Last Updated on November 27, 2025 by Bilal Hasdemir

Noticing vision changes or a bulging eye can be alarming, and understanding the potential link to meningioma brain tumors is crucial for your health decisions.
At Liv Hospital, we are committed to providing you with comprehensive information about these common yet complex tumors. Meningiomas are typically non-malignant brain tumors that can sometimes cause bulging eye symptoms when located near the optic nerve or within the orbit.
We understand the importance of being informed about your health, and we are here to guide you through the key facts about meningiomas.
Key Takeaways
- Meningiomas are the most common type of non-malignant brain tumors.
- They can cause bulging eye symptoms when located near the optic nerve or within the orbit.
- Understanding meningiomas is crucial for making informed health decisions.
- Liv Hospital provides comprehensive care and support for patients with meningiomas.
- Early diagnosis and treatment can significantly impact patient outcomes.
What Are Meningiomas? Definition and Basic Understanding

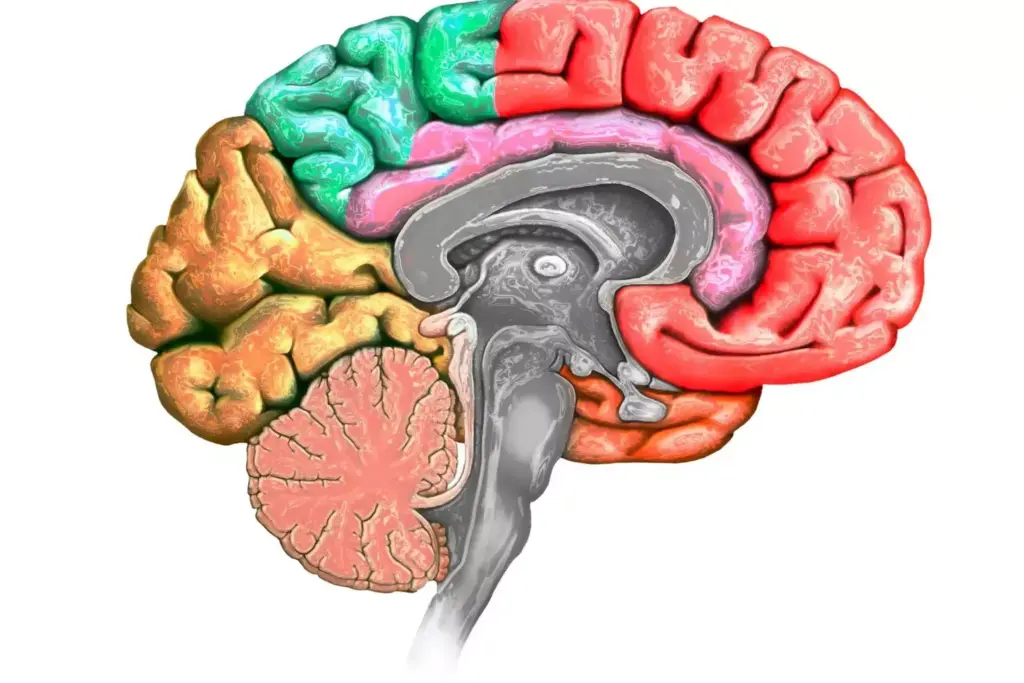
Meningiomas are a type of tumor that originates from the meninges, the protective membranes surrounding the brain and spinal cord. These tumors are typically benign, meaning they are non-cancerous, and their growth can vary significantly from one individual to another.
Origin and Development in the Meninges
The meninges are composed of three layers: the dura mater, arachnoid mater, and pia mater. Meningiomas most commonly arise from the arachnoid mater. The exact cause of meningioma development is not fully understood, but it is believed to involve genetic mutations that lead to uncontrolled cell growth in the meninges.
