Last Updated on December 3, 2025 by Bilal Hasdemir
Nearly 1 in 5 people who have spinal surgery might feel regret, studies show.

This fact shows how key it is to know about patient satisfaction. It’s also important to understand what leads to regret after surgical procedures.What is the back surgery regret rate? We reveal the shocking truth. Discover if most people regret it.
More people are choosing surgery, so we need to look closely at decisional regret. We must see how it affects how well patients do after surgery.
Key Takeaways
- Decisional regret affects a significant portion of patients post-surgery.
- Understanding patient satisfaction is key to better outcomes.
- Regret can come from surgery problems and not meeting expectations.
- Teaching patients well can help reduce regret.
- Good care for patients can make them happier.
The Reality of Back Surgery Outcomes
Understanding back surgery outcomes means looking at both success rates and how happy patients are. Success is often measured by how well the surgery works. But happiness also includes how much pain is gone, how well you can move, and how good you feel overall.
Success Rates vs. Patient Expectations
Success in back surgery is usually about how well symptoms go away and how well you can move. But patients also hope for a better life, to do things they used to, and to have little pain left.
When what happens doesn’t match what patients hoped for, they might not be happy. For example, a surgery might work well but not get rid of all pain or limit movement, making the patient sad.
Defining “Successful” Back Surgery

What makes a back surgery successful can differ between doctors and patients. Doctors look at things like X-rays and how well nerves work. Patients judge success by how much pain is gone and how easy it is to do everyday things.
A successful surgery for a patient might not be the same as what a doctor sees. This shows why it’s important to talk clearly and set realistic hopes before surgery.
The Gap Between Clinical Success and Patient Satisfaction
There’s a big gap between how well surgeries work and how happy patients are. Even when surgeries are technically successful, some patients stay unhappy because their symptoms don’t go away or their hopes aren’t met.
To close this gap, we need to do more before surgery. This includes talking clearly about what to expect, setting realistic hopes, and thinking about the emotional and social sides of recovery.
Back Surgery Regret Rate: What the Data Shows
Looking at data on back surgery regret rates can give us important insights. Many people regret their back surgery. Knowing why this happens is key to making surgery better for everyone.
Current Statistics on Regret After Spine Surgery
Recent studies have shed light on how common regret is after spine surgery. A regret study found that 15% to 20% of patients regret their surgery. But, this number can change based on the surgery type and patient factors.
A regret survey showed that 25% of patients who had lumbar fusion surgery regretted their choice. This shows why we need to understand what causes regret to make patients happier.
How Regret Is Measured in Medical Studies
Medical studies use special scales to measure regret, like after back surgery. The Decision Regret Scale is one tool used to see how much regret patients feel after a medical choice.
The Decision Regret Scale Explained
The Decision Regret Scale is a tested questionnaire for measuring regret after medical decisions. It asks about satisfaction with the decision, the benefits, and any problems that came up.
| Scale Component | Description | Score Range |
| Overall Regret | General feeling about the decision | 1-5 |
| Perceived Benefits | Extent to which the decision was beneficial | 1-5 |
| Decision Satisfaction | Satisfaction with the choice made | 1-5 |
Understanding how regret is measured helps doctors talk to patients better. This can help lower regret rates after back surgery.
Statistical Overview: How Common Is Post-Surgical Regret?
It’s important to know how often people regret their back surgery. Studies have looked into this, giving us insights into what affects patient happiness.
Comprehensive Research Findings
Studies on regret after back surgery show mixed results. A detailed look at these studies shows that regret rates vary a lot. This depends on the surgery type and who is getting it.
For example, about 15% to 20% of people regret their lumbar fusion surgery. Those with degenerative conditions might feel more regret. This is because their conditions are complex, and surgery results can vary a lot.
Variation in Regret Percentages by Procedure Type
The type of surgery greatly affects how often people regret it. Each surgery has its own regret incidence rate. This shows how different surgeries can have different outcomes.
