
We know how vital accurate diagnosis is for vascular health. Abdominal aortic aneurysm ultrasound is a safe way to see the aorta clearly. It’s key for spotting and keeping an eye on AAA.
At Liv Hospital, we take protocols seriously for good care and planning. Our team works hard to offer top-notch healthcare. We also support international patients fully.
Key Takeaways
- Accurate measurements are key in abdominal aortic aneurysm ultrasound.
- Standardized protocols help with good care and planning.
- Non-invasive imaging gives clear, real-time views.
- Liv Hospital aims for the best in healthcare.
- We offer full support to international patients.
Understanding Abdominal Aortic Aneurysms
Abdominal aortic aneurysms (AAA) are a serious condition where the abdominal aorta gets too big. Understanding AAA’s definition, how it works, and what increases the risk is key. We’ll dive into these topics to help you understand AAA better.
Definition and Pathophysiology
An AAA is when the abdominal aorta gets bigger than 1.5 times its normal size. The normal size is about 2 cm. So, an aneurysm is usually diagnosed when it’s over 3 cm.
The causes of AAA are complex. Genetics, environment, and how the aorta works together weaken the aortic wall. This leads to an aneurysm forming.
Risk Factors and Clinical Significance
There are many risk factors for AAA. Knowing these helps us find who’s at higher risk.
Age and Gender Considerations
Age is a big risk factor, with more cases after 65. Men are more likely to get AAA than women, with a 4:1 to 6:1 male-to-female ratio.
Genetic and Lifestyle Factors
Having a family history of AAA raises your risk. Smoking and high blood pressure also play big roles in getting and growing AAA.
| Risk Factor | Description | Impact on AAA Development |
|---|---|---|
| Age | Increased incidence after 65 years | High |
| Gender | Male predominance | Moderate to High |
| Smoking | Significant risk factor | High |
| Family History | Increased risk with affected first-degree relatives | Moderate to High |
The Importance of Early Detection and Monitoring

Early detection and monitoring of abdominal aortic aneurysms (AAA) are key to preventing rupture and lowering death rates. It’s vital to catch AAA early. This lets doctors check the risk of rupture and plan the best course of action.
Rupture Risk Assessment
Figuring out the risk of rupture is a big part of managing AAA. Doctors look at the size and growth of the aneurysm, along with the patient’s health. Accurate AAA measurements are key to understanding the risk and deciding on treatment.
Mortality Rates and Prevention
AAA rupture is very dangerous, which makes early detection and prevention even more important. Finding AAA early lets doctors keep an eye on it and act before it ruptures. This can greatly improve a patient’s chances of survival.
Critical Size Thresholds
Certain sizes of aneurysms are considered high-risk and may need surgery. Usually, this is when they reach 5.5 cm or bigger. Regular monitoring of smaller ones is also important. This helps catch any growth early and prevent them from becoming too big.
Abdominal Aortic Aneurysm Ultrasound: Principles and Benefits
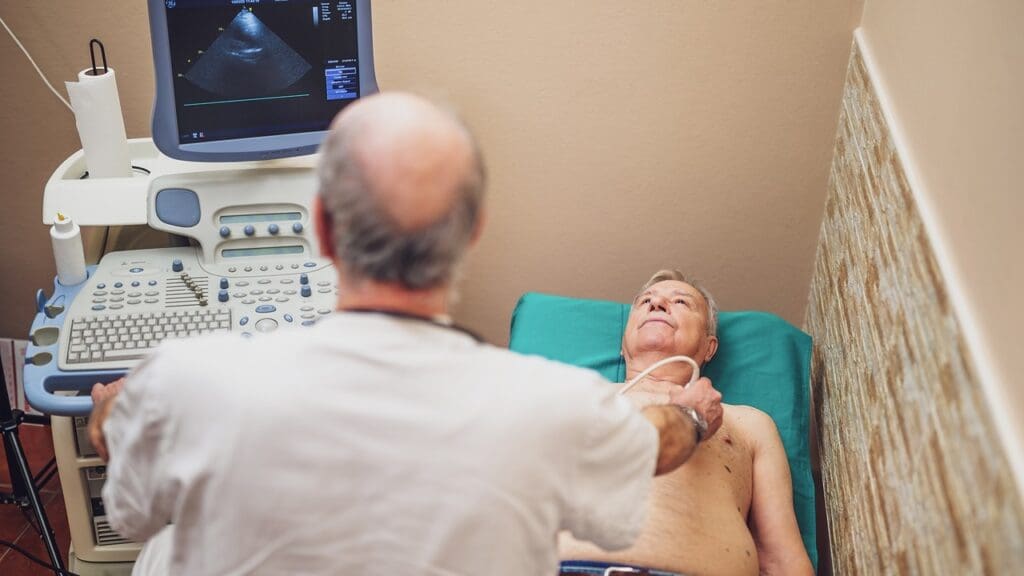
Ultrasound is key in finding and watching abdominal aortic aneurysms (AAAs). It’s non-invasive and shows images in real-time. This makes it a top choice for doctors.
