affect Various Organs
Sickle cell crisis isn’t just one thing. It’s several types that affect different parts of the body. This makes managing sickle cell disease very complex.
Acute Chest Syndrome
Acute chest syndrome (ACS) is a big problem for people with sickle cell disease. It causes new lung problems, fever, and breathing issues. It can happen for many reasons, like infections or lung damage.
Experts say ACS is a medical emergency. It needs quick diagnosis and treatment.
Doctors treat ACS with oxygen, pain relief, and antibiotics. Sometimes, they need to give blood to help the red blood cells.
Splenic Sequestration Crisis
Splenic sequestration crisis happens when red blood cells get stuck in the spleen. This makes the spleen big and can be very dangerous. It’s more common in kids and can cause severe anemia.
Medical Expert, a hematologist, says, “We must quickly treat splenic sequestration crisis to avoid serious problems.” Treatment includes fluids and sometimes blood transfusions.
Aplastic Crisis
Aplastic crisis is when the body stops making new red blood cells. It’s often caused by a virus. This leads to severe anemia, which is very dangerous for people with sickle cell disease.
“Aplastic crisis in sickle cell disease patients requires immediate medical attention to prevent serious complications,” according to a study published in a leading medical journal.
Doctors treat aplastic crisis with blood transfusions. This helps until the bone marrow starts making red blood cells again.
In conclusion, knowing about the different sickle cell crises is key to good care. By understanding each crisis, doctors can better help their patients.
Key Fact #4: Common Triggers of Sickle Cell Crisis
Knowing what triggers sickle cell crisis is key to managing it. This condition can be caused by many things. By knowing these triggers, doctors and patients can prevent or lessen these episodes.
Environmental Factors and Temperature Changes
Environmental factors are big in triggering sickle cell crises. Temperature extremes can start a crisis. Both hot and cold can cause dehydration and affect blood vessels.
We suggest avoiding extreme temperatures. Keeping a comfortable environment can help prevent crises.
Dehydration and Physical Exertion
Dehydration is a major trigger for sickle cell crisis. Losing too much fluid makes sickled red blood cells more likely to block blood vessels. Adequate hydration is vital.
Drinking lots of fluids, even in hot weather or when active, is important. Strenuous or long physical activities can also cause a crisis by increasing oxygen demand and possibly causing dehydration.
Infections and Illness
Infections and illnesses are big triggers for sickle cell crisis. Fighting off an infection can cause inflammation and increase sickling risk. We stress the need for preventive measures like vaccinations and quick treatment of infections.
Patients with sickle cell disease should watch their health closely. They should seek medical help at the first sign of infection or illness.
Understanding and managing these common triggers helps patients and doctors. Together, they can reduce the number and severity of sickle cell crises. This improves the quality of life for those with sickle cell disease.
Recognizing Sickle Cell Crisis: Signs and Symptoms
It’s important to know the signs of a sickle cell crisis to get help quickly. We need to understand the symptoms of this complex condition.
Pain Characteristics and Patterns
Pain is the main symptom of a vaso-occlusive crisis. This pain is often severe and unpredictable, needing fast medical care. The pain can feel sharp or dull, varying from person to person.
The pain can also show up in different ways. Sometimes, it’s in one area like the chest or belly. Other times, it affects more areas of the body. Knowing these patterns helps doctors treat the crisis better.
Organ-Specific Manifestations
Sickle cell crisis can harm different organs, causing various symptoms. For example, acute chest syndrome is a serious issue with chest pain, cough, and trouble breathing. Another problem is splenic sequestration crisis, where red blood cells pile up in the spleen, causing severe anemia.
Other issues include priapism, a long-lasting erection of the penis, and hepatic sequestration, where red blood cells gather in the liver. Spotting these symptoms is key to giving the right care and avoiding lasting harm.
By knowing the signs and symptoms of a sickle cell crisis, we can help patients live better lives. This includes understanding the pain and how it affects different organs.
Key Fact #5: Diagnostic Approach to Sickle Cell Crisis
Diagnosing sickle cell crisis requires a detailed approach. It uses lab tests and imaging studies. This method is key to understanding the crisis’s type and severity. It helps doctors make the right treatment plans and improve patient care.
Essential Sickle Cell Crisis Labs
Labs are essential in managing sickle cell crisis. They include:
- Complete Blood Count (CBC): Shows hemoglobin levels, white blood cell count, and platelet count. It helps spot anemia, infections, or other issues.
- Reticulocyte Count: Counts young red blood cells. It shows how the bone marrow is responding to anemia.