- Lumbar fusion surgery: 15% to 25% regret rate
- Discectomy: 10% to 15% regret rate
- Laminectomy: 12% to 20% regret rate
This means patients should know the risks and benefits of their surgery.
Comparing Satisfaction Rates Across Different Patient Demographics
Satisfaction rates after surgery can change based on who you are. For example, younger people tend to be happier than older ones. This might be because younger people are more likely to bounce back physically and have higher hopes.
| Demographic | Satisfaction Rate |
| Younger patients (< 50 years) | 80% |
| Older patients (≥ 50 years) | 60% |
Knowing these differences helps doctors and patients set better expectations. This can make everyone happier with their surgery results.
Types of Back Surgery and Associated Regret Rates
Back surgery regret rates vary widely depending on the specific procedure undertaken. Different surgical interventions for back pain have distinct outcomes and patient satisfaction levels.
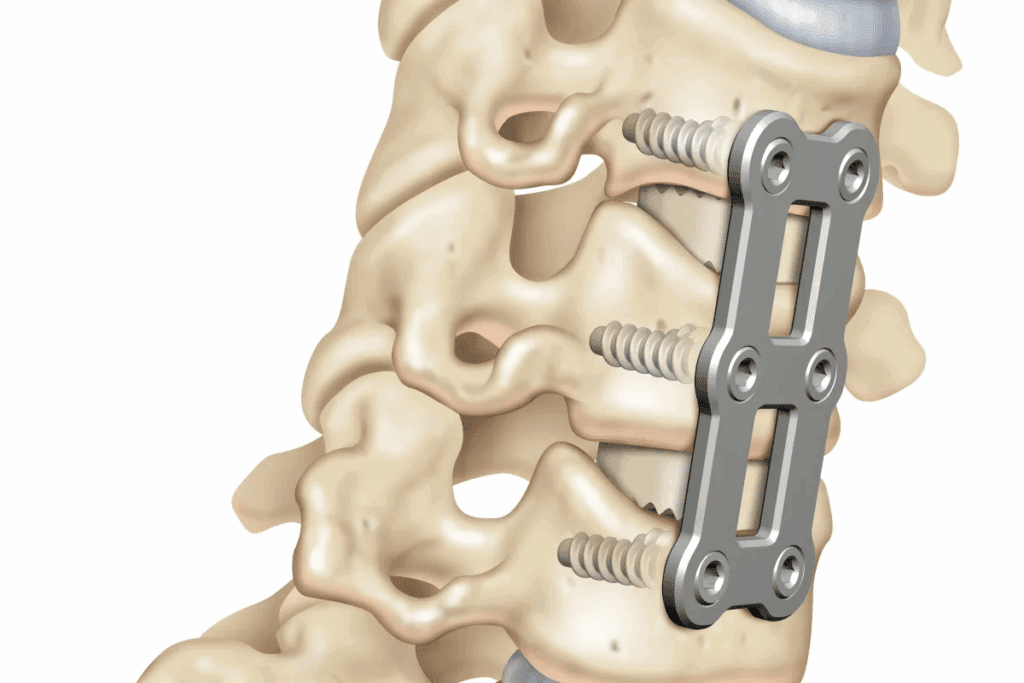
Lumbar Fusion Surgery Outcomes
Lumbar fusion surgery is a common procedure for treating chronic back pain. It’s used for degenerative disc disease, spondylolisthesis, or spinal stenosis. While it can be effective, lumbar surgery regret rates range from 8% to 40% depending on the study and patient population.
Discectomy Procedures and Patient Satisfaction
Discectomy is a surgical procedure to remove herniated disc material. It’s done when the disc is pressing on a nerve root or the spinal cord. Patient satisfaction rates after discectomy are generally high, with studies indicating a satisfaction rate of 70% to 90%.
Yet, a subset of patients may experience regret. This can be due to recurrent herniation, persistent symptoms, or adjacent segment disease. Research suggests that careful patient selection and thorough preoperative evaluation can minimize these risks.