Real-Time High-Resolution Imaging
Ultrasound gives real-time high-resolution images of the aorta. It lets doctors measure and check the aorta accurately. This is vital for spotting aneurysms and tracking how they grow.
Non-Invasive Nature and Patient Comfort
The non-invasive nature of ultrasound makes it safe and comfy for patients. It doesn’t need contrast agents or radiation, unlike some other tests. This makes it perfect for regular checks and long-term watching.
Cost-Effectiveness for Routine Screening
Ultrasound is also cost-effective. This is a big plus for regular screenings. It’s cheap and easy to get, helping find AAAs early. This can lower the risk of aneurysm rupture and save lives.
Using ultrasound’s benefits, we can better find and manage abdominal aortic aneurysms. This helps improve how well patients do.
Normal vs. Aneurysmal Aorta: Diagnostic Criteria
To diagnose abdominal aortic aneurysms (AAA), it’s key to know the normal aorta size and what makes it aneurysmal. The aorta’s normal size changes with age. This is important for spotting an aneurysm.
Normal Abdominal Aorta Dimensions
The normal aorta size is usually under 2 cm in adults. But, size can differ based on age, sex, and body size.
Age-Related Changes
As we get older, the aorta can grow a bit. Knowing these changes helps doctors make accurate diagnoses.
Threshold for AAA Diagnosis
A diameter of 3 cm or more is seen as the AAA diagnosis mark.
The 3cm Criterion
The 3 cm rule is widely used to spot AAA. Ultrasound imaging is a trusted way to measure the aorta’s size.
| Aorta Diameter (cm) | Diagnosis |
|---|---|
| < 2 | Normal |
| 2-3 | Borderline |
| ≥ 3 | Abdominal Aortic Aneurysm (AAA) |
It’s vital for doctors to know these criteria. This helps them diagnose and treat abdominal aortic aneurysms correctly.
Equipment Selection and Optimization
To get accurate AAA measurements, we need to optimize our ultrasound equipment. Choosing the right equipment and adjusting it properly is key for clear images.
Transducer Selection
Picking the right transducer is critical for seeing the aorta well. We often use convex or curvilinear transducers. They give us a wider view.
Machine Settings for Optimal Visualization
Adjusting machine settings is important for the best image quality. We focus on:
- Depth adjustments to make sure the aorta is in the center and fully seen.
- Gain adjustments to make the image bright without adding noise.
Depth and Gain Adjustments
Getting the depth and gain right makes images clearer. We set the depth to see the whole aorta. Then, we adjust the gain to cut down on noise.
Color Doppler Applications
Color Doppler helps us check blood flow and find leaks or clots in the aneurysm. It’s great for understanding the aorta’s blood flow.
Step 1: Patient Preparation and Aorta Localization
Getting an accurate ultrasound of the abdominal aortic aneurysm starts with good preparation and finding the aorta. These steps are key to getting clear images and a correct diagnosis.
Optimal Patient Positioning
It’s important to position the patient right for a clear view of the aorta. They should lie flat on their back with their head a bit up. This helps relax the stomach muscles.
Fasting Requirements
Patients need to fast for at least 8 hours before the ultrasound. This reduces gas in the bowels, making the aorta easier to see.
Anatomical Landmarks for Aorta Identification
To find the aorta, we look for certain body landmarks. The xiphoid process and the belly button are good starting points. The aorta is usually found on the left side, in front of the spine.
Transducer Orientation Techniques
Using the right angle for the transducer is critical for good images. We start with a side view to spot the aorta. Then, we turn the transducer to get a front view.
| Preparation Step | Description |
|---|---|
| Patient Positioning | Supine position with head slightly elevated |
| Fasting | At least 8 hours prior to ultrasound |
| Aorta Localization | Using anatomical landmarks like xiphoid process and umbilicus |
Step 2: Proximal Aorta Measurement Protocol
Measuring the proximal aorta accurately is key to diagnosing abdominal aortic aneurysms (AAA). We use a detailed protocol that includes both transverse and longitudinal scanning. This ensures we get precise measurements.
Transverse and Longitudinal Scanning Approaches
We start with transverse scanning to see the proximal aorta. This helps us check its size and look for any aneurysms. Then, we use longitudinal scanning to measure the aorta’s length and confirm any aneurysms. This method gives us a full view of the proximal aorta.
Suprarenal Aorta Assessment
Checking the suprarenal aorta is very important. It tells us how big the aneurysm is and where it is in relation to major arteries. We focus on the celiac and superior mesenteric arteries because they are key for measuring correctly.