- Blood Chemistry Tests: Checks liver and kidney function. These organs can be affected during a crisis.
- Arterial Blood Gas (ABG): Checks oxygen levels. It helps identify acute chest syndrome.
A leading hematologist says, “Lab tests are key in diagnosing and managing sickle cell crisis. They give important info on the patient’s condition and guide treatment.”
Imaging Studies in Crisis Evaluation
Imaging studies are also vital in evaluating sickle cell crisis complications. Key imaging methods include:
- Chest X-ray: Helps spot acute chest syndrome, a serious complication.
- Abdominal Ultrasound: Finds splenic sequestration or other abdominal issues.
- MRI: Checks for stroke or neurological problems in sickle cell disease patients.
Recent guidelines suggest using imaging studies wisely. They help evaluate specific complications and guide management in sickle cell crisis.
By combining lab tests and imaging, healthcare providers get a full picture of the patient’s condition. This allows for targeted and effective management of sickle cell crisis.
Key Fact #6: Sickle Cell Crisis Management Strategies
Managing sickle cell crisis needs a detailed plan. It focuses on acute pain, staying hydrated, and fighting infections. A team effort among healthcare, patients, and families is key. This helps ease symptoms, prevent worse problems, and better outcomes.
Acute Pain Management Protocols
Handling acute pain is vital in sickle cell crisis care. We use a mix of methods to manage pain. This includes:
- Administering analgesics, such as opioids and nonsteroidal anti-inflammatory drugs (NSAIDs)
- Utilizing patient-controlled analgesia (PCA) for severe pain
- Implementing non-pharmacological interventions, such as heat or cold therapy, relaxation techniques, and distraction methods
A study compared pain management in sickle cell patients. Here’s a summary:
| Management Strategy | Average Pain Reduction | Patient Satisfaction Rate |
| Opioid Therapy | 60% | 85% |
| PCA Therapy | 70% | 90% |
| Non-Pharmacological Interventions | 40% | 80% |
Hydration and Oxygen Therapy
Hydration and oxygen therapy are key in managing sickle cell crisis. We suggest:
- Aggressive hydration with intravenous fluids to prevent dehydration and improve blood flow
- Oxygen therapy to increase oxygen saturation and reduce tissue hypoxia
Addressing Infections and Complications
Infections and complications often happen during a sickle cell crisis. We stress the need to:
- Promptly identify and treat infections with antibiotics
- Watch for signs of complications, like acute chest syndrome or splenic sequestration
- Use preventive measures, such as vaccinations and prophylactic antibiotics
By using a full management plan, we can help patients get better. This also lowers the chance of serious problems from sickle cell crisis.
Emerging Treatments and Research Directions
Sickle cell disease management is getting a boost from new research and treatments. We’re learning more about this condition every day. This knowledge is leading to new ways to help patients.
Novel Pharmacological Approaches
New drugs are being developed to tackle sickle cell disease. These drugs target specific problems caused by the disease. They include:
- Anti-adhesion molecules to reduce vaso-occlusion
- Hemoglobin F inducers to decrease disease severity
- Anti-inflammatory agents to manage chronic inflammation
These new drugs aim to lessen the impact of sickle cell crises. This could greatly improve patients’ lives.
Gene Therapy and Curative Options
Gene therapy is a big hope for sickle cell disease treatment. It could offer a cure by fixing the faulty gene. This could lead to normal hemoglobin production again.
| Therapy Type | Description | Potential Benefits |
| Gene editing | Precise modification of the HBB gene | Potential cure by correcting the genetic defect |
| Lentiviral vector-based gene therapy | Introduction of a healthy HBB gene into patient cells | Restoration of normal hemoglobin production |
These new treatments are very promising. But, we need more research to know how well they work and if they’re safe.
As research keeps moving forward, we’ll see better treatments for sickle cell disease. This will help patients live better lives.
Key Fact #7: Preventing Acute Vaso-Occlusive Crisis
We can lower the risk of vaso-occlusive crisis with lifestyle changes and medical help. It’s key to improve life for those with sickle cell disease.
Lifestyle Modifications and Self-Care Strategies
Making lifestyle changes is important to prevent vaso-occlusive crises. Staying hydrated is key, as dehydration can cause a crisis. Drinking lots of water is recommended.
Avoiding extreme temperatures and eating well also helps manage the condition. Regular exercise is good, but don’t overdo it. Gentle activities like walking or yoga are best. Getting enough sleep and using stress-reduction techniques like meditation can also help.
