
Living with osteogenesis imperfecta, also known as brittle bone disease, is tough. This genetic disorder makes bones very fragile. They can break easily, often without warning.
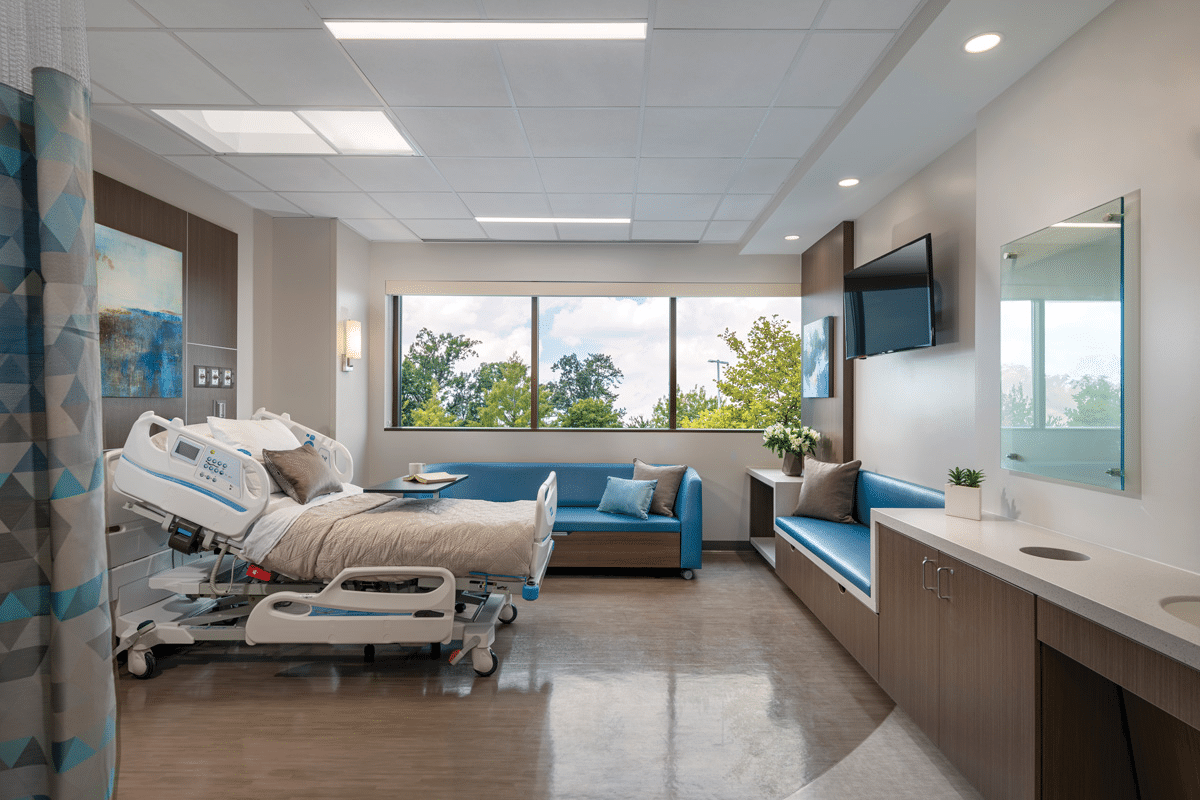
OI needs special care and understanding. At Liv Hospital, we offer top-notch healthcare for international patients. With 25,000-50,000 Americans affected, it’s key to spread the word about OI.
Key Takeaways
- Understanding osteogenesis imperfecta and its genetic causes
- Recognizing the symptoms and challenges associated with OI
- The importance of specialized care and support for individuals with OI
- Liv Hospital’s commitment to delivering world-class healthcare for OI patients
- Raising awareness about OI and its impact on individuals and families
What Is Osteogenesis Imperfecta: Understanding the Bone Breaking Disease
Osteogenesis Imperfecta is a complex genetic disorder that affects bone strength and fragility. It is also known as brittle bone disease or glass bone disease. This condition has drawn a lot of medical interest because of its impact on patients’ lives.
