
Seeing changes in stool color or consistency after a surgical procedure can be scary. Bloody or black stools might mean you need to see a doctor right away.
It’s common to notice changes in bowel habits and stool look after surgery. Most of these changes are not serious and go away as you heal. But, black or bloody stools could mean something serious like bleeding in the gut.
Black tarry stools, or melena, happen when there’s bleeding higher up in the digestive system. This can be due to ulcers, gastritis, or some medicines.
Key Takeaways
- Changes in stool color or consistency after surgery can be a sign of complications.
- Bloody or black stools may indicate gastrointestinal bleeding or other serious issues.
- Understanding the causes of these changes is key to knowing what to do next.
- Seeing a doctor quickly is important if you notice persistent or severe stool changes.
- Liv Hospital’s care focuses on you, ensuring a full check-up and expert handling of post-surgery changes.
Understanding Post-Surgical Stool Changes

It’s important for patients to understand stool changes after surgery. The body goes through many changes after surgery, and stool changes are common. These changes can be due to the surgery type, medications, and the patient’s health.
Some stool changes are normal and temporary. But, others might mean there’s a problem that needs medical help.
Normal vs. Abnormal Stool Changes After Surgery
Normal stool changes can include color changes due to food or medicine. For example, some foods or medicines can make stool darker or lighter. But, abnormal stool changes like black tarry stools or bright red blood are serious signs.
Patients should watch their stool closely. Knowing when to worry is key. The table below shows common stool changes and what might cause them.
| Stool Change | Potential Cause |
| Black tarry stools | Upper gastrointestinal bleeding |
| Bright red blood in stool | Lower gastrointestinal bleeding |
| Light-colored stools | Dietary factors or medication side effects |
When to Consider Post-Surgical Stool Changes an Emergency
Not all stool changes after surgery are a worry. But, some need quick medical help. Severe abdominal pain, vomiting blood, or black tarry stools are emergencies.
Also, big changes in stool frequency or consistency, or blood in stool, need fast doctor contact. Catching problems early can help a lot.
Cause #1: Upper Gastrointestinal Bleeding
Surgery can sometimes lead to upper gastrointestinal bleeding. This can change the color of your stool. This bleeding happens in the esophagus, stomach, and the first part of the small intestine.
This type of bleeding can cause melena. Melena is when your stool turns black and tarry. It usually means there’s bleeding in the upper GI tract.
Peptic Ulcers and Gastritis After Surgery
After surgery, two main causes of upper GI bleeding are peptic ulcers and gastritis. Peptic ulcers are sores in the stomach or duodenum. They can be caused by Helicobacter pylori infection or NSAIDs. Gastritis is inflammation of the stomach lining, which can also cause bleeding.
Both conditions can get worse after surgery. Risk factors include a history of these conditions, NSAIDs use, and Helicobacter pylori infection.
| Condition | Causes | Symptoms |
| Peptic Ulcers | H. pylori infection, NSAIDs use | Abdominal pain, melena |
| Gastritis | Infection, NSAIDs, stress | Nausea, vomiting, abdominal pain |
Black Tarry Stool (Melena): What It Indicates
Melena is a serious symptom that needs immediate medical help. It shows there’s bleeding in the upper GI tract. The black color comes from blood digestion in the digestive system.
Melena means the bleeding is likely from the upper GI tract. It’s important to find the source to treat it right.
Surgical Trauma to the Upper GI Tract
Surgery can sometimes damage the upper GI tract, causing bleeding. This damage can happen during surgery or by accident.
Surgical trauma is a known risk of some surgeries. It’s key for doctors to watch for bleeding signs after surgery.