Types and Locations of Meningiomas
Meningiomas can occur in various locations around the brain and spinal cord. They are classified based on their location, size, and histological characteristics. The World Health Organization (WHO) grading system is used to classify meningiomas into three grades: Grade I (benign), Grade II (atypical), and Grade III (malignant).
Meningiomas can be found in different parts of the central nervous system, including:
- Cerebral convexity
- Skull base
- Spinal cord
- Orbital region
| Type of Meningioma | Location | Characteristics |
|---|---|---|
| Convexity Meningioma | Surface of the brain | Typically benign, slow-growing |
| Skull Base Meningioma | Base of the skull | Can be challenging to treat due to location |
| Spinal Meningioma | Spinal cord | Often benign, can cause spinal cord compression |
Understanding the different types and locations of meningiomas is crucial for determining the best course of treatment and management.
The Connection Between Bulging Eye Brain Tumor and Meningiomas
When meningiomas develop near or around the orbit, they can lead to noticeable changes in eye positioning and vision. These changes are often associated with orbital meningiomas, a type of meningioma that occurs near the eye socket.
How Orbital Meningiomas Cause Eye Protrusion
Orbital meningiomas can cause the eye to bulge or protrude, a condition known as proptosis or bulging eye brain tumor. This occurs when the tumor compresses or invades surrounding tissues, including the extraocular muscles and fat within the orbit. As the tumor grows, it can push the eyeball forward, leading to a noticeable bulge.
The symptoms associated with orbital meningiomas can vary depending on the tumor’s size and location. Common symptoms include:
- Protrusion or bulging of the eye
- Double vision or diplopia
- Vision loss or decreased visual acuity
- Eyelid swelling or retraction
- Limited eye movement
Visual Changes Associated with Meningiomas
In addition to causing the eye to bulge, orbital meningiomas can lead to various visual changes. These changes occur due to the tumor’s impact on the optic nerve and other critical visual structures. Patients may experience:
- Blurred vision
- Double vision
- Loss of peripheral vision
- Decreased visual acuity
Understanding the connection between meningioma symptoms and their effects on vision and eye appearance is crucial for patients and healthcare providers. Early diagnosis and appropriate treatment can significantly improve outcomes for individuals affected by these tumors.
Fact 1: Meningiomas Are Among the Most Common Brain Tumors
Meningiomas are a significant concern in neuro-oncology, and understanding their prevalence is crucial for both patients and healthcare providers. We will explore the statistical prevalence of meningiomas in the general population and examine the demographic patterns associated with these tumors.
Statistical Prevalence in the General Population
Meningiomas account for approximately one-third of all primary brain tumors, making them relatively common. Studies have shown that the incidence of meningiomas is increasing, likely due to improvements in diagnostic imaging techniques. According to various epidemiological studies, the annual incidence rate of meningiomas ranges from 4 to 7 per 100,000 people. To put this into perspective, here are some key statistics:
- The overall incidence of meningiomas is higher in women than in men.
- Meningiomas are more common in adults, with the majority diagnosed between the ages of 40 and 70.
- The incidence of meningiomas increases with age, peaking in the 7th and 8th decades of life.
Age, Gender, and Demographic Patterns
Demographic patterns play a crucial role in understanding the epidemiology of meningiomas. Research has identified several key demographic factors associated with an increased risk of developing meningiomas:
- Gender: Women are more likely to develop meningiomas than men, with a female-to-male ratio ranging from 2:1 to 3:1.
- Age: The incidence of meningiomas increases with age, with most cases diagnosed in middle-aged or older adults.
- Ethnicity: Some studies suggest that meningiomas may be more common in certain ethnic groups, although more research is needed to confirm these findings.
Understanding these demographic patterns can help healthcare providers identify individuals at higher risk and develop targeted screening strategies.
Fact 2: Most Meningiomas Are Non-Malignant
Most meningiomas are non-malignant, a characteristic that significantly influences patient prognosis and treatment options. Understanding the nature of these tumors is essential for patients to make informed decisions about their care.
