Last Updated on November 27, 2025 by Bilal Hasdemir

Watching someone with glioblastoma reach the end is very hard for patients and their families. Knowing the signs of the end helps caregivers give comfort and support in these tough times.
At Liv Hospital, we put patients first. We offer caring, science-backed care for those facing this serious illness. Glioblastoma is a fast-growing brain cancer with a bad outlook. It usually leads to a short life span of less than 15 months after being diagnosed.
Knowing the signs of the end can help families and caregivers support and comfort patients. This makes the patient’s life better in their final days.
Key Takeaways
- Understanding end-of-life signs is key for the right care.
- Glioblastoma is a terminal illness with a short survival time.
- Compassionate care is vital in the final days.
- Liv Hospital focuses on patient-first, evidence-based support.
- Knowing symptoms improves the quality of life for patients.
Understanding Glioblastoma and Its Prognosis
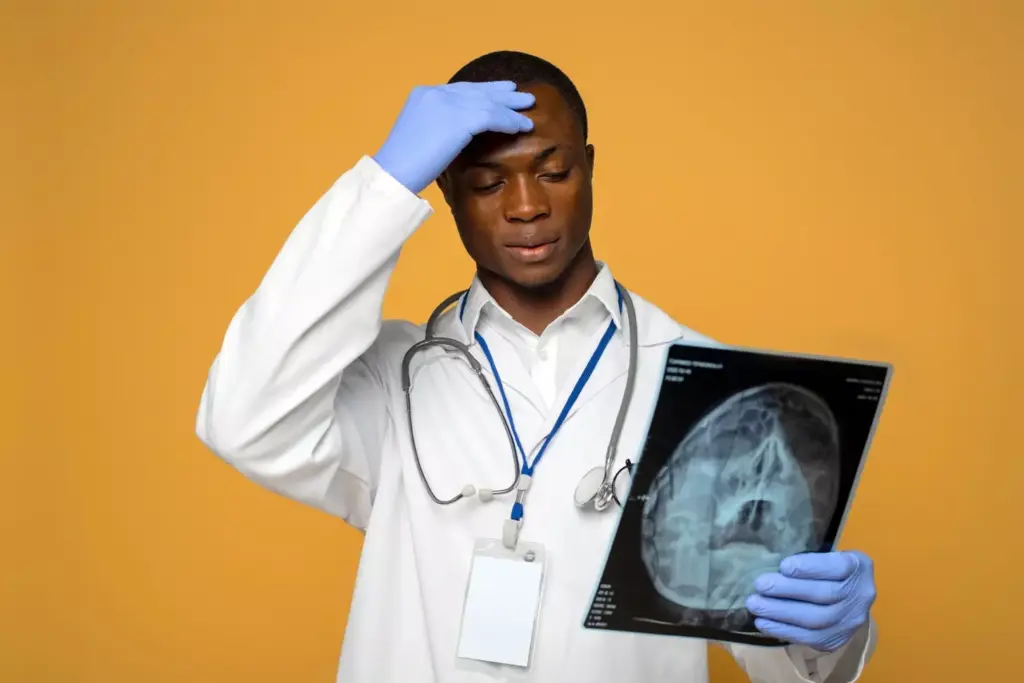
Glioblastoma is a Grade IV glioma, the most aggressive brain cancer. It has a poor prognosis. Knowing about its pathology and prognosis is key for patients and healthcare providers.
What Is Glioblastoma?
Glioblastoma starts from the brain’s glial cells. It grows fast and is hard to treat. The exact cause is unknown, but genetics and environment play a role.
As research advances, we learn more about its genetic mutations.
Classification and Grading of Gliomas
Gliomas are graded based on how much they look like normal cells. Glioblastoma is Grade IV, the highest, showing its aggressive nature.
| Grade | Characteristics | Prognosis |
|---|---|---|
| I | Low-grade, slow-growing | Favorable |
| II | Low-grade, more aggressive than Grade I | Guarded |
| III | High-grade, malignant | Poor |
| IV | High-grade, highly malignant | Very Poor |
Median Survival Rates Despite Modern Treatment
Even with modern treatments, glioblastoma patients’ median survival is less than 15 months. Survival rates depend on age, health status, and genetics.