Definition and Overview of Brittle Bone Disease
Bones in people with Osteogenesis Imperfecta are extremely fragile and easily break. This happens because of a problem with the gene that makes type I collagen, a key protein for bones. The severity of OI can vary a lot, from mild to severe.
Historical Background: From Vrolik to Lobstein Syndrome
The history of OI goes back to Vrolik and Lobstein’s work. Vrolik first described the condition’s severity, mainly in infants. Lobstein later explained its effects in children and adults. Their findings helped us understand OI today, with Vrolik syndrome for the severe form and Lobstein syndrome for the milder form.
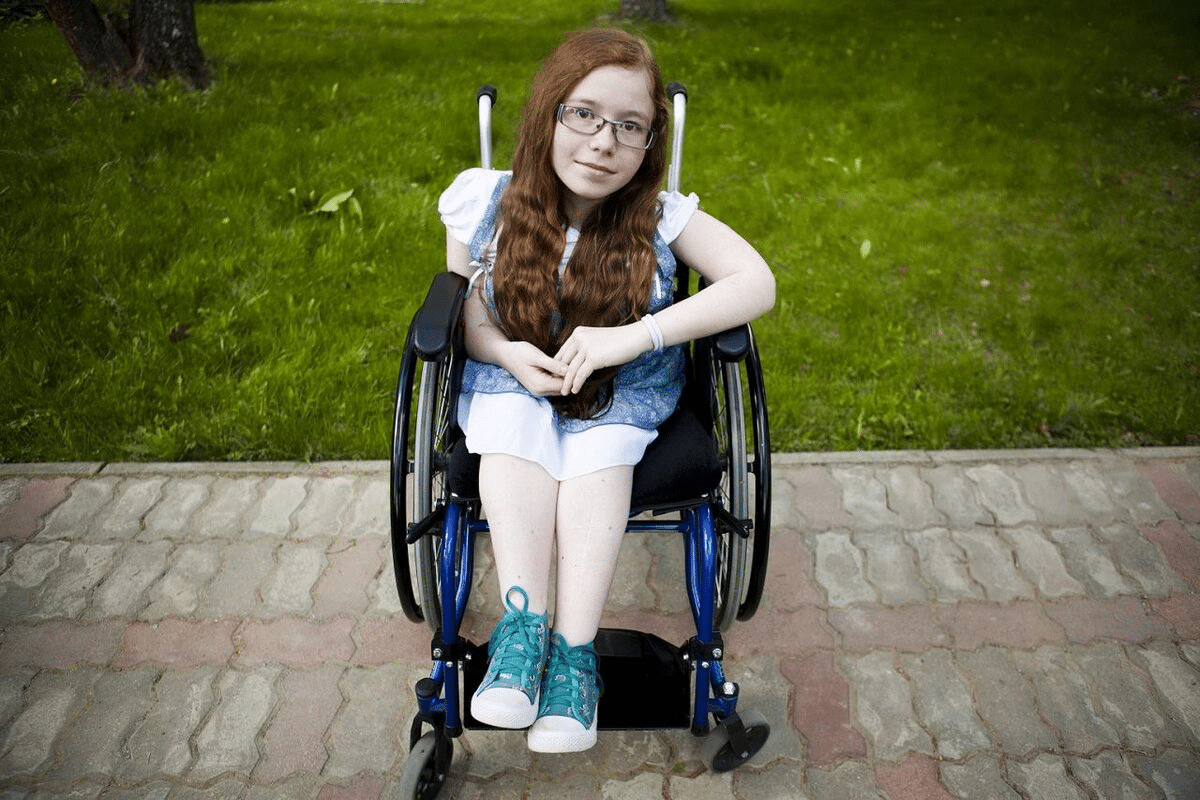
The Impact of OI on Daily Life
OI greatly affects the daily lives of those who have it. It causes physical challenges like frequent fractures. It also leads to emotional and social challenges. Simple tasks can be hard because of the risk of bone fractures. People with OI often need ongoing medical care and support to manage their condition.