Benign vs. Malignant Classification
Meningiomas are typically classified as benign, atypical, or malignant based on their characteristics and behavior. The majority, approximately 80-90%, are benign, meaning they are non-cancerous and usually grow slowly. Atypical meningiomas, which account for about 10-15%, may grow more quickly and have a higher chance of recurrence. Malignant meningiomas, though rare (about 1-3%), are cancerous and can invade surrounding brain tissue.
Understanding the classification of meningiomas is crucial because it directly impacts treatment decisions and patient outcomes. Benign meningiomas, while often monitored rather than immediately treated, can still cause symptoms due to their location and size.
WHO Grading System for Meningiomas
The World Health Organization (WHO) grading system is used to classify meningiomas based on their histological features. This system helps predict the tumor’s behavior and guides treatment decisions.
| WHO Grade | Meningioma Type | Characteristics |
|---|---|---|
| I | Benign | Slow-growing, non-cancerous |
| II | Atypical | More aggressive, higher recurrence risk |
| III | Malignant | Cancerous, invasive |
The WHO grading system provides a standardized way to assess meningiomas, helping clinicians and patients understand the prognosis and choose the most appropriate treatment strategy.
By understanding whether a meningioma is benign, atypical, or malignant, healthcare providers can tailor treatment plans to the individual patient’s needs, improving outcomes and quality of life.
Fact 3: Meningioma Symptoms Vary by Location and Size
Understanding the symptoms of meningiomas requires considering both the location and size of the tumor. Meningiomas, being tumors that arise from the meninges, the protective membranes surrounding the brain and spinal cord, can cause a wide range of symptoms depending on their location and dimensions.
Common Symptoms Across All Meningiomas
While the specific symptoms can vary, there are some commonalities across different meningiomas. Headaches are one of the most frequently reported symptoms, often resulting from the tumor pressing on the brain or causing a buildup of cerebrospinal fluid. Other common symptoms include seizures, visual disturbances, and weakness or numbness in the limbs. These symptoms occur because meningiomas can exert pressure on adjacent brain structures, disrupting their normal function.
As noted by a medical expert, “The presentation of meningiomas can be quite varied, but often includes symptoms related to increased intracranial pressure or focal neurological deficits.”
Location-Specific Symptoms
The location of a meningioma significantly influences the symptoms it causes. For instance, meningiomas located near the optic nerve can lead to visual loss or double vision. Those situated in areas controlling motor functions might cause weakness or paralysis of specific parts of the body. Meningiomas affecting the brainstem or cranial nerves can result in difficulty swallowing, speech changes, or facial weakness. Understanding the specific location of a meningioma is crucial for predicting and managing its symptoms.
We recognize that each patient’s experience with meningioma symptoms can be unique, influenced by the tumor’s size, location, and the individual’s overall health. Therefore, a comprehensive evaluation is essential for determining the best course of treatment.
Fact 4: Tumor Size Significantly Impacts Symptom Severity
As meningiomas grow in size, they can exert more pressure on surrounding brain structures, leading to increased symptom severity. The size of a meningioma is a critical factor in determining the severity of symptoms experienced by patients.
How Size Affects Pressure and Mass Effect
Larger meningiomas are more likely to produce significant symptoms due to the mass effect or pressure on adjacent brain structures. This pressure can lead to a variety of symptoms, including headaches, seizures, and neurological deficits.
Key effects of larger meningioma size include:
- Increased intracranial pressure
- Compression of adjacent brain tissues
- Displacement of vital structures
We must consider these factors when evaluating the impact of meningioma size on symptom severity.
Growth Patterns and Rates
Meningiomas can exhibit varying growth patterns and rates. Some meningiomas grow slowly over many years, while others may grow more rapidly. Understanding these growth patterns is essential for predicting symptom progression and planning treatment.