Laminectomy Regret Incidence
Laminectomy involves removing part or all of the lamina to relieve pressure on the spinal cord or nerves. While generally effective for treating spinal stenosis, some patients may experience regret. This can be due to persistent pain or new-onset instability.
| Procedure | Regret Rate | Common Reasons for Regret |
| Laminectomy | 15%-30% | Persistent pain, new instability |
| Discectomy | 10%-20% | Recurrent herniation, persistent symptoms |
| Lumbar Fusion | 8%-40% | Persistent pain, limited functional improvement |
Spinal Deformity Correction and Long-term Satisfaction
Surgical correction of spinal deformities, such as adult scoliosis, can significantly improve quality of life. These complex procedures carry a higher risk of complications and potentially higher regret rates.
Studies on adult scoliosis regret indicate that while many patients experience significant improvement, some may regret their decision. This can be due to complications, persistent pain, or unmet expectations. Long-term satisfaction is influenced by factors such as the degree of deformity correction, postoperative care, and patient selection.
Primary Causes of Decisional Regret
It’s important to know why people might regret their back surgery. This knowledge helps both patients and doctors. Knowing the reasons can help lower the risks of surgery.
Unrealistic Expectations Before Surgery
Having unrealistic expectations is a big reason for regret. People often think surgery will fix all their problems. But, it’s key for doctors to set realistic expectations and explain what surgery can and can’t do.
Inadequate Preoperative Education and Counseling
Inadequate preoperative education can cause confusion. It’s important to talk to patients before surgery. This way, they know what to expect and can prepare for it.
Complications and Unexpected Side Effects
Complications and unexpected side effects can lead to regret. While some problems can’t be avoided, talking about risks beforehand helps. Common issues include infections, nerve damage, and problems with surgical tools.
- Infection
- Nerve damage
- Hardware failure
Persistent Pain Despite Intervention
Persistent pain is another reason for regret. If pain doesn’t go away, patients might feel the surgery was a failure. It’s important to remember that surgery doesn’t always stop pain. Health and other conditions can also affect results.
Understanding these causes helps doctors support their patients better. This way, patients can make informed choices and be happier with their surgery results.
Failed Back Surgery Syndrome: The Ultimate Regret
Failed Back Surgery Syndrome (FBSS) is a big worry for both patients and doctors. It’s a condition where back pain keeps coming back after surgery. This makes it the biggest regret for many.
Definition and Prevalence of FBSS
FBSS is not just one thing. It’s a mix of symptoms and problems after back surgery. How common it is depends on the surgery and the patient. About 10% to 40% of back surgery patients get FBSS.
Prevalence Rates of FBSS:
| Surgical Procedure | FBSS Prevalence |
| Lumbar Fusion | 20-30% |
| Discectomy | 15-25% |
| Laminectomy | 10-20% |
Relationship to Patient Regret and Dissatisfaction
FBSS often leads to patient regret and unhappiness after surgery. People with FBSS say they have less quality of life, ongoing pain, and can’t do much. This makes them feel frustrated, let down, and regretful of their surgery choice.
Management Options After Failed Surgery
Handling FBSS needs a team effort. This includes managing pain, physical therapy, and sometimes redoing the surgery. The right treatment depends on why FBSS happened and the patient’s health.
- Pain management through medication and interventional procedures
- Physical therapy to improve function and reduce pain
- Revision surgery in selected cases
Psychological Impact of Failed Procedures
The mental effects of FBSS can be huge. It can cause depression, anxiety, and lower patient happiness. It’s key to deal with these mental sides of FBSS.
Healthcare providers should take a full view of managing FBSS. They need to look at both the physical and mental sides of the condition.
Predictors of Postoperative Regret in Spine Surgery
Understanding what leads to regret after spine surgery is key. It helps manage what patients expect and boosts their happiness. Several things can make someone regret their surgery.
Demographic Risk Factors
Some demographic factors can affect regret after spine surgery. Age, gender, and how much money someone has are examples. Younger people might have different hopes for surgery than older ones.
| Demographic Factor | Influence on Regret |
| Age | Younger patients may have higher expectations. |
| Gender | Some studies suggest gender differences in satisfaction rates. |
| Socioeconomic Status | Access to post-operative care can vary. |
Psychological and Social Determinants
Psychological factors like preoperative anxiety and depression can greatly affect how happy a patient is. Also, having a strong support system is important for recovery and happiness.