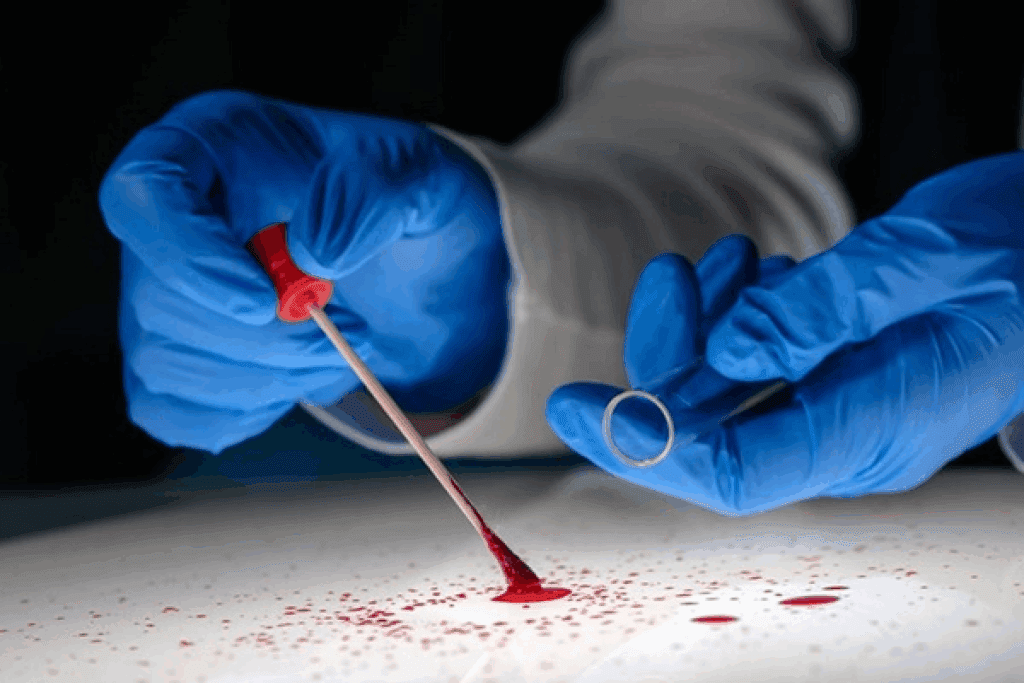
Cause #2: Lower Gastrointestinal Bleeding and Bloody Stool After Surgery
After surgery, lower gastrointestinal bleeding can show up as bright red blood in the stool. This is a serious issue, mainly for those who have had colorectal surgery.
Bright Red Blood in Stool: What It Means
Bright red blood in stool usually means lower gastrointestinal bleeding. This symptom is alarming and needs quick medical check-up. It suggests the bleeding is from the lower colon or rectum.
The bleeding might be from surgical trauma or surgery complications. Finding the bleeding source is key to the right treatment.
Surgical Site Bleeding in Colorectal Procedures
Colorectal surgery can lead to bleeding at the surgical site, causing bloody stools. The surgery’s complexity and the patient’s health affect the risk of such issues.
| Risk Factors | Description |
| Surgical Complexity | The more complex the surgery, the higher the risk of bleeding. |
| Patient Health | Pre-existing conditions can increase the risk of surgical site bleeding. |
| Post-Surgical Care | Inadequate post-surgical care can lead to complications, including bleeding. |
Anastomotic Leaks and Complications
An anastomotic leak is a serious issue after colorectal surgery. It happens when the surgical connection between intestine parts fails, causing leakage. This can lead to severe bleeding, infection, and other serious problems.
Symptoms of an anastomotic leak include severe abdominal pain, fever, and bloody stools. Quick medical help is vital to manage this condition well.
Cause #3: Medication-Related Stool Changes
After surgery, some medications can change stool color or consistency. These changes might worry you, but knowing how meds affect stool can help. It makes managing these changes easier for both patients and doctors.
Blood Thinners and NSAIDs
Blood thinners and NSAIDs are given after surgery to stop blood clots and ease pain. But, they can irritate the stomach, causing bloody or black stools. Blood thinners can also make the digestive tract bleed more. NSAIDs might lead to stomach ulcers and gastritis.
Iron Supplements and Bismuth-Containing Medications
Iron supplements are given to those who lost a lot of blood during surgery. They can make stools black or dark green because of the iron. Bismuth medications, used for stomach issues, can also darken stool. These changes are usually not dangerous but can be scary if you’re not expecting them.