Factors influencing meningioma growth rates include:
- Tumor grade and histology
- Genetic factors
- Hormonal influences
We will discuss these factors in more detail to provide a comprehensive understanding of meningioma growth patterns.
By understanding how meningioma size affects symptom severity and growth patterns, we can better manage patient care and develop effective treatment strategies.
Fact 5: Diagnosis Involves Multiple Imaging Techniques
The diagnosis of meningiomas involves a combination of imaging techniques to accurately visualize the tumor and assess its characteristics.
Imaging plays a critical role in diagnosing meningiomas. We use various imaging modalities to determine the size, location, and potential impact of the tumor on surrounding brain structures.
MRI and CT Scan Findings
Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) scans are the primary imaging techniques used in diagnosing meningiomas.
MRI Findings: MRI is particularly useful for soft tissue characterization, providing detailed images of the tumor and its relationship with adjacent structures. Meningiomas typically appear as well-defined, dural-based masses with strong contrast enhancement.
CT Scan Findings: CT scans are valuable for assessing calcifications within the tumor and evaluating bony changes. Meningiomas often show hyperostosis (thickening of the bone) adjacent to the tumor.
| Imaging Modality | Key Features for Meningioma Diagnosis |
|---|---|
| MRI | Detailed soft tissue imaging, dural-based masses, contrast enhancement |
| CT Scan | Calcification detection, bony changes, hyperostosis |
Differential Diagnosis Considerations
Differential diagnosis is crucial in distinguishing meningiomas from other intracranial tumors. We must consider other possibilities based on imaging findings.
Some key considerations include:
- Other types of brain tumors (e.g., gliomas, metastases)
- Schwannomas
- Solitary fibrous tumors
- Granular cell tumors
Accurate diagnosis requires careful evaluation of imaging characteristics, clinical presentation, and sometimes, histopathological examination.
By combining multiple imaging techniques and considering differential diagnoses, we can achieve a more accurate diagnosis and develop an effective treatment plan for patients with meningiomas.
Fact 6: Treatment Options Depend on Several Factors
The treatment of meningiomas depends on various factors, including tumor size, location, and symptoms. We understand that each patient’s situation is unique, and treatment plans are tailored accordingly.
Surgical Approaches and Considerations
Surgery is often the primary treatment for meningiomas, especially for those that are causing symptoms or are growing. The goal of surgery is to remove as much of the tumor as possible while preserving surrounding brain tissue and function.
The decision to operate depends on several factors, including:
- The tumor’s location and accessibility
- The patient’s overall health and age
- The presence and severity of symptoms
In some cases, surgery may not be possible or may be too risky. In these situations, alternative treatments are considered.
Radiation Therapy Options
Radiation therapy is another treatment option for meningiomas, particularly for tumors that cannot be completely removed surgically or are inoperable due to their location. Radiation therapy can help control tumor growth and alleviate symptoms.
There are different types of radiation therapy, including:
- Stereotactic radiosurgery (SRS)
- Fractionated stereotactic radiotherapy (FSRT)
These techniques deliver precise doses of radiation to the tumor, minimizing damage to surrounding healthy tissue.
Observation Strategy for Asymptomatic Meningiomas
For patients with asymptomatic meningiomas, particularly small tumors that are not causing any symptoms, a strategy of observation with regular monitoring may be recommended. This approach involves regular imaging studies to track the tumor’s size and growth.
The benefits of observation include:
- Avoiding unnecessary treatment and its potential side effects
- Preserving quality of life
- Intervening if the tumor shows signs of growth or becomes symptomatic
We work closely with our patients to determine the most appropriate treatment plan based on their individual circumstances.
Fact 7: Prognosis Is Generally Favorable for Most Patients
The outlook for individuals diagnosed with meningiomas is generally positive, with most patients experiencing favorable outcomes. We understand that receiving a diagnosis can be overwhelming, but it’s essential to recognize that the majority of meningiomas are benign and can be effectively managed with appropriate treatment.