Surgical Complexity and Technical Considerations
The complexity of the surgery and the surgeon’s skill can change the outcome. More complex surgeries might have more risks, which could lead to regret.
Pre-existing Conditions That Increase Regret Risk
People with chronic pain or who have had surgery before might regret their new surgery more. Knowing these risks helps manage what patients expect.
By understanding these predictors, doctors can give better advice. This can help lower the chance of regret after spine surgery.
The Impact of Complications on Regret Incidence
It’s important for surgeons and patients to understand how complications affect regret in spine surgery. Complications can happen during or after surgery. They can change how well a patient does and how happy they are with the surgery.
Common Complications in Spine Surgery
Like any surgery, spine surgery has risks. These can include infections, nerve damage, hardware failure, and ongoing pain. Infection can make recovery longer and might need more surgeries. Nerve damage can cause numbness, weakness, or pain that lasts.
| Complication | Description | Potential Impact on Patient |
| Infection | Bacterial infection at the surgical site | Prolonged recovery, additional surgeries, increased risk of further complications |
| Nerve Damage | Damage to nerves during surgery | Numbness, weakness, chronic pain, decreased quality of life |
| Hardware Failure | Failure of implanted hardware (e.g., rods, screws) | Need for revision surgery, potentially more pain or less mobility |
Direct Correlation Between Complications and Regret
Studies show that complications and regret are closely linked. When problems happen, patients often feel unhappy with their surgery. This unhappiness can come from not getting what they hoped for, more pain, or less ability to move.
Managing Expectations About Possible Complications
It’s key to manage what patients expect to avoid regret. Doctors and healthcare teams should talk a lot before surgery. They should explain what might go wrong and how likely it is.
By setting clear expectations, patients can better understand what might happen. This helps them make choices that are right for them.
Degenerative Spine Conditions and Regret Outcomes
It’s important to know about the regret that can come with spine problems. These issues include degenerative disc disease, spinal stenosis, adult scoliosis, and spondylolisthesis. Each one has its own challenges and things to consider when it comes to surgery.
Degenerative Disc Disease Surgery Satisfaction
Surgery for degenerative disc disease aims to ease pain and improve function. Patient satisfaction can vary. It depends on what the patient expected before surgery and if they have other health issues.
Many patients say they feel better after surgery. But, the results can change based on the surgery method used.
Spinal Stenosis Procedure Outcomes
Spinal stenosis surgery can greatly help those who have it. The success of the surgery is not just about feeling better. It’s also about what the patient says about their experience.
Research shows many patients see big improvements. But, some may not feel completely better.
Adult Scoliosis Surgical Regret Rates
Surgery for adult scoliosis is complex and comes with risks. Surgical regret rates depend on how complicated the surgery is, any complications after, and if the patient’s hopes were met.
While many patients are happy with their results, some may regret it. This can be due to ongoing pain or not meeting their expectations.
Spondylolisthesis Treatment Satisfaction
Treatment for spondylolisthesis depends on how bad it is and the patient’s symptoms. Patient satisfaction with surgery is usually high. This is when there’s a lot of pain relief and better function.
But, deciding to have surgery is a big choice. It’s about weighing the good against the bad.
In conclusion, the results of spine surgery are complex. They depend on many things like who gets surgery, how it’s done, and aftercare. Knowing these factors helps reduce regret and increase happiness for patients.
Revision Surgery: Second Chances or Deeper Regret?
Many patients see revision surgery as a second chance for back pain relief. But, deciding on more surgery is complex. It involves weighing the possible benefits against the risks.
Satisfaction Rates After Revision Procedures
Studies show that satisfaction after revision surgery varies a lot. Satisfaction depends on why the surgery was needed, the first surgery type, and the patient’s health. Some patients see big improvements, while others keep feeling pain or are unhappy.
