Last Updated on October 21, 2025 by mcelik

Autoimmune disorders are tricky to spot because the body’s immune system attacks its own tissues. Advanced imaging like MRI has changed how we diagnose and track these conditions. MRI is key in finding autoimmune diseases that harm the brain.
In recent years, autoimmune disease brain MRI has become an essential tool for detecting inflammation, lesions, and other abnormalities caused by immune system dysfunction. It helps doctors better understand how these diseases affect brain structures.
We’ll look into how MRI helps diagnose and keep an eye on autoimmune diseases, focusing on brain-related ones. Knowing what MRI scans can do helps both patients and doctors during diagnosis.
Key Takeaways
- Understanding the role of MRI in diagnosing autoimmune diseases.
- The benefits of using MRI scans for monitoring autoimmune disorders.
- How MRI technology is advancing the field of autoimmune disease diagnosis.
Understanding Autoimmune Diseases and Diagnostic Challenges
Autoimmune diseases are complex and hard to diagnose. They happen when the body’s immune system attacks its own tissues. This can affect many parts of the body.
What Are Autoimmune Diseases?
Autoimmune diseases include conditions like rheumatoid arthritis, lupus, and multiple sclerosis. They can cause a wide range of symptoms. This makes them hard to diagnose.
Common Autoimmune Diseases and Their Symptoms:
| Disease | Primary Symptoms |
| Rheumatoid Arthritis | Joint pain, swelling, and stiffness |
| Lupus | Fatigue, fever, skin rashes, joint pain |
| Multiple Sclerosis | Vision problems, muscle weakness, coordination issues |
The Diagnostic Journey for Autoimmune Conditions
Diagnosing autoimmune diseases is a long and complex process. It involves clinical evaluation, lab tests, and sometimes MRI. Many symptoms are not specific, making diagnosis tough.
MRI is becoming key in diagnosing autoimmune diseases. It shows detailed images of affected tissues and organs. This helps identify specific damage or inflammation patterns.
Understanding autoimmune diseases and their diagnosis challenges is important. Advanced tools like MRI play a big role in managing these complex conditions.
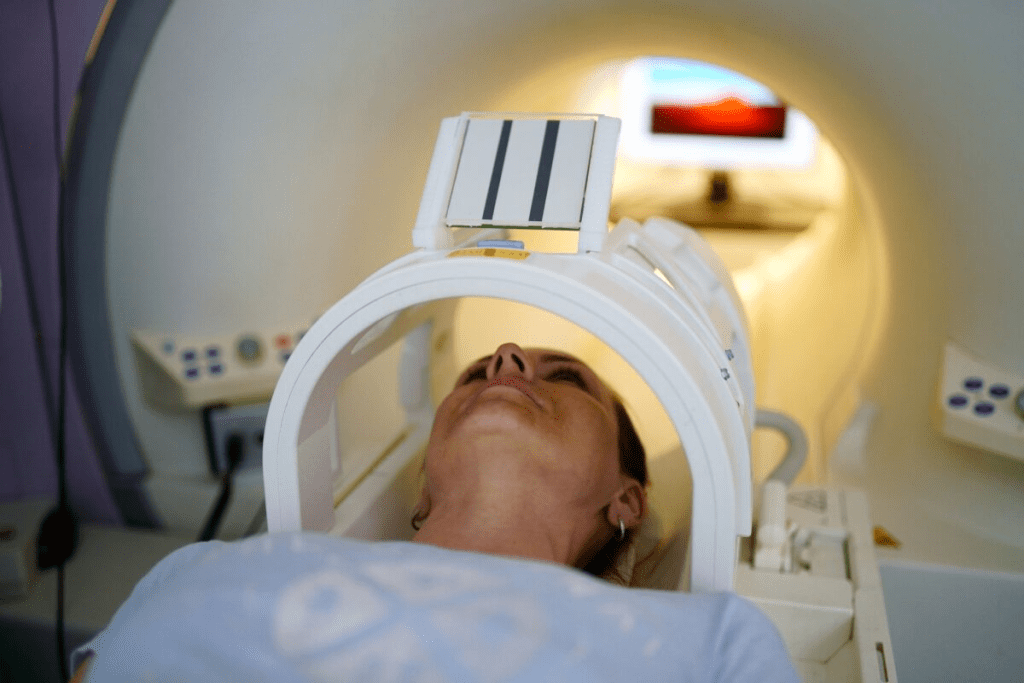
The Basics of MRI Technology
Understanding MRI technology is key to seeing how it helps diagnose autoimmune diseases. MRI, or Magnetic Resonance Imaging, is a top-notch tool in medicine. It uses strong magnetic fields and radio waves to show us what’s inside our bodies without surgery.