Recurrence Rates and Risk Factors
One of the critical aspects of meningioma prognosis is understanding the likelihood of recurrence. Recurrence rates vary depending on the tumor’s grade and the extent of surgical removal. For benign meningiomas (WHO Grade I), the recurrence rate is relatively low, ranging from 7% to 20% over 10 years, depending on whether the tumor was completely removed. We closely monitor patients to detect any potential recurrence early, as timely intervention can significantly impact outcomes.
Several factors can influence the risk of recurrence, including:
- The tumor’s grade: Higher-grade meningiomas are more likely to recur.
- The extent of surgical resection: Tumors that are not completely removed are more likely to recur.
- Patient-specific factors: Age, overall health, and genetic predispositions can play a role.
Long-term Survival Statistics
Long-term survival for patients with meningiomas is generally good, especially for those with benign tumors. Studies have shown that the 10-year survival rate for patients with benign meningiomas is approximately 85% to 90%. For atypical and malignant meningiomas, the prognosis is less favorable, but advancements in treatment modalities continue to improve outcomes.
We emphasize the importance of regular follow-up appointments to monitor for recurrence and manage any late effects of treatment. By working closely with our patients, we can optimize their care and improve their quality of life.
In conclusion, while a meningioma diagnosis requires careful consideration and management, the prognosis for most patients is favorable. We are committed to providing comprehensive care and support to our patients, ensuring they receive the best possible outcomes.
Risk Factors and Potential Causes of Meningiomas
Research into meningiomas has uncovered several key risk factors that contribute to their development. Understanding these factors can help in the early detection and management of these tumors.
Genetic Predispositions
Certain genetic conditions can increase the risk of developing meningiomas. For instance, neurofibromatosis type 2 (NF2) is a genetic disorder that significantly raises the likelihood of meningioma development. Individuals with a family history of NF2 are at a higher risk and may benefit from regular monitoring.
Other genetic mutations, such as those affecting the SMARCB1 and SUZ12 genes, have also been associated with an increased risk of meningiomas. Genetic testing can help identify individuals with these mutations, allowing for early intervention.
Environmental and Hormonal Factors
Exposure to radiation is a known risk factor for developing meningiomas. Individuals who have undergone radiation therapy, especially at a young age, are at a higher risk of developing these tumors. The risk is dose-dependent, with higher doses of radiation leading to a greater likelihood of meningioma development.
Hormonal influences also play a role in the development of meningiomas. Meningiomas are more common in women, suggesting a possible hormonal component. Some studies have indicated that hormonal factors, such as the use of hormone replacement therapy, may influence the risk of developing meningiomas.
Other potential risk factors include certain environmental exposures, although more research is needed to fully understand their impact. We will continue to explore these factors as new evidence emerges.
Conclusion: Key Takeaways About Meningiomas and Bulging Eye Symptoms
Understanding meningiomas is crucial for patients to make informed decisions about their care. We have explored the key facts about these common brain tumors, including their potential to cause bulging eye symptoms.
Meningiomas are typically non-malignant and can vary significantly in their symptoms based on location and size. The connection between meningiomas and bulging eye symptoms is particularly significant when these tumors occur in the orbit.
By recognizing the key takeaways about meningiomas, patients can better navigate their diagnosis and treatment options. We have seen that diagnosis involves multiple imaging techniques, and treatment options depend on several factors, including tumor size, location, and patient health.
Overall, the prognosis for most patients with meningiomas is generally favorable, with a range of effective treatment strategies available. By understanding these key aspects of meningiomas, patients can take an active role in managing their condition and improving their outcomes.
FAQ
What is a meningioma?
A meningioma is a type of tumor that originates from the meninges, the protective membranes surrounding the brain and spinal cord. Most meningiomas are benign, meaning they are non-cancerous.
Are meningiomas cancerous?
Most meningiomas are not cancerous. They are typically benign tumors that grow slowly. However, some meningiomas can be malignant, although this is less common.
