When the body’s bone marrow not making red cells, it can cause many serious health problems. These include low hemoglobin and platelets, which lead to fatigue, weakness, easy bruising, and increased bleeding risk. Additionally, a reduced white blood cell count raises the risk of infections. At LivHospital, our expert team specializes in managing these complex bone marrow issues, offering advanced treatments such as blood transfusions, immunosuppressive therapies, and stem cell transplants to improve patient outcomes and quality of life.
Bone marrow failure happens when the marrow can’t make enough blood cells. This leads to several health issues. We will look at the 12 main reasons for this condition. This will help you understand why hemoglobin and platelets are low and the dangers involved.
Key Takeaways
- Understanding bone marrow failure is key to managing it well.
- Low hemoglobin and platelets can cause tiredness and more bleeding.
- Anemia with low white blood cells raises the risk of infections.
- LivHospital offers detailed care for complex blood disorders.
- Early diagnosis and treatment can greatly improve results.
Understanding Bone Marrow Function and Blood Cell Production

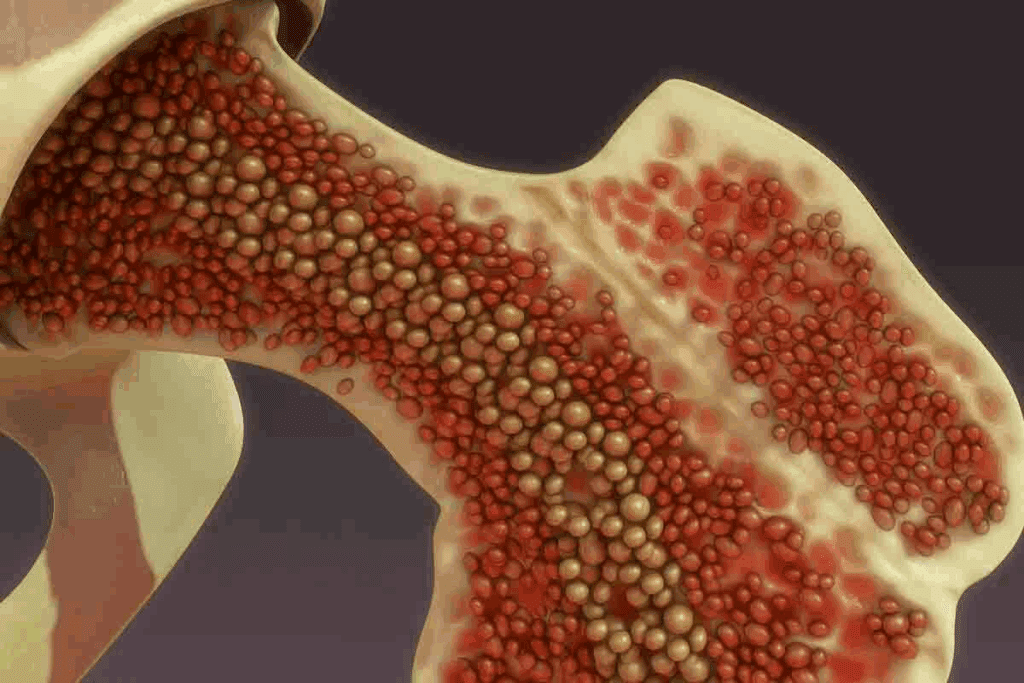
Bone marrow is key to making blood cells, which is vital for our health. It’s the spongy tissue inside bones like the hips and thighbones. It makes red cells, white cells, and platelets.
The Role of Bone Marrow in Blood Cell Formation
Bone marrow is vital for making blood cells. It has stem cells that turn into different blood cells. Each type of cell has its own job.
Normal Production of Red Cells, White Cells, and Platelets
Bone marrow makes red cells to carry oxygen, white cells to fight infections, and platelets for blood clotting. It produces these cells in the right amounts to keep us healthy.
The Relationship Between Hemoglobin, Platelets, and White Blood Cells
Hemoglobin in red cells is key for oxygen transport. Platelets help stop bleeding when we’re hurt. White cells fight off infections. Keeping these cells in balance is important for our health.
Recognizing the Symptoms of Bone Marrow Failure
It’s important to know the signs of bone marrow failure to get help quickly. This condition makes the body make fewer blood cells. This can lead to symptoms that affect many parts of your health.
Fatigue and Weakness from Low Hemoglobin
Fatigue and weakness are common signs of bone marrow failure. This is because of low hemoglobin levels. Hemoglobin carries oxygen to your body’s tissues and organs.
When hemoglobin is low, your body doesn’t get enough oxygen. This makes you feel tired and weak. You might also feel short of breath, dizzy, and have pale skin.
Low hemoglobin levels can make daily tasks hard. It’s important to get help if you notice these symptoms.
Increased Bleeding and Bruising from Low Platelets
Bone marrow failure can also cause easy bleeding and bruising. This is because of low platelet counts. Platelets help your blood clot.
With low platelets, you might bruise easily or bleed a lot from small cuts. You could also bleed from your gums or nose. This can be scary and needs quick medical help.