How MRI Works
MRI machines align hydrogen atoms in our bodies with a strong magnetic field. Then, radio waves disturb these atoms, sending signals to the MRI machine. These signals help create detailed images of our body’s inside parts.
This process is non-invasive and safe. It doesn’t use harmful radiation, making it good for many patients.
MRI scans are great for seeing soft tissue issues, like some autoimmune diseases. They help us see inflammation, damage, or other changes. This is key for figuring out what’s wrong and how to treat it.
Types of MRI Scans Relevant to Autoimmune Diseases
There are many MRI scans, each for different uses. Contrast-enhanced MRI uses a special agent to show certain body parts, like inflammation. This is helpful for diagnosing diseases like multiple sclerosis or neuropsychiatric lupus.
Other scans, like functional MRI (fMRI) and diffusion-weighted imaging, offer more details. They show brain activity and tissue changes. These advanced scans help doctors understand and manage autoimmune diseases better.
Autoimmune Disease Brain MRI: What Can It Reveal?
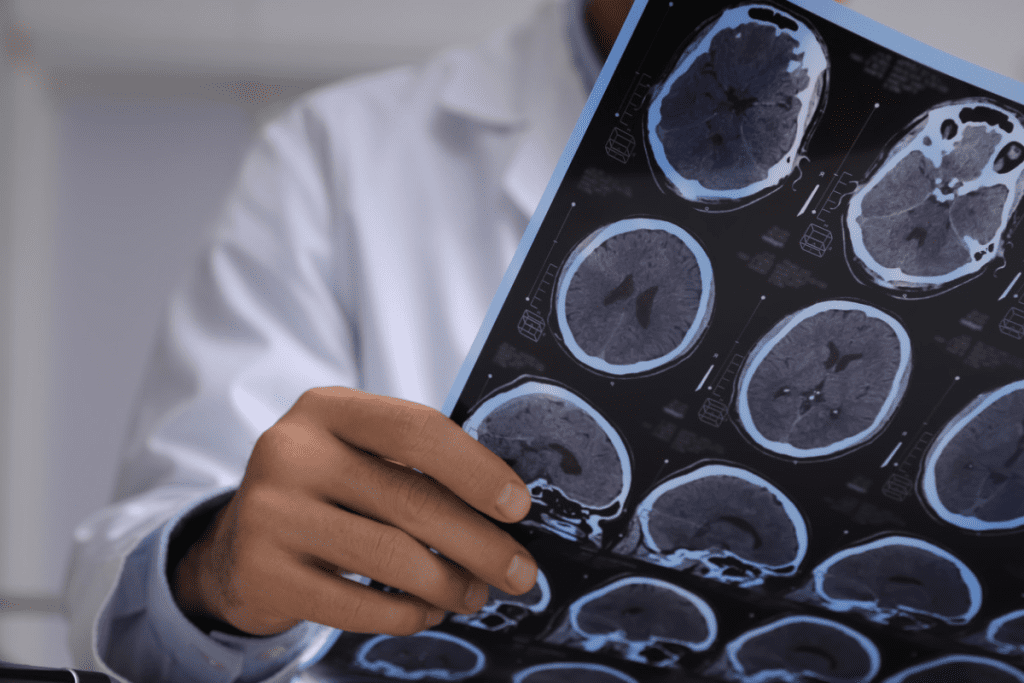
Brain MRI is a key tool for finding problems linked to autoimmune diseases. Conditions like multiple sclerosis, lupus, and rheumatoid arthritis can harm the brain. MRI scans show how these diseases affect the brain.
High-resolution imaging in brain MRI shows how much the brain is involved in autoimmune diseases. This info is key for diagnosing, planning treatment, and tracking how the disease changes over time.