Fact 1: The Genetic Foundations of Glass Bone Disease
Understanding the genetic roots of Osteogenesis Imperfecta is key. This condition, also known as Brittle Bone Disease, stems from genetic flaws. These flaws affect the production of type I collagen, a vital protein for bone strength.
Type I Collagen Defects: The Root Cause
Type I collagen is essential for bone health, giving bones strength and flexibility. Problems with the genes for type I collagen, COL1A1 and COL1A2, lead to weak bones. This makes bones more likely to break.
The role of type I collagen in bone health is huge. It’s made of two alpha-1 chains and one alpha-2 chain, forming a strong structure. But, mutations in these genes can mess up collagen, causing OI symptoms.
Inheritance Patterns of Osteogenesis Imperfecta
Osteogenesis Imperfecta can be passed down in different ways, mainly autosomal dominant. This means one mutated gene can cause the condition. In some severe cases, it’s autosomal recessive, needing two mutated genes to show symptoms.
|
Inheritance Pattern |
Description |
Implications |
|---|---|---|
|
Autosomal Dominant |
One mutated gene copy is sufficient to cause OI |
Each child of an affected parent has a 50% chance of inheriting the mutated gene |
|
Autosomal Recessive |
Two mutated gene copies are required to cause OI |
Carriers have a 25% chance of having an affected child with each pregnancy |
Genetic Mutations Associated with OI
There are many genetic mutations linked to Osteogenesis Imperfecta. These include point mutations, deletions, and duplications in COL1A1 and COL1A2 genes. The severity of OI can vary based on the mutation’s type and location.
Knowing these genetic mutations is vital for genetic counseling and family planning. Healthcare providers can help families understand the risk of passing on OI. This way, they can plan for future pregnancies and support affected family members.
Fact 2: Types and Classification of Brittle Bone Syndrome
Osteogenesis Imperfecta, or brittle bone syndrome, is not just one condition. It’s a range of disorders with different levels of bone fragility. Each type has its own set of symptoms and severity.
There are four main types of OI, each with its own set of features. Knowing these types is key for diagnosis and treatment.
Type I: Mild Osteogenesis Imperfecta
Type I OI is the mildest form. People with Type I OI might have mild bone fragility. They rarely break bones. They also often have blue or gray sclerae, a common sign of the condition.
Type II: Perinatal Lethal Form
Type II is the most severe and often fatal in the first few weeks of life. Babies with Type II OI have extremely fragile bones. They can break bones before or at birth. This type also often leads to breathing problems due to rib deformities.
Type III: Progressively Deforming
Type III OI is marked by bones that deform over time due to frequent fractures. People with Type III often have serious skeletal issues. This type is quite severe and can greatly affect their quality of life.
Type IV: Moderate OI
Type IV OI is in the middle in terms of severity. It has moderate bone fragility and varying degrees of skeletal deformity. Those with Type IV may face fractures, short stature, and dental issues.
By classifying OI into these types, doctors and researchers can better understand it. They can also predict outcomes and create treatment plans that fit each person’s needs.
- Type I: Mild OI with minimal bone fragility.
- Type II: Perinatal lethal form with extreme bone fragility.
- Type III: Progressively deforming with significant skeletal deformities.
- Type IV: Moderate OI with variable bone fragility and deformity.
Fact 3: Recognizing the Symptoms and Clinical Features
Osteogenesis Imperfecta (OI) shows different symptoms, affecting bones and other body systems. Knowing these symptoms is key for diagnosis and care.