Key factors affecting satisfaction rates include:
- The complexity of the initial procedure
- The presence of complications
- Patient selection criteria for revision surgery
Risk-Benefit Analysis of Additional Surgeries
Before deciding on revision surgery, a detailed risk-benefit analysis is key. It’s about comparing the chance for better results to the risks of complications, long recovery, or ongoing dissatisfaction. Patients and doctors must carefully consider these points to make smart choices.
Potential risks associated with revision surgery include:
- Infection or wound complications
- Nerve damage or neurological deficits
- Hardware failure or other mechanical issues
Decision-Making Framework for Revision Candidates
A clear decision-making framework is vital for those thinking about revision surgery. It involves looking at the patient’s medical history, why the first surgery didn’t work, and what the second surgery might achieve. It’s important for patients and doctors to make this decision together.
Considerations for revision candidates include:
- Understanding the goals and limitations of revision surgery
- Evaluating alternative treatment options
- Assessing psychological readiness for additional surgery
Patient Testimonials on Multiple Surgeries
Patient stories offer valuable insights into revision surgery experiences. While results vary, these accounts can inspire hope and help guide others facing similar choices.
“I underwent revision surgery after my initial procedure failed to alleviate my back pain. The second surgery was more successful, and I’m grateful for the relief I now experience.” – Patient testimonial
For some, revision surgery is a chance for a better life. But, it’s important to understand the risks and benefits clearly before making this choice.
Patient Satisfaction vs. Clinical Success: Bridging the Gap
Clinical success and patient satisfaction are two different things in spine surgery. Clinical success is about things like how well the surgery went and how well the patient is doing afterward. But patient satisfaction is about how the patient feels, like if their pain is better and if they’re happier with the surgery.
Disconnects Between Clinical Measures and Patient Experience
Many studies show that what doctors measure and what patients feel can be different. For example, a surgery might be a success by all medical standards but the patient might not feel better. This could be because of things like mental health or social issues.
Key factors contributing to this disconnect include:
- Preoperative expectations and their alignment with postoperative outcomes
- The presence of comorbidities or psychosocial factors that influence pain perception and quality of life
- The subjective nature of pain and its impact on patient-reported outcomes
Quality of Life Improvements Despite Technical Success
Improving a patient’s quality of life is very important. Even if a surgery is a technical success, how much better a patient feels can vary a lot. This depends on things like how sick the patient was before, any other health issues, and how well they can handle stress.
The Subjective Nature of Surgical Satisfaction
How happy a patient is after surgery is very personal. It depends on many things, like what the patient expected, their health before surgery, and how much support they get after. Doctors need to understand and deal with these things to make patients happier.
Effective strategies to enhance patient satisfaction include:
- Personalized preoperative counseling to manage expectations
- Comprehensive postoperative care and support
- Encouraging patient engagement in their recovery process
Minimizing Regret: The Surgeon’s Role
Surgeons play a key role in reducing regret after spine surgery. They need to be skilled technically and understand patient psychology and risks well.
Effective Patient Selection Criteria
Choosing the right patients is vital to avoid regret. Surgeons must look at medical history, psychological stability, and realistic expectations. This helps spot regret predictors and guide surgery decisions.
They should consider symptoms, health issues, and the patient’s overall health. It’s also important to check the patient’s motivation for surgery and their understanding of what might happen.
Comprehensive Preoperative Counseling Techniques
Good preoperative counseling is key to managing patient expectations and regret. Surgeons must clearly explain the risks and benefits of the surgery and other options.
This counseling should be personalized to each patient’s needs. It should cover possible complications, recovery time, and expected results. This way, patients can make informed decisions about their care.
Setting Realistic Expectations
It’s important to set realistic expectations to ensure patient satisfaction and reduce regret. Surgeons should work with patients to set clear goals and expectations. This should consider the patient’s individual circumstances and needs.
This approach helps patients know what to expect from the surgery. It reduces the chance of disappointment or dissatisfaction. It requires a deep understanding of spine surgery outcomes and clear communication with patients.