“The prognosis for glioblastoma patients is generally poor, with a median survival of less than 15 months, highlighting the need for more effective treatment strategies.”
We aim to offer the latest treatments and support for glioblastoma patients. Our goal is to enhance their quality of life and survival chances.
The Terminal Nature of High-Grade Glioma Death

It’s important for patients and their families to understand glioblastoma’s terminal nature. Glioblastoma is a high-grade glioma known for its aggressive growth and poor treatment response. This makes it a terminal diagnosis for many.
Why Glioblastoma Is Considered Terminal
Glioblastoma is terminal because it grows fast and is hard to treat. Even with new medical technology and treatments, the outlook for glioblastoma patients is bleak. The tumor’s aggressive growth and tendency to come back after treatment make it terminal.
Key factors contributing to glioblastoma’s terminal nature include:
- Rapid tumor growth and recurrence
- Limited effectiveness of current treatments
- Poor overall survival rates
Factors Affecting Survival Time
Several factors affect how long glioblastoma patients live. These include the patient’s age, how well they can perform daily tasks, and how much of the tumor was removed during surgery. Younger patients who can perform well and have more of the tumor removed tend to live longer.
| Factor | Impact on Survival |
|---|---|
| Age | Younger patients tend to have better survival rates |
| Performance Status | Patients with good performance status have better outcomes |
| Extent of Surgical Resection | More extensive resection is associated with longer survival |
Disease Progression Timeline
The timeline for glioblastoma’s progression varies but follows a common pattern. After diagnosis, patients get treatment like surgery, radiation, and chemotherapy. But, the tumor often comes back, leading to a decline in the patient’s health.
The progression of glioblastoma can be broken down into several stages:
- Initial diagnosis and treatment
- Tumor recurrence
- Deterioration of patient condition
- End-of-life care
Knowing about glioblastoma helps manage patient expectations and care. By understanding the terminal nature of the disease and survival factors, healthcare providers can offer more compassionate and complete support to patients and their families.
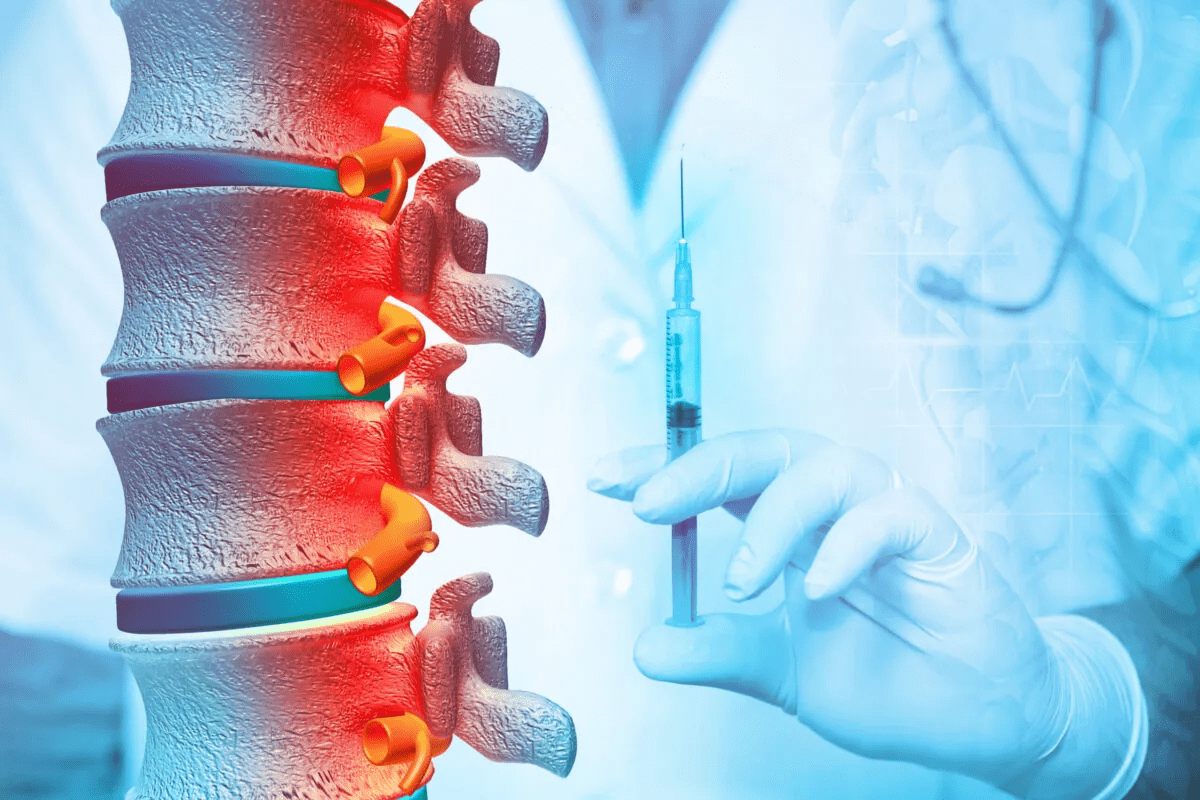
Early Signs of End-Stage Glioblastoma
When glioblastoma reaches its end stage, symptoms get worse and happen more often. This is a key time to change care plans to keep the patient comfortable and improve their life quality.
Increasing Frequency of Symptoms
Signs of end-stage glioblastoma include more headaches, seizures, and brain function loss. These symptoms get worse and happen more often, affecting daily life a lot.
Symptoms may include:
- Increased frequency of seizures
- Worsening headaches
- Enhanced cognitive decline, including memory loss and confusion
Changes in Medication Effectiveness
As glioblastoma gets worse, medicines start to work less well. This makes symptoms worse because treatments that used to help now don’t.
Adjustments in medication regimens are needed to manage symptoms. Doctors might change dosages or switch medicines to help.
Declining Performance Status
A drop in performance status is a sign of end-stage glioblastoma. Patients might feel very tired, weak, and struggle with everyday tasks.
This decline means care needs to shift. It often focuses on making the rest of life better through palliative care.
Cognitive Decline in Final Stages
Glioblastoma’s growth often leads to big changes in thinking and memory. As the tumor gets bigger, it can really affect how a person thinks and acts. This can make life harder for the patient and those who care about them. We’ll look at how glioblastoma’s final stages impact thinking and memory.
Confusion and Disorientation
Confusion and getting lost in time are big signs of thinking problems in glioblastoma patients. As the disease gets worse, people might not know where they are or what time it is. This can upset both the patient and their family a lot.
Memory Loss and Recognition Issues
Memory problems are another big issue. Patients might forget what happened recently, not know who people are, or forget important stuff. This makes talking and getting along with others harder, making care even more complicated.
Personality Changes
As glioblastoma gets worse, people’s personalities can change a lot. They might get moody, pull back, or act in ways they never did before. These changes can be hard for those taking care of them and their loved ones to handle.
| Cognitive Symptom | Description | Impact on Patient |
|---|---|---|
| Confusion and Disorientation | Difficulty understanding surroundings and time | Distress, difficulty in daily activities |
| Memory Loss | Forgetting recent events, familiar faces | Communication difficulties, dependency on caregivers |
| Personality Changes | Mood swings, withdrawal, uncharacteristic behaviors | Challenges for caregivers, emotional distress |
Cognitive decline is a big part of glioblastoma’s final stages. It shows up as confusion, memory loss, and changes in personality. Knowing about these symptoms is key to giving the right care and support to patients.
Communication Difficulties as Death Approaches
As glioblastoma gets worse, talking becomes harder. The tumor can harm the brain’s parts for speaking. This leads to many communication problems.
Progressive Speech Problems
Patients with glioblastoma often face speech issues. Speech can become slurred, slow, or hard to get because of the tumor’s impact on brain areas for language.