Bone Fragility and Frequent Fractures
Bone fragility is a major sign of OI, causing many fractures. These breaks can happen with little trauma, sometimes without reason. We’ll look at how often fractures happen and where they usually occur in the next table.
|
Age Group |
Average Fractures per Year |
Common Fracture Sites |
|---|---|---|
|
0-5 years |
3-5 |
Long bones (femur, humerus) |
|
6-12 years |
2-4 |
Long bones, vertebrae |
|
13+ years |
1-3 |
Vertebrae, pelvis, long bones |
Blue or Gray Sclerae (Whites of the Eyes)
People with OI often have blue or gray sclerae. This means the whites of their eyes look colored because the scleral tissue is transparent. This is a big clue for doctors, but not all types of OI show it.
Growth Delays and Skeletal Deformities
Growth delays and skeletal deformities are common in OI, mainly in severe cases. These can include being shorter than usual, bowed limbs, and spinal problems like scoliosis. Early treatment with orthopedic care can greatly improve life quality.
Non-Skeletal Manifestations
But OI is more than just a bone problem. It can also cause hearing loss, dental issues (like dentinogenesis imperfecta), and heart problems in some. Taking care of these other issues is part of the treatment.
By knowing the many symptoms of Osteogenesis Imperfecta, doctors can create better treatment plans. This helps improve life quality for those affected.
Fact 4: Prevalence and Demographics of Brittle Bone Disease
Knowing about Osteogenesis Imperfecta’s prevalence and demographics is key. It helps healthcare providers and those with the condition. OI is a genetic disorder that makes bones very fragile. It affects many different groups of people.
Incidence Rates in the United States
In the U.S., about 1 in 15,000 to 1 in 20,000 babies are born with OI. This number changes because of how some cases are missed or not reported. It also changes because of the many different genes involved.
Research shows that OI doesn’t favor one gender over the other. It’s usually spotted in kids, but some milder cases might not be found until later.
Global Distribution of OI
Worldwide, OI is found in roughly the same number of people, about 1 in 15,000 to 1 in 20,000. This shows that OI is a genetic issue, not tied to any specific group.
A study in the Journal of Bone and Mineral Research found OI in every population studied. The same rate of occurrence in different countries points to its genetic roots.
Age and Gender Considerations
OI can happen to anyone at any age, but how it shows up can differ. Kids often get diagnosed because they break bones a lot and have blue-colored eyes.
Even though OI lasts a lifetime, there are ways to manage it. Knowing how common it is helps plan better care and services.
As we learn more about OI, it’s important to understand its prevalence and demographics. This knowledge is essential for giving the best care possible.
Fact 5: How Osteogenesis Imperfecta Is Diagnosed
Diagnosing Osteogenesis Imperfecta (OI) is a detailed process. It includes clinical evaluation, imaging studies, and genetic testing. This thorough approach is key to accurately identifying OI and differentiating it from other conditions.
Clinical Evaluation Process
The first step in diagnosing OI is the clinical evaluation. It involves a detailed medical history and physical exam. We look for signs like bone fractures, skeletal deformities, and blue or gray sclerae.
We also consider the patient’s family history. This helps us understand if other family members have OI or similar symptoms. This information is important for diagnosing the condition.
Imaging Studies and Their Importance
Imaging studies are vital in diagnosing OI. X-rays help us see bone density and detect fractures or deformities. DEXA scans may also be used to measure bone mineral density, which is often affected in OI.
In some cases, ultrasound or MRI may be used. They help us evaluate skeletal involvement or monitor disease progression.
Genetic Testing Methods
Genetic testing is a critical part of diagnosing OI. It looks for mutations in the genes that encode type I collagen (COL1A1 and COL1A2). These mutations are common in OI cases. We use DNA sequencing and mutation analysis to find these genetic changes.
In some cases, we may test for mutations in other genes associated with OI. This is important for individuals with atypical forms of the condition.