Follow-up Care and Long-term Support
Follow-up care and long-term support are essential to minimize regret after spine surgery. Surgeons must ensure patients get adequate follow-up care. This includes monitoring for complications and addressing concerns or questions.
By providing ongoing support, surgeons help patients through the recovery process. This involves a commitment to long-term care and addressing any issues that come up.
Minimizing Regret: The Patient’s Responsibility
When thinking about back surgery, patients have a big role. Being proactive and informed can greatly affect the outcome and satisfaction.
Thorough Research and Self-Education
One important step is to research your condition and the surgery. It’s key to know the risks, benefits, and alternatives to surgery.
- Understanding the surgical procedure and its implications
- Learning about possible complications and risks
- Exploring other treatments and their success rates
Seeking Second Opinions and Multiple Consultations
Getting a second opinion is vital. It helps confirm your diagnosis and understand treatment options. It also gives a wider view of your condition.
Talking to several specialists can give a full picture of your condition and treatments.
| Specialist | Role | Benefits of Consultation |
| Orthopedic Surgeon | Specializes in surgical treatments for musculoskeletal disorders | Provides detailed information on surgical options and outcomes |
| Neurosurgeon | Expert in surgical treatments for neurological conditions | Offers insights into the neurological aspects of back surgery |
| Physical Medicine and Rehabilitation Specialist | Focuses on non-surgical treatments and rehabilitation | Helps patients understand non-surgical alternatives and post-operative care |
Exploring Non-Surgical Alternatives First
It’s important to try non-surgical options first. This could be physical therapy, pain management, or lifestyle changes.
Preparing Mentally and Physically for Surgery
Getting ready for surgery means both mental and physical steps. Follow your surgeon’s advice on pre-operative care, like lifestyle changes or medications.
Mental readiness is also key. It can greatly affect your recovery and how happy you are with the surgery.
Decision-Making Tools to Prevent Surgical Regret
Patients thinking about back surgery can use decision-making tools to lower regret risk. These tools help people make smart choices about their care. They consider each person’s unique needs and situations.
Shared Decision-Making Models in Spine Care
Shared decision-making models are becoming more common in spine care. They help patients and doctors work together. This teamwork can lead to better patient satisfaction and less regret.
Risk Assessment Calculators and Predictive Tools
Risk calculators and predictive tools are great for patients thinking about spine surgery. They look at medical history and surgery complexity. They help guess how well the surgery might go.
| Tool | Description | Benefits |
| Risk Assessment Calculator | Estimates the risk of complications and decisional regret | Helps patients make informed decisions |
| Predictive Modeling | Forecasts possible spine surgery outcomes based on individual factors | Improves patient understanding and expectations |
Patient Decision Aids and Educational Resources
Patient decision aids and educational resources are key for informed choices. They give patients all the info they need about their options. This includes the good and bad sides of each choice.
- Detailed explanations of surgical procedures
- Information on possible complications and risks
- Testimonials from patients who have had similar surgeries
Questions to Ask Before Consenting to Surgery
Before agreeing to surgery, patients should ask important questions. This ensures they know what they’re getting into. Some key questions include:
- What are the possible benefits and risks of this surgery?
- What are the other options, and how do they compare?
- What are the expected spine surgery outcomes, and how will they be measured?
By using these tools and asking the right questions, patients can lower their chance of decisional regret. They can also be happier with their care choices.
Long-Term Outcomes and Evolution of Regret
Back surgery results can differ a lot for each patient. Many things affect these results, like the surgery type, patient health, and care after surgery. Knowing these outcomes helps manage hopes and boost patient satisfaction.
How Regret Changes Over Time Post-Surgery
Studies show that regret incidence can change after surgery. At first, some feel better and are happy with their choice. But, as time goes on, new problems or unresolved issues might change how they feel.
Things like ongoing pain, limited movement, or unexpected problems can make regret grow. But, good post-surgery care and support can help. This can make patients feel better in the long run.