Common Brain Abnormalities in Autoimmune Conditions
Autoimmune diseases can cause different brain problems that MRI can spot. Some common issues include:
- Lesions in the white matter, which can be a sign of multiple sclerosis
- Inflammation and swelling, seen in conditions like lupus
- Shrinkage of brain tissue, found in many autoimmune diseases
These problems can greatly affect a patient’s symptoms and life quality. For example, white matter lesions can cause thinking and movement problems.
| Autoimmune Condition | Common Brain MRI Findings |
| Multiple Sclerosis | White matter lesions, periventricular lesions |
| Lupus | Inflammation, edema, white matter changes |
| Rheumatoid Arthritis | Occasional vasculitis, rare meningitis |
Interpreting Brain MRI Results in Autoimmune Contexts
Understanding brain MRI results in autoimmune diseases needs a deep knowledge of both the diseases and MRI findings. Doctors and radiologists must work together. They need to link MRI findings with symptoms and other test results.
When looking at MRI results, it’s important to think about the patient’s medical history, symptoms, and other test results. This approach helps accurately diagnose and manage brain-related autoimmune conditions.
By combining medical knowledge with advanced imaging like brain MRI, we can better understand autoimmune diseases. This helps us find more effective treatments.
How MRI Detects Inflammation in Autoimmune Diseases
MRI is great at finding inflammation, which is key in diagnosing and treating autoimmune diseases. These diseases cause inflammation in different parts of the body, like the brain, joints, and organs.
Visualizing Inflammatory Processes
MRI is very good at spotting inflammation in tissues. It shows how much inflammation there is and how it affects nearby tissues. This helps doctors understand how serious the disease is and what treatment to use.
Inflammation can cause swelling and other changes that MRI can see. These include edema, enhancement, and other signs of inflammation.
Edema, Enhancement, and Other Inflammatory Markers
Edema shows up as bright spots on MRI images, meaning there’s swelling. Enhancement, seen after contrast is added, points to active inflammation. Other signs, like changes in tissue or lesions, can also be seen.
| Inflammatory Marker | Description | MRI Finding |
| Edema | Swelling caused by excess fluid | Hyperintense on T2-weighted images |
| Enhancement | Areas of active inflammation | Visible after contrast agent administration |
| Lesions | Abnormal tissue areas | Varying appearances on different MRI sequences |
MRI finds these signs of inflammation, giving doctors important info for diagnosing and tracking autoimmune diseases. This info helps doctors decide on treatments and see if they’re working.
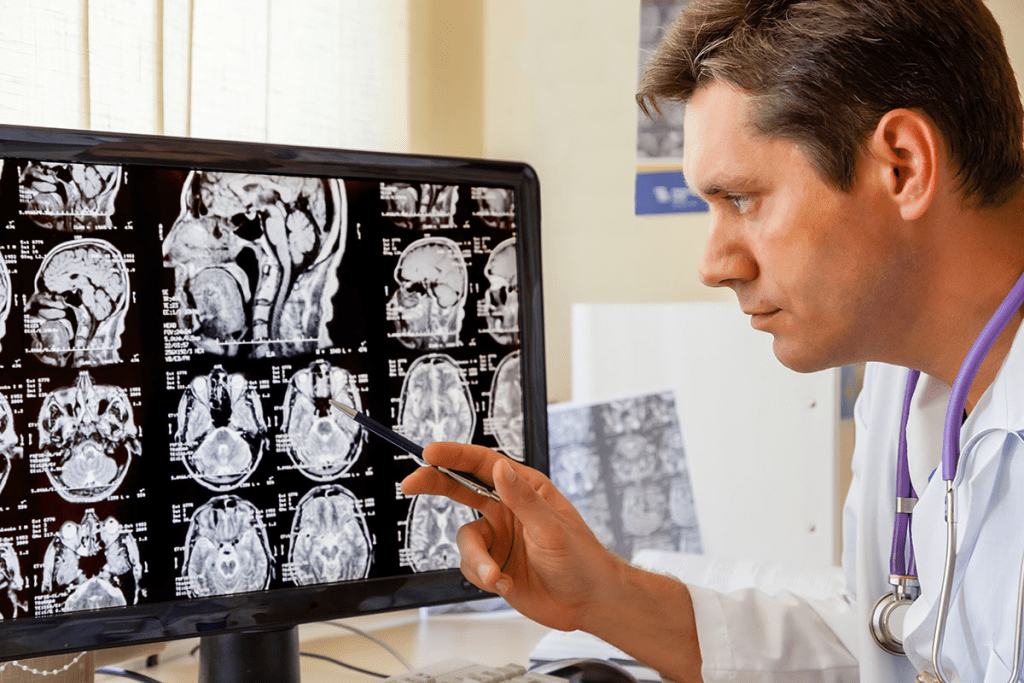
MRI for Multiple Sclerosis Diagnosis and Monitoring
Magnetic Resonance Imaging (MRI) has changed how we diagnose and track Multiple Sclerosis (MS). It gives us detailed views of the brain and spinal cord. This helps doctors spot the lesions that are a sign of MS.