Patients might also have prolonged bleeding after injuries or spontaneous bleeding. This is a sign that you need to see a doctor right away.
Recurrent Infections from Low White Blood Cells
Low white blood cells make you more likely to get infections. White blood cells fight off germs. Without enough, you might get sick often.
Symptoms of infections include fever, chills, and swollen lymph nodes. In serious cases, these infections can be very dangerous. That’s why you need to see a doctor fast.
When to Seek Medical Attention
If you’re feeling tired, bleeding a lot, or getting sick often, see a doctor. Early treatment can really help if you have bone marrow failure.
If you or someone you know is feeling very tired, bleeding a lot, or keeps getting sick, go to a doctor. They can figure out what’s wrong and help you get better.
Aplastic Anemia: A Primary Cause of Bone Marrow Not Making Red Cells
Aplastic anemia is a serious disorder where the bone marrow can’t make enough blood cells. This is because the immune system attacks the bone marrow stem cells. As a result, there’s a drop in red blood cell production and other problems.
Mechanisms of Bone Marrow Failure in Aplastic Anemia
Aplastic anemia stops the bone marrow from making blood cells because of damaged stem cells. This damage can come from toxins, certain medicines, or autoimmune disorders. The immune system goes wrong, with T cells attacking the bone marrow stem cells. This stops blood cell production.
How Aplastic Anemia Affects All Blood Cell Lines
Aplastic anemia doesn’t just affect red blood cells. It also impacts white blood cells and platelets. A lack of red blood cells can cause anemia, leading to tiredness and weakness. Low white blood cell counts make infections more likely, and fewer platelets can cause bleeding and bruising.
Treatment Approaches for Aplastic Anemia
Treatment for aplastic anemia depends on how severe it is and the patient’s health. Immunosuppressive therapy is often used to stop the immune system from attacking the bone marrow. Sometimes, a bone marrow transplant is suggested, mainly for younger patients with a matching donor. Supportive care, like blood transfusions and antibiotics, is also key in managing the condition.
Dealing with aplastic anemia can be tough, but the right treatment can help many patients live active lives. It’s important to work closely with healthcare providers to find the best treatment plan.
Myelodysplastic Syndromes (MDS) and Impaired Blood Cell Production
MDS, or myelodysplastic syndromes, affect the bone marrow’s ability to make healthy blood cells. This leads to defective blood cells. These problems cause anemia, infections, and bleeding disorders.
Types of Myelodysplastic Syndromes
Myelodysplastic syndromes are divided into types based on the blood cells affected and the disorder’s genetics. The main types are:
- Refractory Anemia (RA)
- Refractory Anemia with Ringed Sideroblasts (RARS)
- Refractory Cytopenia with Multilineage Dysplasia (RCMD)
- Refractory Anemia with Excess Blasts (RAEB)
Each type has its own features and outlook.
How MDS Leads to Low Hemoglobin and Platelets
In MDS, the bone marrow can’t make enough healthy red blood cells and platelets. This is because of changes in the bone marrow cells. Patients often have anemia and low platelet count. This causes fatigue, weakness, and a higher risk of bleeding.
Prognosis and Management Options
The outlook for MDS patients varies. It depends on the type, age, and other health issues. Treatment options include supportive care, medications, and sometimes bone marrow transplantation.
| Prognostic Factor | Description | Impact on Prognosis |
| IPSS Score | International Prognostic Scoring System score based on blast percentage, karyotype, and number of cytopenias. | Higher scores indicate poorer prognosis. |
| Patient Age | Age of the patient at diagnosis. | Older age is associated with poorer prognosis. |
| Cytogenetic Abnormalities | Genetic abnormalities in bone marrow cells. | Certain abnormalities are associated with a worse prognosis. |
Knowing the prognosis and treatment options is key for MDS patients. It helps them make informed decisions about their care.
Inherited Bone Marrow Failure Syndromes
Inherited bone marrow failure syndromes are rare genetic disorders. They affect the body’s ability to make blood cells. These conditions lead to health problems because the bone marrow can’t make enough blood cells. We will look at Fanconi anemia and Diamond-Blackfan anemia, two key examples.
Fanconi Anemia: Mechanisms and Presentation
Fanconi anemia is a genetic disorder that affects blood cell production. It causes congenital abnormalities, bone marrow failure, and an increased risk of cancer. The problem lies in genes that help fix DNA, which is important for cell health.
People with Fanconi anemia often feel fatigue, infections, and bleeding. This is because they have low counts of red and white blood cells and platelets.
Diamond-Blackfan Anemia: Impact on Red Cell Production
Diamond-Blackfan anemia mainly affects red blood cell production. It leads to a significant reduction in red blood cell production, causing severe anemia. Symptoms include pallor, fatigue, and shortness of breath.
This condition is linked to mutations in genes that help make red blood cells. It is often diagnosed in infancy or early childhood.
Dyskeratosis Congenita and Shwachman-Diamond Syndrome
Dyskeratosis congenita and Shwachman-Diamond syndrome are also inherited bone marrow failure syndromes. Dyskeratosis congenita is known for oral leukoplakia, nail dystrophy, and reticulated skin hyperpigmentation. It also increases the risk of bone marrow failure and cancer.