As the disease gets worse, patients might have:
- Dysarthria, which makes speech slurred or slow
- Aphasia, making it hard to find the right words or understand language
- Anomia, making it hard to remember names of people, places, or things
Difficulty Expressing Needs
As glioblastoma gets worse, patients find it hard to say what they need. This is because of cognitive decline, fatigue, or the effort to speak. Caregivers are key in helping by paying attention to nonverbal signs and making a supportive space for talking.
We can help by:
- Encouraging patients to speak at their own pace
- Using open-ended questions to get more detailed answers
- Being patient and understanding when speaking is hard
Nonverbal Communication Changes
Nonverbal signs like facial expressions, body language, and eye contact can also change. Patients may struggle to keep eye contact or understand social cues. This can make it hard for them to connect with others.
Knowing these changes helps caregivers adjust how they talk to patients. We should pay attention to nonverbal signals and respond in a way that comforts and supports.
By understanding and tackling these communication issues, we can better care for glioblastoma patients at the end of their lives.
Physical Symptoms in Glioblastoma’s Final Weeks
The final weeks of glioblastoma bring many tough physical symptoms. These symptoms greatly affect the patient’s life quality. To help, we need to offer full supportive care for comfort.
Extreme Fatigue and Weakness
Extreme fatigue and weakness are common in glioblastoma’s final weeks. Even simple tasks can be hard. Patients might need help with daily tasks.
Managing fatigue is key. It involves rest, good nutrition, and sometimes medicine. Fatigue comes from the tumor, treatments, and other issues like anemia or depression.
Mobility Limitations
Mobility issues are big in glioblastoma’s final stages. Patients may feel weak, numb, or paralyzed. This makes moving hard.
Physical therapy and rehab are vital. They help keep patients mobile. Simple exercises can improve life quality and prevent complications.
Swallowing Difficulties and Nutritional Challenges
Swallowing problems, or dysphagia, are common too. They can cause nutritional issues, dehydration, and pneumonia. Nutritional support is key to manage these risks.
| Nutritional Challenge | Management Strategy |
|---|---|
| Dysphagia | Dietary modifications, swallowing therapy |
| Nutritional deficiencies | Oral nutritional supplements, enteral nutrition |
| Dehydration | Fluid supplementation, monitoring hydration status |
We help patients and families create a nutritional plan. It ensures they get the nutrients and hydration they need. This helps keep them strong and comfortable.
Neurological Manifestations in End-Stage GBM
As glioblastoma reaches its end stage, patients face severe neurological symptoms. These signs show how the disease is getting worse and affect their life quality. We will look at the main symptoms in the final stages, like changes in seizures, loss of consciousness, and changes in reflexes and responses.
Seizure Activity Changes
Seizures are a big worry for glioblastoma patients. As the disease gets worse, seizures can happen more often or be more intense. We keep a close eye on these changes to help manage symptoms.
Table 1: Seizure Activity Changes in End-Stage Glioblastoma
| Seizure Characteristic | Change Observed |
|---|---|
| Frequency | Increased frequency |
| Severity | Increased severity |
| Response to medication | Decreased effectiveness |
Loss of Consciousness
Loss of consciousness is a clear sign that glioblastoma is getting worse. As the tumor grows, it can press on important brain areas. This can make the patient’s consciousness fade.
Altered Reflexes and Responses
In the end stage of glioblastoma, reflexes and responses can change a lot. These changes might mean the patient’s brain is getting worse. They could have weaker or stronger reflexes, showing brain damage.
- Decreased reflex response
- Abnormal reflexes
- Changes in pupillary response
Bodily Functions in the Last Days of Life
The last days of life for glioblastoma patients bring big changes in how their body works. These changes need careful care and support. It’s hard for patients and their caregivers as the disease gets worse.
Incontinence Issues
Incontinence is a big problem in the final stages of glioblastoma. The tumor messes with the brain’s control over the body. This can lead to losing control of bladder or bowel. It’s hard for patients and their families, so caring and managing it well is key.