Characteristic MS Lesions on MRI
MS lesions are key signs of the disease and show up on MRI scans. These lesions are damage spots in the central nervous system. They happen when the immune system attacks the nerve fibers’ protective covering.
On MRI, these lesions look like bright spots on T2-weighted images. They also appear as dark or enhanced spots on T1-weighted images after contrast material is used. Knowing about these lesions helps doctors diagnose MS and understand its severity.
McDonald Criteria and the Role of MRI
The McDonald criteria are guidelines for diagnosing MS. They include MRI findings to check for lesions in different parts of the CNS and over time. MRI is key in this process, showing lesions in various CNS areas and new ones over time.
“The integration of MRI into the McDonald criteria has significantly improved the accuracy and timeliness of MS diagnosis, enabling healthcare providers to initiate appropriate treatment earlier in the disease course.”
” A Neurologist
Monitoring Disease Progression with Serial MRIs
Serial MRI scans help track MS over time. By comparing scans, doctors can see new lesions and how active the disease is. This helps them decide if treatment needs to be changed.
We use MRI for both diagnosing and managing MS long-term. Regular MRI scans let us adjust treatments to fit each patient’s needs. This approach improves their quality of life.
Lupus and MRI: Detecting CNS Involvement
Systemic lupus erythematosus (SLE) is a complex autoimmune disease. It can affect the central nervous system (CNS) significantly. MRI plays a key role in detecting this involvement. Lupus can show up in many ways, making it hard to diagnose and manage its CNS effects.
We will look at how MRI helps spot CNS involvement in lupus patients. We’ll focus on neuropsychiatric lupus and how to tell lupus brain lesions from other conditions.
Neuropsychiatric Lupus on MRI
Neuropsychiatric lupus (NPSLE) includes neurological and psychiatric symptoms in lupus patients. MRI is a key tool for diagnosing and tracking NPSLE. Common MRI findings include:
- White matter lesions: These are damaged areas in the brain’s white matter. They appear as hyperintense lesions on T2-weighted images.
- Cerebral atrophy: Some NPSLE patients show signs of brain volume loss on MRI.
- Infarctions: MRI can spot infarctions or strokes caused by lupus-related vasculopathy or vasculitis.
A recent study noted that MRI findings in NPSLE can be non-specific. This makes clinical correlation key for accurate diagnosis.
“The role of MRI in NPSLE is not only to detect abnormalities but also to monitor disease activity and response to treatment.”
Differentiating Lupus Brain Lesions from Other Conditions
It can be tough to tell lupus brain lesions from other conditions because many MRI findings are non-specific. Yet, certain characteristics can help in making a more accurate diagnosis. For example:
- Lesion location and distribution: Lupus-related lesions often favor certain brain areas, which can be seen on MRI.
- Clinical correlation: It’s important to match MRI findings with clinical symptoms and lab results for diagnosing NPSLE.
- Serial MRI scans: Watching changes over time with serial MRI scans can help assess disease activity and treatment response.
We stress that a complete approach is needed for diagnosing and managing CNS involvement in lupus patients. This includes clinical evaluation, lab tests, and imaging studies like MRI.
Rheumatoid Arthritis: Joint Visualization Through MRI
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that affects the joints. MRI plays a crucial role in both diagnosing and managing rheumatoid arthritis. We’ll see how MRI helps spot joint inflammation early and track treatment success in RA patients.
Early Detection of Joint Inflammation
MRI is very good at finding early signs of joint inflammation in RA. It can spot synovitis and bone marrow edema. These signs are important for catching RA early, before it causes too much damage.