Antibiotics and Their Effect on Stool
Antibiotics are often used after surgery to prevent or treat infections. But, they can upset the balance of gut bacteria. This can lead to diarrhea. In some cases, antibiotics can cause Clostridium difficile infection, a serious issue that needs quick medical care.
Knowing how post-surgical meds can affect stool helps patients during recovery. If your stool changes a lot or don’t go back to normal, talk to your doctor. They can figure out why and what to do next.
Cause #4: Hemorrhoids and Anal Fissures
Surgery and anesthesia can make hemorrhoids and anal fissures worse. Hemorrhoids are swollen veins in the lower rectum or anus. Anal fissures are small tears in the anus lining. Both can cause a lot of pain and discomfort.
How Surgery and Anesthesia Exacerbate Existing Hemorrhoids
Surgery and anesthesia can make hemorrhoids worse in several ways. The patient’s position and the pressure from surgical tools can strain the veins. Anesthesia can also change bowel habits, leading to constipation, which can make hemorrhoids worse.
Also, opioids used for pain can slow down bowel movements, causing constipation. This constipation can strain the veins, making hemorrhoids worse.
Post-Surgical Constipation and Straining
Constipation after surgery is common and can lead to straining. Straining puts more pressure on the veins, which can cause or worsen hemorrhoids. Anal fissures can also make patients hesitant to have bowel movements, leading to more constipation.
To reduce these risks, patients are advised to eat a high-fiber diet, stay hydrated, and be active soon after surgery. Stool softeners may also be given to prevent constipation and reduce straining.
Treatment Options for Post-Surgical Hemorrhoids
Treating post-surgical hemorrhoids involves lifestyle changes and medical treatments. Eating more fiber can help soften stool and reduce straining. Drinking enough water is also key to preventing constipation.
- Topical treatments like creams or ointments can help with pain and inflammation.
- Sitz baths can offer relief and help with healing.
- In some cases, procedures like rubber band ligation or sclerotherapy may be needed for persistent hemorrhoids.
For anal fissures, treatments include topical nitroglycerin or botulinum toxin injections. These help relax the anal sphincter and aid in healing. In severe cases, surgery might be necessary.
It’s important for patients to talk to their healthcare provider about symptoms and treatment options. This helps find the best approach for their situation.
Cause #5: Specific Surgical Procedures and Stool Changes
Some surgeries can change how our digestive system works, affecting our stool. Operations like gallbladder removal, hysterectomy, and cesarean section can impact bowel movements and stool.
Gallbladder Surgery (Cholecystectomy)
Removing the gallbladder can change bile flow, affecting stool color and consistency. After this surgery, patients might see:
- Diarrhea or loose stools from bile flow into the intestine
- Stool color changes, making it lighter or more yellow
- Higher risk of not absorbing bile salts well, affecting stool consistency
Table: Possible Stool Changes After Cholecystectomy
| Stool Characteristic | Pre-Surgery | Post-Surgery |
| Color | Normal brown | Lighter or yellowish |
| Consistency | Normal | Loose or diarrhea |
| Frequency | Normal | Increased |
Hysterectomy and Bowel Function Changes
A hysterectomy can affect bowel function indirectly. Changes may include:
- Constipation from changes in pelvic floor anatomy or pain
- Possible nerve damage during surgery, affecting bowel habits
- Adhesions or scar tissue that can impact bowel movements
Cesarean Section and Post-Operative Stool Changes
A cesarean section can cause stool changes post-surgery. These changes may include:
- Constipation from pain, anesthesia, or narcotics
- Changes in bowel habits from the surgical stress response
- Higher risk of hemorrhoids from constipation and straining
In conclusion, different surgeries can change stool characteristics. Knowing these changes helps patients and doctors manage recovery better.
Cause #6: Dietary Factors Affecting Stool Color
What you eat can change the color of your stool after surgery. Some foods can make your stool darker, which might worry you. Knowing how diet affects stool color helps manage your expectations and spot problems early.