How common are meningiomas?
Meningiomas are among the most common types of brain tumors. They account for approximately 30% of all primary brain tumors, with a higher prevalence in women than men.
What are the symptoms of a meningioma?
Symptoms of meningiomas vary depending on their location and size. Common symptoms include headaches, seizures, and visual disturbances. Some patients may experience weakness, numbness, or personality changes.
Can meningiomas cause bulging eye symptoms?
Yes, orbital meningiomas can cause bulging eye symptoms, also known as proptosis or exophthalmos. This occurs when the tumor grows behind the eye, pushing it forward.
How are meningiomas diagnosed?
Diagnosis typically involves imaging tests such as MRI or CT scans. These tests help visualize the tumor and determine its size, location, and characteristics.
What are the treatment options for meningiomas?
Treatment depends on several factors, including the tumor’s size, location, and grade. Options may include surgical removal, radiation therapy, or observation, depending on the individual case.
Are meningiomas benign or malignant?
Most meningiomas are benign. The World Health Organization (WHO) grading system classifies meningiomas into three grades, with Grade I being benign, Grade II being atypical, and Grade III being malignant.
What is the prognosis for patients with meningiomas?
The prognosis is generally favorable for most patients, especially those with benign meningiomas. Recurrence rates vary depending on the tumor grade and extent of surgical removal.
What are the risk factors for developing meningiomas?
Risk factors include genetic predispositions, exposure to radiation, and certain hormonal influences. Women are more likely to develop meningiomas than men, suggesting a possible hormonal component.
Can meningiomas be monitored rather than treated immediately?
Yes, some meningiomas, especially small, asymptomatic ones, may be monitored with regular imaging tests rather than treated immediately. This approach is often referred to as “watchful waiting” or “active surveillance.”
FAQ
What is a meningioma?
A meningioma is a type of tumor that originates from the meninges, the protective membranes surrounding the brain and spinal cord. Most meningiomas are benign, meaning they are non-cancerous.
Are meningiomas cancerous?
Most meningiomas are not cancerous. They are typically benign tumors that grow slowly. However, some meningiomas can be malignant, although this is less common.
How common are meningiomas?
Meningiomas are among the most common types of brain tumors. They account for approximately 30% of all primary brain tumors, with a higher prevalence in women than men.
What are the symptoms of a meningioma?
Symptoms of meningiomas vary depending on their location and size. Common symptoms include headaches, seizures, and visual disturbances. Some patients may experience weakness, numbness, or personality changes.
Can meningiomas cause bulging eye symptoms?
Yes, orbital meningiomas can cause bulging eye symptoms, also known as proptosis or exophthalmos. This occurs when the tumor grows behind the eye, pushing it forward.
How are meningiomas diagnosed?
Diagnosis typically involves imaging tests such as MRI or CT scans. These tests help visualize the tumor and determine its size, location, and characteristics.
What are the treatment options for meningiomas?
Treatment depends on several factors, including the tumor’s size, location, and grade. Options may include surgical removal, radiation therapy, or observation, depending on the individual case.
Are meningiomas benign or malignant?
Most meningiomas are benign. The World Health Organization (WHO) grading system classifies meningiomas into three grades, with Grade I being benign, Grade II being atypical, and Grade III being malignant.
What is the prognosis for patients with meningiomas?
The prognosis is generally favorable for most patients, especially those with benign meningiomas. Recurrence rates vary depending on the tumor grade and extent of surgical removal.
What are the risk factors for developing meningiomas?
Risk factors include genetic predispositions, exposure to radiation, and certain hormonal influences. Women are more likely to develop meningiomas than men, suggesting a possible hormonal component.
Can meningiomas be monitored rather than treated immediately?
Yes, some meningiomas, especially small, asymptomatic ones, may be monitored with regular imaging tests rather than treated immediately. This approach is often referred to as “watchful waiting” or “active surveillance.”