- Synovitis: Inflammation of the synovial membrane, seen on MRI as thickening and enhancement.
- Bone Marrow Edema: Areas of increased signal intensity on MRI, showing inflammation in the bone marrow.
Spotting these signs early means we can start treatment sooner. This can change the disease’s course and help patients better.
Monitoring Treatment Response in RA
MRI is not just for diagnosing; it also helps track how well treatments work. By watching how joint inflammation changes, doctors can tweak treatment plans as needed.
- Less synovitis and bone marrow edema means treatment is working well.
- If inflammation stays the same or gets worse, treatment might need to change.
Regular MRI scans give us important info on treatment success. This helps us make better decisions about future care.
MRI in Autoimmune Encephalitis Diagnosis
MRI is key in diagnosing autoimmune encephalitis. It gives detailed images that help doctors spot the condition. Autoimmune encephalitis happens when the immune system attacks the brain, causing inflammation and neurological symptoms.
Getting a diagnosis early is vital for good treatment and outcomes. MRI is a must-have tool in diagnosing this condition. It shows the brain’s structure and where inflammation might be.
Limbic Encephalitis Patterns
Limbic encephalitis mainly affects the limbic system, which handles emotions, behavior, and memory. On MRI, it shows changes in the temporal lobes, like the hippocampus and amygdala.
These changes include:
- T2-weighted hyperintensity, showing inflammation or swelling
- Contrast enhancement, meaning the blood-brain barrier is disrupted
- Atrophy or volume loss in affected areas over time
Spotting these patterns is key to diagnosing limbic encephalitis and differentiating it from other conditions.
Anti-NMDA Receptor Encephalitis Findings
Anti-NMDA receptor encephalitis is a form of autoimmune encephalitis. It’s marked by antibodies against NMDA receptors in the brain. MRI findings for this condition can be subtle but are essential for diagnosis.
Common MRI findings include:
| MRI Finding | Clinical Significance |
| T2-weighted hyperintensity in the cerebral cortex or hippocampi | Shows inflammation or neuronal damage |
| Mild meningeal enhancement | Indicates inflammation of the meninges |
| Normal or non-specific findings | Does not rule out the diagnosis; clinical correlation is essential |
A leading researcher, says, “Diagnosing anti-NMDA receptor encephalitis needs a mix of clinical assessment, serological testing, and imaging. MRI is key in identifying or ruling out other causes of encephalitis.”
“Diagnosing anti-NMDA receptor encephalitis is often tough because of its varied symptoms. But MRI, along with clinical evaluation and antibody testing, helps make an accurate diagnosis.”
We stress the importance of combining MRI findings with clinical presentation and other tests for accurate diagnosis and management of autoimmune encephalitis.
Spinal MRI in Autoimmune Disorders
Spinal MRI has changed neurology by giving clear views of the spinal cord. It’s key for spotting and tracking autoimmune diseases that hit the spine. This tool helps doctors see the spinal cord and the areas around it.
Transverse Myelitis and Neuromyelitis Optica
Transverse myelitis is an inflammatory disease that messes with the spinal cord. It causes pain, weakness, and numbness. Neuromyelitis optica, or Devic’s disease, mainly attacks the optic nerve and spinal cord. Spinal MRI is essential for spotting these conditions by showing inflammation.
It shows how much inflammation and damage there is in the spinal cord. This helps doctors tell these conditions apart from other spinal issues.
Spinal Manifestations of Multiple Sclerosis
Multiple sclerosis (MS) is a chronic disease that can hit the spinal cord. Spinal MRI helps find MS lesions in the spinal cord. These are common in the disease.
MS lesions in the spinal cord show up as bright spots on T2-weighted images. These spots might not cause symptoms or might lead to neurological problems.
“The ability to visualize the spinal cord in detail has significantly improved our understanding of autoimmune disorders affecting the spine,” said a leading neurologist.
| Condition | Typical MRI Findings | Clinical Symptoms |
| Transverse Myelitis | Inflammatory lesions, swelling | Pain, weakness, numbness |
| Neuromyelitis Optica | Longitudinally extensive lesions | Vision loss, weakness, bladder dysfunction |
| Multiple Sclerosis | Hyperintense lesions on T2-weighted images | Variable, including weakness, numbness, vision problems |
We’ve talked about how spinal MRI helps with diagnosing and tracking autoimmune diseases. This includes transverse myelitis, neuromyelitis optica, and multiple sclerosis. It gives doctors clear images of the spinal cord, helping them make accurate diagnoses and track how the disease is progressing.