Foods That Can Cause Black or Dark Stool
Some foods can make your stool black or dark. These include:
- Black licorice
- Blueberries
- Iron-rich foods like spinach and red meat
- Certain medications and supplements, such as iron supplements
Black stools can also mean upper gastrointestinal bleeding. If you see black stools, think about your diet and any other symptoms.
Dietary Recommendations During Post-Surgical Recovery
Follow a balanced diet that’s easy on your stomach during recovery. This might include:
- Eating small, frequent meals
- Avoiding spicy or fatty foods
- Staying hydrated by drinking plenty of water
- Incorporating foods rich in fiber to promote regular bowel movements
Slowly adding normal foods to your diet can ease digestive discomfort.
| Food Type | Effect on Stool Color | Recommendation |
| Iron-rich foods | Can cause dark or black stools | Consume in moderation |
| Beets | Can cause red or pink stools | Enjoy in moderation, if you’re not used to eating beets |
| Blueberries and black licorice | Can cause dark stools | Avoid eating too much, if you notice stool color changes |
Distinguishing Diet-Related Changes from Complications
Diet can change stool color, but it’s important to know the difference from complications. If you see:
- Persistent black stools
- Bloody stools
- Severe abdominal pain
- Fever or chills
Seek medical help right away. These signs could mean a serious issue that needs quick attention.
Being aware of your diet and how it affects your stool helps you navigate recovery better. It also helps you spot any issues early.
Cause #7: Post-Surgical Infections and Inflammatory Conditions
After surgery, infections and inflammation can harm stool quality and recovery. Patients may get infections or have inflammation that affects their gut health.
Clostridium Difficile Infection
Clostridium difficile, or C. diff, is a bacterial infection that can happen after surgery. It’s more common in those who have taken antibiotics. This infection leads to severe diarrhea, stomach pain, and other gut problems.
Antibiotics can upset the balance of gut bacteria, letting C. diff grow and cause infection. It’s important for patients to know the risks and signs of C. diff infection. These include:
- Watery diarrhea
- Abdominal cramps
- Fever
- Blood in stool
Inflammatory Bowel Conditions Triggered by Surgery
Surgery can start or make inflammatory bowel conditions like Crohn’s disease or ulcerative colitis worse. These conditions can change stool to be loose, bloody, and painful.
The exact reasons surgery can trigger IBD are not clear. But, stress from surgery, changes in gut bacteria, and other factors might play a role.
Signs of Infection vs. Normal Recovery
Telling normal recovery from infection or inflammation is key. Some discomfort and bowel changes are okay after surgery. But, some symptoms might mean a problem.
Signs of infection or inflammation include:
| Symptom | Normal Recovery | Possible Infection/Inflammatory Condition |
| Diarrhea | Mild, temporary | Severe, persistent |
| Blood in Stool | Rare, minimal | Frequent, significant |
| Abdominal Pain | Mild, manageable | Severe, worsening |
Patients should watch their symptoms closely. If they notice anything odd, they should tell their doctor right away.
What to Do When You Experience Abnormal Stool After Surgery
If you’ve noticed unusual changes in your stool after surgery, it’s essential to understand what to do next. Abnormal stool can manifest in various forms, such as bloody or black stool, and it’s critical to address these changes promptly.
Immediate Steps to Take
Upon noticing abnormal stool after surgery, the first step is to contact your healthcare provider. They will guide you on the immediate actions to take based on the severity of your symptoms.
- Document your symptoms: Keep a record of the changes you’ve observed in your stool, including the frequency and any associated symptoms like pain or dizziness.
- Stay hydrated: Drink plenty of fluids to help prevent dehydration, specially if you’ve experienced bleeding or diarrhea.
- Avoid strenuous activities: Rest and avoid heavy lifting or bending to minimize the risk of exacerbating any underlying conditions.