Long-Term Satisfaction Studies (5+ Years)
Studies on patient satisfaction five years or more after surgery are very helpful. They show that some patients stay happy, but others might not. This can happen because of changes in their condition or other reasons.
Looking at these studies, it’s clear that ongoing care and setting realistic hopes are key. This helps understand how long the benefits of surgery last.
Factors That Improve Satisfaction Over Time
Several things can make patient satisfaction better over time. Good pain control, thorough rehab, and mental support are very important. These help make the recovery better.
- Personalized care plans tailored to individual patient needs
- Access to multidisciplinary support teams
- Ongoing education on managing expectations and adapting to new physical limitations
Adapting to New Physical Limitations
Getting used to new physical limits after surgery is key. Patients who adapt well usually feel happier. They can better handle their condition and keep a good life quality.
Ways to adapt include physical therapy, changing your lifestyle, and sometimes more medical help. This helps with any new problems.
Conclusion: Making Informed Decisions About Back Surgery
Back surgery is a big decision that comes with risks and outcomes. The rate of regret after back surgery is a major concern. Looking at the results of spine surgery and how happy patients are can help guide choices.
How happy a patient is can depend on many things. This includes the surgery type, what they hoped for before surgery, and how they recover after. Teaching patients a lot about their surgery can make them happier with the results.
Knowing the risks and benefits of back surgery helps patients set realistic goals. This way, they are more likely to be happy with the outcome. Healthcare teams focusing on the patient’s needs and making decisions together can reduce regret. This approach can also make patients more satisfied with their care.
FAQ
What is the overall regret rate for back surgery?
The regret rate for back surgery varies. Studies show that 10% to 30% of patients regret their decision to undergo back surgery. This depends on the surgery type and individual cases.
How is regret measured in medical studies related to back surgery?
Regret is measured with the Decision Regret Scale. This tool checks how much patients regret their surgery. It looks at satisfaction, expectations, and outcomes.
What are the most common causes of regret after back surgery?
Regret often comes from unrealistic expectations and not enough education before surgery. Complications and ongoing pain also play a big role. This shows why clear counseling and realistic goals are key.
How do different types of back surgery compare in terms of regret rates?
Different surgeries have different regret rates. For example, fusion surgery, discectomy, and laminectomy have their own rates. These rates are influenced by the surgery’s complexity and the patient’s background.
What is Failed Back Surgery Syndrome (FBSS), and how does it relate to regret?
FBSS is when patients keep feeling pain after surgery. This often leads to regret and dissatisfaction. Treatment options include more surgery, pain management, and psychological support.
Can complications during or after back surgery increase the likelihood of regret?
Yes, complications can greatly increase regret. They can cause unmet expectations, a long recovery, or more treatments. This is why it’s important to assess risks and educate patients well.
How can patients minimize the risk of regret after back surgery?
To lower regret risk, patients should research well, get second opinions, and consider non-surgical options. They should also prepare mentally and physically for surgery. Working closely with their doctors is also important.
What role do surgeons play in minimizing patient regret?
Surgeons are key in reducing regret. They should carefully choose patients, provide detailed counseling, and set clear expectations. They also need to offer ongoing care and support.
Are there decision-making tools available to help prevent surgical regret?
Yes, tools like shared decision-making models and patient decision aids can help. They help patients make informed choices and lower regret risk.
How do long-term outcomes influence regret after back surgery?
Long-term results greatly affect regret. Patients who see lasting benefits from surgery tend to regret less. Those with ongoing pain or complications may regret more over time.
What is the significance of patient satisfaction versus clinical success in back surgery?
Satisfaction and success are different. Satisfaction is how patients feel, while success is based on objective measures. It’s important to consider both to improve outcomes.
Can revision surgery improve outcomes and reduce regret?
Revision surgery can help some patients, improving their situation and reducing regret. But, it also comes with risks and uncertainties. It’s a decision that needs careful thought.
References
National Center for Biotechnology Information. Back surgery regret decisional considerations patient satisfaction. Retrieved from https://pubmed.ncbi.nlm.nih.gov/35412877/