Whole-Body MRI for Systemic Autoimmune Diseases
Whole-body MRI has changed how we look at systemic autoimmune diseases. It lets us see the whole body, giving us deep insights into these conditions. This helps us understand how severe they are.
Applications in Vasculitis and Connective Tissue Diseases
Whole-body MRI is great for spotting vasculitis, a blood vessel inflammation. It’s also good for diseases like lupus and rheumatoid arthritis. It shows how far these diseases have spread.
Vasculitis is hard to image because it affects many parts of the body. Whole-body MRI shows where the inflammation is. This helps doctors plan better treatments.
In connective tissue diseases, MRI helps see how the disease affects different parts. This is key for making good treatment plans.
Benefits of a Whole-Body Approach
Whole-body MRI has many advantages:
- It finds disease early
- It shows how bad the disease is
- It tracks how the disease changes over time
- It helps doctors choose the right treatments
Using whole-body MRI, doctors can understand systemic autoimmune diseases better. This leads to better care for patients.
Contrast vs. Non-Contrast MRI for Autoimmune Conditions
Autoimmune diseases are hard to diagnose. The choice between contrast and non-contrast MRI is key. MRI technology gives detailed images of the body’s inside.
Choosing to use contrast agents in MRI scans depends on several factors. These include the type of autoimmune disease and the information needed by healthcare providers.
When Contrast Agents Are Necessary
Contrast agents make certain features on MRI scans more visible. In autoimmune diseases, they help spot inflammation, damage, or disease activity better than non-contrast MRI.
In conditions like Multiple Sclerosis (MS), contrast agents show active brain and spinal cord lesions. This is vital for diagnosis and treatment planning. In autoimmune encephalitis, they reveal inflammation and neuronal damage.
Safety Considerations for Contrast Use
While contrast agents improve MRI scans, their use must be thoughtfully considered. The main concern is the risk of allergic reactions, though rare.
Another worry is the effect on kidney function, mainly in those with pre-existing kidney disease. Gadolinium-based contrast agents can cause Nephrogenic Systemic Fibrosis (NSF) in severe kidney cases.
We must balance the benefits of contrast agents against these risks. This means choosing patients carefully, considering other diagnostic methods, and following safe administration guidelines.
Limitations of MRI in Autoimmune Disease Detection
Using MRI to find autoimmune diseases has its limits. It’s important for doctors and patients to know this. MRI has changed how we diagnose diseases, but it faces challenges in autoimmune cases.
False Negatives and False Positives
When MRI is used to find autoimmune diseases, false results are a big issue. A false negative result can mean a patient gets treatment too late. This can make their condition worse. On the other hand, false positives can cause worry and lead to more tests that might not be needed.
False results happen for many reasons. These include how good the MRI is, the disease’s stage, and other health issues. These can hide or look like autoimmune changes on MRI.
Conditions That May Be Missed by MRI
Some autoimmune diseases are hard to see on MRI scans. This could be because of the disease itself or MRI’s limits. Early stages of some diseases might not show up on MRI. It’s key to understand these limits when looking at MRI results.
Accuracy and Reliability Considerations
How well MRI works to find autoimmune diseases depends on several things. These include the MRI machine’s quality, the radiologist’s skill, and the scan’s protocol. Making sure MRI scans are done and read well is vital for their usefulness.
Also, combining MRI results with other tests and the doctor’s evaluation is important. This way, we get a full picture of the patient’s health. This approach helps overcome MRI’s limits and improves diagnosis.
MRI vs. Other Diagnostic Methods for Autoimmune Diseases
MRI is a powerful tool for diagnosing autoimmune diseases. But, it’s not the only method used. Blood tests, CT scans, PET scans, and clinical evaluation also play key roles in diagnosing and managing these complex conditions.
Blood Tests and Biomarkers
Blood tests are often the first step in diagnosing autoimmune diseases. They detect specific antibodies and biomarkers linked to various conditions. For example, tests for antinuclear antibodies (ANA) help diagnose systemic lupus erythematosus (SLE).