Relationship to Celiac and Superior Mesenteric Arteries
The celiac and superior mesenteric arteries are important for measuring the suprarenal aorta. By finding these landmarks, we can see how close the aneurysm is to these vital arteries.
Common Challenges and Solutions
One big challenge is bowel gas getting in the way. It can block our view of the aorta. To fix this, we adjust the patient’s position or use gentle pressure with the probe. These steps help us get clear AAA ultrasound images and accurate measurements.
Step 3: Mid-Aortic Segment Evaluation Techniques
When doing an AAA ultrasound, checking the mid-aortic segment is key. This area is important because it has the renal artery origins. These are vital landmarks.
Identifying Renal Artery Origins
To check the mid-aortic segment, we first find the renal artery origins. These arteries split off from the aorta, just below the superior mesenteric artery. It’s important to see these origins clearly to measure the aorta’s size right and spot any changes.
Capturing True Perpendicular Views
Getting true perpendicular views of the aorta is key for accurate measurements. We adjust the ultrasound probe to get a circular view of the aorta. Staying away from oblique views is important to avoid overestimating the aorta’s size.
Avoiding Oblique Measurements
To avoid oblique views, we make sure the ultrasound beam hits the aortic wall straight on. This might mean adjusting the probe’s angle and position a bit. Using the right technique is essential for getting good measurements.
Documenting Maximum Diameter
Lastly, we record the biggest diameter of the mid-aortic segment. This is key for spotting and tracking AAA. We measure from the outer edge of the aortic wall to the other, giving a true size of the aneurysm.
Step 4: Distal Aorta and Iliac Bifurcation Assessment
Checking the distal aorta and iliac bifurcation is key in AAA ultrasound imaging. It’s important for diagnosing and tracking AAA.
Navigating Bowel Gas Interference
Bowel gas can make imaging hard. We adjust the patient’s position or use compression to move gas. Optimizing the ultrasound image is key for precise measurements.
Measuring at the Aortic Bifurcation
Measuring the aorta at the bifurcation needs careful technique. We make sure our measurements are correct, following the standardized protocol for AAA ultrasound measurements.
Iliac Artery Evaluation
Checking the iliac arteries is a big part of the AAA ultrasound exam. We look at the common iliac arteries for signs of aneurysm.
Common Iliac Aneurysm Detection
Finding common iliac aneurysms is very important. They can be linked to AAA. We examine the iliac arteries closely and note any issues.
By using these steps and techniques, we can accurately check the distal aorta and iliac bifurcation. This is vital for managing AAA patients.
Step 5: Standardized Measurement Techniques
The fifth step in our AAA ultrasound protocol uses standardized measurement techniques. These techniques ensure consistency and accuracy. They are key for diagnosing and monitoring abdominal aortic aneurysms (AAAs).
Inner-to-Inner Wall Method
The inner-to-inner wall method is a common way to measure the aorta’s diameter. It measures from the inner edge of the front wall to the inner edge of the back wall.
Applications and Limitations
This method is great for finding the maximum diameter of an aneurysm. But, it might not work well with a lot of thrombus or wall calcification.
Outer-to-Outer Wall Method
The outer-to-outer wall method measures from the outer edge of the front wall to the outer edge of the back wall. It’s often used for watching and monitoring AAAs.
Clinical Implications
This method gives a full view of the aneurysm size, including any thrombus. This is important for planning treatment and managing patients.
Leading-Edge-to-Leading-Edge Technique
The leading-edge-to-leading-edge technique measures from the leading edge of the front wall to the leading edge of the back wall. It’s often used with other imaging methods.
As the Society for Vascular Surgery says, “Standardized measurement techniques are key for accurate aorta measurements.”
“The use of standardized measurement techniques is essential for the accurate diagnosis and monitoring of abdominal aortic aneurysms.”
Impact on Treatment Planning
The choice of measurement technique greatly affects treatment planning and patient outcomes. Using standardized techniques ensures our patients get consistent and accurate diagnoses. This leads to better care.
Step 6: Thrombus Identification and True Lumen Assessment
Accurate thrombus identification and true lumen assessment are key in abdominal aortic aneurysm (AAA) ultrasound imaging. These steps are vital for a complete evaluation and diagnosis.
Recognizing Intraluminal Thrombus
Intraluminal thrombus is common in many AAAs. Its presence can greatly affect the aneurysm’s risk. Thrombus identification is critical for determining the aneurysm’s true size and rupture risk.
Echogenicity Patterns
The echogenicity of the thrombus can vary. It can appear as hyperechoic, isoechoic, or hypoechoic areas in the aneurysm sac. Recognizing these patterns helps in distinguishing thrombus from the true lumen.
Measuring True vs. False Lumen
Distinguishing between the true and false lumen is vital, even when the aneurysm distorts the aortic anatomy. True lumen assessment involves identifying the lumen that is in continuity with the aortic flow.