Prenatal Diagnosis Options
Prenatal diagnosis is available for families with a history of OI. Genetic testing can be done on fetal cells obtained through amniocentesis or CVS. This helps families prepare for the birth of a child with OI.
|
Diagnostic Method |
Description |
Application in OI Diagnosis |
|---|---|---|
|
Clinical Evaluation |
Thorough medical history and physical examination |
Identifies signs and symptoms of OI, assesses overall health |
|
Imaging Studies (X-rays, DEXA scans) |
Assesses bone density, detects fractures or deformities |
Essential for diagnosing OI, monitoring disease progression |
|
Genetic Testing |
Identifies mutations in COL1A1 and COL1A2 genes |
Confirms diagnosis, identifies genetic basis of OI |
|
Prenatal Diagnosis (Amniocentesis, CVS) |
Genetic testing on fetal cells |
Determines if fetus has inherited OI-causing mutation |
Treatment Approaches for Glass Bones Disease
Osteogenesis Imperfecta treatment includes many methods. These are medical management, surgery, and physical therapy. They aim to make life better for patients. The main goals are to reduce fractures, improve movement, and boost overall health.
Medical Management Strategies
Medical management is key in treating OI. It involves using medicines like bisphosphonates. These help make bones stronger and lower fracture risk. We watch for side effects and adjust treatments as needed.
- Bisphosphonates: These are the most used medicines for OI, helping bones get denser.
- Other medications: We might give extra medicines for issues like hearing loss or dental problems.
Surgical Interventions for Bone Strengthening
Surgery is very important in managing OI. It helps fix deformities and make bones more stable. We think about surgery when there are many fractures or big deformities.
- Rodding surgery: This involves putting metal rods in bones to support them and prevent fractures.
- Osteotomies: We do osteotomies to fix bone deformities and improve how bones line up.
Physical and Occupational Therapy Benefits
Physical and occupational therapy are vital in managing OI. They help patients move better and be more independent. We create special exercise plans for each patient.
- Physical therapy: This improves strength, flexibility, and movement with tailored exercises.
- Occupational therapy: We help patients learn daily skills and adapt to their surroundings to avoid injuries.
By using medical management, surgery, and physical therapy together, we can greatly enhance the lives of those with Osteogenesis Imperfecta.
Living with OI: Daily Challenges and Adaptations
Living with Osteogenesis Imperfecta (OI) brings daily challenges that need careful management. People with OI face physical limits, medical needs, and emotional hurdles. They must find ways to adapt and cope.
Home and Environmental Modifications
Adapting to OI often means changing one’s living space. Homes are made safer by removing hazards and installing handrails. These changes help prevent fractures and boost independence.
For example, someone with OI might rearrange furniture for easier movement. They might also use non-slip mats in bathrooms to avoid falls. These steps not only make spaces safer but also increase confidence in daily tasks.
Educational and Workplace Accommodations
Those with OI need special help in school and at work. This can include flexible scheduling and ergonomic furniture. Employers and schools can create environments that support productivity and well-being.
- Providing extra time to move between classes or to complete tasks
- Ensuring accessible facilities, such as ramps or elevators
- Allowing for regular breaks to rest and avoid fatigue
Psychological and Social Support
Living with OI affects mental health and social interactions. Psychological support from loved ones and counselors is key. Support groups offer a sense of community and understanding.
Social support networks help with the emotional side of OI. They provide a place to share experiences and advice.
Family Planning Considerations
For adults with OI, planning a family is a big decision. Genetic counseling helps understand the risk of passing OI to children. This knowledge aids in making informed family planning choices.
Pregnant individuals with OI need special prenatal care. This involves close monitoring and a team effort between obstetricians and OI specialists.
Research and Future Directions in Osteogenesis Imperfecta Treatment
Osteogenesis Imperfecta research is leading the way in medical breakthroughs. New treatments are coming. We’re learning more about the genetic and molecular causes of OI. This is changing how we treat and manage it.