Caregivers should handle incontinence with care. They can use protective clothes and set up a routine for checks and changes. This helps keep the patient’s dignity and comfort.
Changes in Breathing Patterns
As glioblastoma gets worse, breathing changes happen too. Patients might breathe irregularly, stop breathing for a bit, or have Cheyne-Stokes respiration. This can worry families, so they should know what to expect and how to comfort their loved ones.
Caregivers can make things better by creating a comfy space. They can offer gentle support and use oxygen if a doctor says it’s okay.
Temperature Regulation Problems
In the last days, glioblastoma patients might have trouble keeping their body temperature right. They might get too cold or too hot. Keeping an eye on their temperature and adjusting their space can help.
Using blankets or changing the room temperature can help them stay comfy. It’s also important to watch for signs of infection, which can cause fever. Managing it according to the patient’s plan is vital.
Knowing about these changes helps caregivers support glioblastoma patients in their final days. Being ready for incontinence, breathing changes, and temperature issues lets families give compassionate care. This makes a big difference during a tough time.
Final Hours: Physical Signs of Imminent Glioma Death
When glioblastoma is near the end, it’s important for patients and their caregivers to know the signs. These signs show that death is close. They help in giving the right care and comfort during this time.
Cool Extremities and Skin Changes
One sign is cool hands and feet. This happens because the body’s blood flow is slowing down. The skin might also look pale or blue because of this.
Mottled Appearance
Another sign is when the skin looks mottled. This means the body can’t keep its temperature right. It shows up as patches of color change, often on the hands and feet.
Rattling Breath (Death Rattle)
The “death rattle” is a rattling sound when someone breathes. It’s because the throat muscles relax and mucus builds up. It can be hard for loved ones to hear, but it’s common in the last hours of life.
| Physical Sign | Description |
|---|---|
| Cool Extremities | Hands and feet feel cool due to decreased circulation |
| Mottled Appearance | Patches of discoloration on the skin due to poor circulation |
| Rattling Breath (Death Rattle) | Rattling sound when breathing due to relaxed throat muscles and mucus accumulation |
Knowing these signs helps caregivers and family get ready for the end. It lets them give the needed comfort and support.
Variations in End-of-Life Symptoms Based on Tumor Location
The location of a glioblastoma tumor greatly affects symptoms at the end of life. Different brain areas control different functions. So, where the tumor is affects the symptoms that show up. Knowing this helps doctors tailor care to each patient’s needs.
Frontal Lobe Tumors
Glioblastomas in the frontal lobe can change personality, behavior, and thinking. Patients might see:
- Disinhibition and impulsivity
- Apathy or decreased motivation
- Difficulty with problem-solving and decision-making
- Changes in speech production, such as Broca’s aphasia
These symptoms can be hard for families and caregivers. They can change how the patient acts and talks.
Temporal Lobe Tumors
Temporal lobe glioblastomas can cause many symptoms, including:
- Seizures, which may be more frequent or severe as the disease progresses
- Auditory hallucinations or disturbances
- Memory impairments, mainly short-term memory
- Language difficulties, such as Wernicke’s aphasia
Seizures are a big worry with temporal lobe tumors. They might need changes in medication.
Brainstem Gliomas
Brainstem gliomas are rare in adults but pose big challenges. Symptoms include:
- Difficulty with speech and swallowing
- Weakness or paralysis of facial muscles
- Coordination and balance problems
- Respiratory issues due to involvement of the brainstem
These tumors often have a poor outlook. This is because of their critical location and the challenges of surgery.
Occipital and Parietal Tumors
Glioblastomas in the occipital and parietal lobes can cause:
- Visual disturbances, including blindness or visual field defects
- Spatial perception and navigation difficulties
- Sensory disturbances, such as numbness or tingling
- Difficulty with hand-eye coordination
These symptoms can make it hard for patients to interact with their world.
Knowing how tumor location affects symptoms helps doctors give better care. By understanding the specific challenges of glioblastomas in different brain areas, we can support patients and their families better in the final stages.