Information to Provide Your Healthcare Provider
When you contact your healthcare provider, it’s essential to provide detailed information about your symptoms. This includes:
| Information | Details to Include |
| Symptom Description | Describe the color, consistency, and frequency of your stool. |
| Associated Symptoms | Mention any other symptoms you’re experiencing, such as abdominal pain or fever. |
| Medication and Supplements | List any medications or supplements you’re taking, as they may be relevant to your condition. |
Diagnostic Tests You May Undergo
Your healthcare provider may recommend various diagnostic tests to determine the cause of your abnormal stool. These tests can include:
- Endoscopy: A procedure that allows your doctor to visually examine the inside of your gastrointestinal tract.
- Imaging tests: X-rays, CT scans, or MRI scans may be used to identify any abnormalities or complications.
- Stool tests: Analyzing a stool sample can help identify infections or other conditions affecting your bowel movements.
Treatment Approaches Based on Causes
The treatment for abnormal stool after surgery depends on the underlying cause. Your healthcare provider will recommend a treatment plan based on the diagnosis.
“The key to managing abnormal stool after surgery is prompt evaluation and treatment. By understanding the cause, healthcare providers can offer targeted therapies to alleviate symptoms and prevent complications.”
For instance, if the cause is related to medication, adjusting your prescription may resolve the issue. In cases of infection, antibiotics or other antimicrobial therapies might be necessary.
By following these steps and working closely with your healthcare provider, you can effectively manage abnormal stool after surgery and ensure a smoother recovery.
Conclusion: Monitoring Your Recovery Through Stool Changes
Watching your stool changes after surgery is key for a smooth recovery. Different things can change your stool’s color and texture, like bleeding or what you eat. Knowing these changes can help you stay healthy and catch problems early.
Understanding why your stool might be bloody or black can help you act fast. This includes knowing about bleeding, the effects of medicines, and how food affects you. Your doctor can help you know what to expect and how to handle any stool changes.
Good recovery monitoring means watching your stool closely and talking to your healthcare team. This way, you can quickly deal with any issues. It helps you recover well.
FAQ
What causes black tarry stool after surgery?
Black tarry stool, or melena, often means there’s bleeding in the upper gut. This can happen due to peptic ulcers or gastritis. Surgery might make these problems worse or start them.
Is bloody stool after surgery a serious condition?
Yes, bloody stool after surgery is serious. It could mean there’s bleeding in the gut, which needs quick medical help. How serious it is depends on the cause and how much blood is lost.
Can certain medications cause changes in stool color after surgery?
Yes, some medicines can change stool color. This includes blood thinners, NSAIDs, iron pills, and meds with bismuth. These can affect how your stool looks and feels.
How does gallbladder surgery affect stool color and consistency?
Gallbladder surgery can change how your stool looks and feels. Some people might get diarrhea or have lighter-colored stools. This is because the surgery changes how bile moves through your body.
Can diet affect stool color after surgery?
Yes, what you eat can change your stool color. Foods high in iron or certain meds can do this. Beets are another example. It’s key to know if these changes are just from food or if they’re a sign of something more serious.
What are the signs of infection versus normal recovery in stool changes after surgery?
Signs of infection include diarrhea that won’t stop, bloody stools, a lot of belly pain, and fever. Normal recovery might have some stool changes, but these are usually mild and short-lived.
What should I do if I experience abnormal stool after surgery?
If your stool changes after surgery, call your doctor right away. Tell them about your symptoms, like stool color, how it looks, and how often you have it.
Can surgery trigger or exacerbate inflammatory bowel conditions?
Yes, surgery can make inflammatory bowel conditions worse in some people. This might cause diarrhea or bloody stools.
Are there any dietary recommendations for managing stool changes during post-surgical recovery?
Yes, eating a balanced diet and drinking plenty of water can help with stool changes. Also, avoid foods that might irritate your gut or change your stool color.
What diagnostic tests may be performed to investigate abnormal stool after surgery?
Tests like endoscopy, colonoscopy, imaging, and stool tests might be used to find out why your stool is different. The tests depend on what your doctor thinks might be causing the problem.
References
- Pietrangelo, A. (2024). Managing weight loss after gallbladder removal. Medical News Today. Retrieved from https://www.medicalnewstoday.com/articles/317659



