Gene Therapy Developments
Gene therapy is a big hope for OI treatment. It aims to fix the genetic problems that cause OI. This could greatly improve life for those with the condition.
Stem Cell Research Progress
Stem cell research is also showing great promise. It could help grow stronger bones and reduce fractures. Scientists are looking into how stem cells can boost bone density.
Novel Pharmacological Approaches
New medicines are being made to strengthen bones and lower fracture risk. These treatments aim to lessen OI symptoms. Researchers are working hard to find even better solutions.
Improving Quality of Life: Emerging Technologies
New technologies like 3D printing and advanced orthotics are making life better for OI patients. They offer ways to create custom support devices and improve mobility.
|
Research Area |
Current Status |
Potential Impact |
|---|---|---|
|
Gene Therapy |
Preclinical trials |
Correcting genetic cause |
|
Stem Cell Research |
Clinical trials |
Bone regeneration |
|
Novel Pharmacological Approaches |
Phase II/III trials |
Improved bone density |
|
Emerging Technologies |
Varied, from conceptual to clinical use |
Enhanced quality of life |
As research keeps moving forward, we’ll see big changes in Osteogenesis Imperfecta treatment. The future looks bright for those with this condition.
Conclusion: Building Awareness and Support for Those with Brittle Bone Disease
Osteogenesis Imperfecta, or brittle bone disease, is a complex condition. It needs a deep understanding and support. Raising awareness about OI is key to helping those with it live fulfilling lives.
We’ve looked at the genetic roots, types, symptoms, diagnosis, and treatments for OI. A broad approach is needed to manage it well. By increasing awareness and support, we can make a better world for those with brittle bone disease.
Research into gene therapy, stem cells, and new medicines is promising. It could greatly improve life for those with OI. As we go forward, we must focus on awareness, education, and support for those with glass bone syndrome. They deserve the care and understanding they need.
FAQ
What is Osteogenesis Imperfecta (OI), also known as brittle bone disease?
Osteogenesis Imperfecta is a genetic disorder. It makes bones break easily, often without reason. It’s also called brittle bone disease.
What causes Osteogenesis Imperfecta?
OI is caused by problems with type I collagen. This protein is key for bone, skin, and teeth strength. These issues usually come from genetic mutations.
How is Osteogenesis Imperfecta inherited?
OI is usually passed down in an autosomal dominant way. This means one copy of the mutated gene causes the disorder. But, some cases come from random mutations.
What are the different types of Osteogenesis Imperfecta?
OI is divided into types based on symptoms and genetics. The main types are Type I (mild), Type II (fatal at birth), Type III (deforming), and Type IV (moderate).
What are the symptoms of Osteogenesis Imperfecta?
Symptoms include fragile bones and frequent fractures. People with OI also have blue or gray sclerae and growth delays. They might have skeletal deformities and other issues like hearing loss and dental problems.
How is Osteogenesis Imperfecta diagnosed?
Doctors use clinical evaluation, X-rays, and genetic testing to diagnose OI. They might also use prenatal ultrasound or genetic testing.
What are the treatment options for Osteogenesis Imperfecta?
Treatments include medications to prevent fractures and surgery to strengthen bones. Physical and occupational therapy help improve mobility and function.
How can individuals with Osteogenesis Imperfecta adapt to daily challenges?
People with OI can adapt by making home and environmental changes. They also need educational and workplace adjustments. Psychological and social support, along with careful family planning, are important.
What is the current state of research into Osteogenesis Imperfecta?
Research is exploring gene therapy, stem cell research, and new medicines. These studies aim to enhance the lives of those with OI.
What is the prevalence of Osteogenesis Imperfecta?
OI affects about 1 in 15,000 to 1 in 20,000 births. But, it might be underdiagnosed.
Are there any new treatments on the horizon for Osteogenesis Imperfecta?
Yes, new treatments like gene therapy, stem cell research, and medicines are being developed. They could improve life for those with OI.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK536957/