Avoiding Measurement Pitfalls
To ensure accurate measurements, it’s important to avoid common pitfalls. Techniques for accurate dimension capture include using multiple imaging planes and optimizing machine settings.
Techniques for Accurate Dimension Capture
Using standardized measurement techniques and being aware of artifacts is key to accurate AAA assessment. This includes using the correct gain settings and ensuring the ultrasound beam is perpendicular to the aorta.
By following these guidelines and techniques, healthcare professionals can improve the accuracy of AAA ultrasound assessments. This leads to better patient outcomes.
Step 7: Documentation and Surveillance Protocols
Accurate documentation and surveillance are key for managing abdominal aortic aneurysms (AAAs) found through ultrasound. We use standardized processes to give our patients the best care.
Standardized Reporting Templates
Standardized reporting templates are important for keeping care consistent. They include vital info like:
- Maximum aneurysm diameter
- Aneurysm location and extent
- Presence of thrombus or other complicating features
Image Acquisition Requirements
Getting high-quality images is essential for accurate AAA assessment. We follow strict protocols for image capture, including:
- Transverse and longitudinal views of the aorta
- Measurements at multiple levels
- Documentation of any abnormalities
Follow-up Scheduling Based on AAA Size
Follow-up plans are based on the aneurysm’s initial size. This helps tailor monitoring and planning for treatment.
Small Aneurysm Monitoring
Small aneurysms (less than 4 cm) need regular ultrasound checks, usually every 6-12 months. The schedule can change based on the patient and doctor’s judgment.
Large Aneurysm Management
Larger aneurysms (5.5 cm or more) need closer monitoring, often every 3-6 months. These cases often involve vascular surgery specialists to decide when to intervene.
Following these protocols helps us give our patients the best care for their AAAs. This approach reduces risks and improves their health outcomes.
Conclusion: Ensuring Accurate AAA Detection and Management
It’s vital to detect and manage abdominal aortic aneurysms (AAA) correctly to prevent rupture and save lives. We’ve shared the 7 key steps for accurate measurement using abdominal aorta ultrasound. This tool is key in diagnosing AAA.
Effective management of AAA depends on precise measurements from aortic aneurysm ultrasound. By following these steps, healthcare professionals can ensure accurate detection and monitoring. This leads to better patient outcomes.
Standardized protocols in aaa on ultrasound are essential for consistent and reliable results. Accurate detection of AAA is the base of effective management. It allows for timely interventions and lowers the risk of rupture.
By using abdominal aorta ultrasound and following best practices, we can improve patient care and outcomes in AAA management. Our dedication to top-notch healthcare helps international patients get the advanced medical treatments they need.
What is an abdominal aortic aneurysm (AAA) and how is it diagnosed using ultrasound?
An abdominal aortic aneurysm is when the aorta in your belly gets bigger. Doctors use ultrasound to check its size. If it’s 3cm or bigger, it’s considered an aneurysm.
What are the benefits of using ultrasound for AAA detection and monitoring?
Ultrasound is safe, shows what’s happening in real time, and is easy on the wallet. It’s perfect for checking and watching over AAAs.
How is the size of an abdominal aortic aneurysm measured on ultrasound?
Doctors use special ways to measure the aorta’s size. They look at the inside or outside walls. This makes sure the measurements are right and the same every time.
What is the significance of the 3cm criterion in diagnosing AAA?
The 3cm mark is important because it means the aorta is really big. This increases the risk of it bursting. So, doctors need to keep an eye on it or take action.
How often should patients with a small AAA undergo ultrasound surveillance?
How often depends on the size of the aneurysm. Smaller ones are checked less often than bigger ones.
What are the key steps in performing an AAA ultrasound examination?
First, the patient gets ready. Then, the doctor finds the aorta. They measure it at different points and look for blood clots. They follow strict rules to document everything.
How is thrombus identified and assessed during an AAA ultrasound?
Blood clots are seen as bright spots in the aneurysm. The doctor notes how big they are and where. This helps figure out the risk of problems.
What are the challenges in visualizing the aorta during ultrasound, and how can they be overcome?
Seeing the aorta can be hard because of gas in the bowel or the patient’s body shape. Adjusting the patient’s position or using different tools can help see better.
How do ultrasound measurements of AAA influence treatment planning?
The size of the aneurysm helps decide what to do next. Big ones or ones growing fast might need surgery or a special repair.
What is the role of standardized reporting in AAA ultrasound?
Standardized reports make sure all important details are written down the same way. This helps doctors talk to each other clearly and plan care better.
References
- ACEP Sonoguide (Basic Aorta) : https://www.acep.org/sonoguide/basic_aorta
- PMC – PubMed Central : https://pmc.ncbi.nlm.nih.gov/articles/PMC6350491