Preventive Medications and Vaccinations
Some medicines and vaccines can also prevent vaso-occlusive crises. Hydroxyurea is a common drug that can reduce crisis frequency and other complications.
Vaccines are vital for sickle cell disease patients to avoid infections that can lead to a crisis. Make sure to get all recommended vaccines, like pneumococcal, influenza, and meningococcal.
By using these preventive steps, people with sickle cell disease can lower their crisis risk. This improves their life quality greatly.
Epidemiology of Sickle Cell Crisis in the United States
Understanding sickle cell disease is key to tackling its big healthcare challenge in the U.S. It hits certain groups harder, affecting healthcare use and the economy.
Prevalence Among Different Populations
Sickle cell disease hits some groups more than others. African Americans are hit hard, with about 1 in 365 having the disease. Hispanic Americans, like those from Puerto Rico and the Dominican Republic, also see more cases. It’s less common among non-Hispanic whites.
There’s also a notable sickle cell trait prevalence. About 1 in 12 African Americans carry it. Knowing these numbers helps in planning public health efforts.
Healthcare Utilization and Economic Impact
Sickle cell disease leads to a lot of healthcare use. This includes many hospital visits for crises and other issues. The cost is high, affecting emergency visits, hospital stays, and ongoing care.
A study showed the yearly healthcare cost per patient is very high. This adds up to a big economic burden on healthcare systems.
To lessen these effects, we need better management and prevention. This means better care access, patient education, and new treatments. These steps can help reduce crisis frequency and severity.
Conclusion: Living with Sickle Cell Disease and Managing Crises
Living with sickle cell disease means you need a full plan to handle crises well. Sickle cell crisis is a big problem that affects your life a lot. It causes chronic hemolytic anemia, organ damage, and vaso-occlusive crises (VOCs).
Studies show patients often have many VOCs, with an average of 5.3 episodes in 12 months. This is found in a study on PubMed Central.
Managing crises is not just about treating the acute episodes. It also means taking steps to prevent them and making lifestyle changes. Fatigue, depression, and anxiety are common issues for patients. This shows the need for care that looks at both physical and emotional health.
Improving quality of life is a main goal for many patients. By understanding the disease, recognizing symptoms, and using good management strategies, healthcare providers can make a big difference. We need to keep working on research and treatments to better care for those with sickle cell disease.
FAQ
What is a sickle cell crisis?
A sickle cell crisis is a painful episode for those with sickle cell disease. It happens when sickled red blood cells block blood vessels.
What are the different types of sickle cell crisis?
There are several types of sickle cell crisis. These include vaso-occlusive crisis, acute chest syndrome, splenic sequestration crisis, and aplastic crisis. Each affects different organs and has its own clinical implications.
What triggers a sickle cell crisis?
Several things can trigger a sickle cell crisis. These include environmental factors, dehydration, physical exertion, and infections. Managing or avoiding these can help reduce the risk of a crisis.
How is sickle cell crisis diagnosed?
Diagnosing sickle cell crisis involves several tests. These include a complete blood count and reticulocyte count. Imaging studies are also used to evaluate the crisis and its complications.
What is the management strategy for sickle cell crisis?
Managing sickle cell crisis includes several steps. These include acute pain management, hydration, and oxygen therapy. It also involves addressing infections and complications to provide full care to patients.
Can sickle cell crisis be prevented?
Yes, preventing acute vaso-occlusive crisis is possible. It involves lifestyle changes, self-care, and preventive medications and vaccinations. These can help reduce the risk of a crisis.
What are the emerging treatments for sickle cell disease?
New treatments for sickle cell disease are being developed. These include novel pharmacological approaches and gene therapy. They offer hope for better patient outcomes and a possible cure.
How does sickle cell crisis affect patient quality of life?
Sickle cell crisis has a big impact on patient quality of life. It causes physical and emotional challenges. Patients need full care and support to manage these issues.
What is the significance of understanding the pathophysiology of sickle cell crisis?
Understanding sickle cell crisis is key to better management. It helps in developing effective strategies and improving patient outcomes.
How common is sickle cell crisis in the United States?
Sickle cell crisis is common in certain groups in the United States. It leads to a lot of healthcare use and economic impact.
References
- Centers for Disease Control and Prevention. (2024). Data & statistics on sickle cell disease and vaso-occlusive crises. https://www.cdc.gov/sickle-cell/data/index.html
- Kato, G. J., Piel, F. B., Reid, C., et al. (2018). Sickle cell disease. Nature Reviews Disease Primers, 4, 18010. https://www.nature.com/articles/nrdp201810