Conclusion: Supporting Loved Ones Through Glioblastoma’s Final Stages
Glioblastoma is a serious condition that gets worse as it progresses. It’s important to support loved ones during this tough time. This support helps keep the patient comfortable and improves their quality of life.
Caregivers are key in caring for someone with glioblastoma in its final stages. They manage symptoms and meet the patient’s needs. It’s also vital to support caregivers, helping them deal with the emotional and practical challenges of caring for someone at the end of life.
Knowing the signs and symptoms of glioblastoma’s progression helps families prepare. This knowledge allows them to offer better support. It makes the patient’s remaining time more peaceful and comfortable.
We stress the need for a caring and informed approach when supporting loved ones with glioblastoma. It’s all about meeting their unique needs during this critical time.
FAQ
What is glioblastoma, and how is it classified?
Glioblastoma, also known as glioblastoma multiforme (GBM), is a brain cancer. It starts from the brain’s glial cells. It’s classified as a Grade IV glioma, which is the most aggressive and malignant form of glioma.
What are the median survival rates for glioblastoma patients?
Despite modern treatments, glioblastoma patients’ survival rates are short. They usually live from 12 to 18 months after diagnosis.
Why is glioblastoma considered a terminal illness?
Glioblastoma is seen as terminal because it’s a very aggressive and malignant cancer. Current treatments can’t cure it. The disease always gets worse, leading to a decline in the patient’s quality of life.
What are the early signs of end-stage glioblastoma?
Early signs of end-stage glioblastoma include more frequent symptoms. Medications may not work as well. The patient’s overall performance status also declines.
How does cognitive decline manifest in the final stages of glioblastoma?
In the final stages, cognitive decline can show as confusion and disorientation. Memory issues and changes in personality also occur. These challenges are hard for patients and their caregivers.
What communication challenges do patients with advancing glioblastoma face?
Patients with advancing glioblastoma may struggle with speech problems. They find it hard to express their needs. Changes in nonverbal communication also make support from caregivers more difficult.
What physical symptoms occur in the final weeks of glioblastoma?
In the final weeks, symptoms include extreme fatigue and mobility issues. Swallowing difficulties also occur. A supportive care approach is needed to improve patient comfort.
What neurological manifestations occur in the end stages of glioblastoma?
Neurological signs in the end stages include changes in seizure activity. Loss of consciousness and changes in reflexes and responses also occur. These signs show the disease is progressing.
How do bodily functions change in the last days of life for glioblastoma patients?
In the last days, patients may experience incontinence and changes in breathing. Problems with temperature regulation also occur. Compassionate care is needed.
What physical signs indicate imminent death in glioblastoma patients?
Signs of imminent death include cool extremities and a mottled appearance. Rattling breath also indicates the end is near. This helps caregivers and family members prepare.
How does the location of the glioblastoma tumor affect end-of-life symptoms?
The tumor’s location affects end-of-life symptoms. Symptoms vary based on the tumor’s location in different brain regions, such as frontal, temporal, or brainstem areas.
What support is available for loved ones during the final stages of glioblastoma?
Caregivers and family members can get support. This includes palliative care, counseling, and respite care. These services help them cope with caring for a loved one with glioblastoma.
Is glioblastoma multiforme terminal?
Yes, glioblastoma multiforme is considered terminal. It’s currently incurable and always gets worse, leading to a decline in the patient’s quality of life.
What is the prognosis for patients with glioblastoma stage 4 after surgery?
The prognosis for patients with glioblastoma stage 4 after surgery varies. It depends on factors like the extent of tumor resection, overall health, and response to adjuvant therapies.
References
Glioblastoma Support. (n.d.). End-state symptoms of brain tumor patients. Retrieved from https://glioblastomasupport.org/end-of-life-resources/end-state-symptoms-of-brain-tumor-patients
National Center for Biotechnology Information (NCBI). (2011). End-of-life care for glioblastoma patients: A review (PMC ID: PMC3098016). Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC3098016