While MRI gives detailed images of internal structures, blood tests show the body’s immune response. Together, they offer a deeper understanding of the disease.
| Diagnostic Method | Primary Use | Advantages |
| MRI | Detailed imaging of internal structures | High-resolution images, non-invasive |
| Blood Tests | Detecting antibodies and biomarkers | Early detection, monitoring disease activity |
| CT Scans | Quick imaging, for emergencies | Fast, widely available |
CT Scans and X-rays
CT scans and X-rays are great for checking structural damage and complications from autoimmune diseases. For instance, X-rays can show joint damage in rheumatoid arthritis. CT scans give detailed images of internal organs.
But, these methods use radiation, making them less ideal for frequent use. MRI, being radiation-free, is safer for long-term monitoring.
PET Scans and Nuclear Medicine
PET scans show metabolic activities in the body, helping spot inflammation or disease activity. They’re very useful in diagnosing and monitoring vasculitis.
While PET scans give functional info, they lack MRI’s anatomical detail. Using PET-MRI combines both, improving diagnostic accuracy.
Clinical Evaluation and Its Importance
Clinical evaluation is key in diagnosing autoimmune diseases. Healthcare providers look at symptoms, medical history, and physical exams to guide further testing.
No single method is perfect. A mix of clinical evaluation, lab tests, and imaging like MRI gives the most accurate diagnosis and treatment plan.
Conclusion: The Future of MRI in Autoimmune Disease Diagnosis
MRI will remain key in diagnosing autoimmune diseases. New MRI tech will help doctors spot and track these conditions better. This means better care for patients.
Research is pushing MRI to new heights. It aims to make images clearer, scans faster, and spot inflammation better. These changes will help find diseases sooner and more accurately. This is great news for patients.
As MRI tech gets better, so will our ability to manage autoimmune diseases. MRI will play a bigger role in diagnosing and tracking diseases like multiple sclerosis and lupus. This will lead to better treatments and a better life for those affected.
FAQ
Can MRI detect autoimmune diseases?
Yes, MRI can spot autoimmune diseases. It shows inflammation and tissue damage.
How does MRI help in diagnosing autoimmune diseases?
MRI gives detailed images of affected tissues. This helps doctors spot specific patterns and abnormalities.
What autoimmune diseases can be detected using MRI?
MRI can find and track many autoimmune diseases. This includes multiple sclerosis, lupus, and rheumatoid arthritis.
What are the characteristic MRI findings in multiple sclerosis?
MRI shows lesions in the brain and spinal cord. These appear as high signal intensity on T2-weighted images.
Can MRI detect inflammation in autoimmune diseases?
Yes, MRI can spot inflammation. It looks for signs like edema and enhancement in affected tissues.
How is MRI used in diagnosing lupus?
MRI helps find CNS involvement in lupus. It looks for brain lesions and abnormalities.
What is the role of MRI in rheumatoid arthritis diagnosis?
MRI is key in diagnosing rheumatoid arthritis. It shows joint inflammation, helping track the disease.
Can MRI detect autoimmune encephalitis?
Yes, MRI can find autoimmune encephalitis. It spots patterns like limbic encephalitis in the brain.
What are the benefits of whole-body MRI in assessing systemic autoimmune diseases?
Whole-body MRI offers a full-body view. It helps doctors see disease extent in different body parts.
When are contrast agents necessary in MRI for autoimmune conditions?
Contrast agents are needed for detailed MRI views. They help see inflammation and tissue damage clearly.
What are the limitations of MRI in detecting autoimmune diseases?
MRI might miss some conditions. It can also have false positives and negatives. This means doctors must carefully review MRI results.
How does MRI compare to other diagnostic methods for autoimmune diseases?
MRI is a valuable tool. It works with blood tests and CT scans to give a full picture of autoimmune diseases.
Can MRI rule out autoimmune disease?
MRI is very helpful but can’t always rule out autoimmune disease. Some conditions might not show up on MRI.
What is the future of MRI in autoimmune disease diagnosis?
MRI’s role in diagnosing autoimmune diseases is growing. New MRI tech will help doctors better manage these complex conditions.
References
- National Center for Biotechnology Information. (2010). The role of magnetic resonance imaging in autoimmune disease: Diagnostic and monitoring applications. Journal of Autoimmunity, 35(3), 227“239.