Shwachman-Diamond syndrome affects the bone marrow, pancreas, and skeletal system. It leads to neutropenia, exocrine pancreatic insufficiency, and skeletal abnormalities.
“Understanding the genetic basis and clinical manifestations of these inherited syndromes is critical for proper care and management.”
In conclusion, inherited bone marrow failure syndromes are complex genetic disorders. They impact the body’s ability to produce blood cells. Conditions like Fanconi anemia, Diamond-Blackfan anemia, dyskeratosis congenita, and Shwachman-Diamond syndrome need careful management to address health challenges.
Autoimmune Disorders Affecting Bone Marrow Function
When the immune system goes wrong, it can harm the bone marrow’s job. This job is to make healthy blood cells. Autoimmune disorders happen when the body attacks itself. This can lead to fewer blood cells being made.
Pure Red Cell Aplasia: Selective Red Cell Production Failure
Pure red cell aplasia is a rare condition where the bone marrow can’t make enough red blood cells. This causes severe anemia. It can be caused by autoimmune diseases, infections, or certain medicines.
Treatment often involves finding and fixing the cause. It may also include medicines to calm down the immune system.
“The diagnosis of pure red cell aplasia requires a thorough examination of the bone marrow and ruling out other causes of anemia,” emphasizes the importance of accurate diagnosis in managing the condition.
Systemic Lupus Erythematosus and Bone Marrow Suppression
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease. It can harm many parts of the body, including the bone marrow. This can lead to fewer blood cells being made.
SLE can cause anemia, low white blood cell count, and low platelet count. To manage SLE, doctors try to calm down the immune system.
Treatment approaches for SLE may include corticosteroids, immunosuppressive drugs, and other medications aimed at controlling symptoms and preventing flare-ups.
Other Autoimmune Conditions Affecting Blood Cell Production
Other autoimmune conditions can also affect blood cell production. For example, autoimmune hemolytic anemia happens when the immune system attacks red blood cells. Immune thrombocytopenia is when the immune system destroys platelets.
- Autoimmune hemolytic anemia
- Immune thrombocytopenia
- Other autoimmune conditions that may affect blood cell production
It’s important to understand how autoimmune disorders and bone marrow function are connected. This helps doctors diagnose and treat these conditions better. By treating the autoimmune cause, doctors can help the bone marrow work right again.
Infections That Suppress Bone Marrow Activity
Certain infections can slow down bone marrow work. This affects how blood cells are made. It can cause anemia, make infections more likely, and lead to bleeding problems.
Viral Infections: Parvovirus B19, EBV, and CMV
Viral infections are a big reason for bone marrow slowdown. Parvovirus B19 attacks red blood cell makers in the bone marrow, causing anemia. Epstein-Barr Virus (EBV) and Cytomegalovirus (CMV) also harm bone marrow, reducing blood cell production.
These viruses can be very serious, mainly for people with weak immune systems. For example, parvovirus B19 can cause temporary aplastic crises in those with hemolytic diseases.
HIV and Its Effects on Bone Marrow Function
HIV (Human Immunodeficiency Virus) infection also slows down bone marrow. HIV directly attacks bone marrow cells, cutting down blood cell production. This can cause anemia, low white blood cell count, and low platelet count.
HIV’s impact on bone marrow is complex. It involves direct viral attacks and indirect effects through immune system problems.
Tuberculosis and Other Bacterial Infections
Bacterial infections, like tuberculosis (TB), can also harm bone marrow. TB can spread into the bone marrow, reducing blood cell making. Other bacterial infections can have similar effects by releasing inflammatory substances that slow down bone marrow.
| Infection | Effect on Bone Marrow | Consequences |
| Parvovirus B19 | Infects red blood cell precursors | Anemia, transient aplastic crises |
| HIV | Directly infects bone marrow cells | Anemia, leukopenia, thrombocytopenia |
| Tuberculosis | Infiltrates bone marrow | Suppression of blood cell production |
It’s important to understand how these infections affect bone marrow. This helps doctors diagnose and treat patients better. Early treatment can lessen the harm these infections do to bone marrow.
Medication and Toxin-Induced Bone Marrow Suppression
Medications and toxins can harm bone marrow, making it hard to produce blood cells. This serious issue can cause anemia, infections, and bleeding problems.
Chemotherapy Drugs and Their Impact on Blood Cells
Chemotherapy is a major cause of bone marrow suppression. These drugs attack fast-growing cells, like cancer and blood-making cells. This can lower the levels of red, white, and platelet cells.
Effects of Chemotherapy on Blood Cell Production:
- Red blood cells: Anemia, fatigue, and weakness
- White blood cells: Increased risk of infections
- Platelets: Bleeding and bruising
Antibiotics and Other Medications That Affect Bone Marrow
Some antibiotics and drugs can also harm bone marrow. For example, sulfonamides and anticonvulsants can lower blood cell production.
| Medication Class | Examples | Effect on Bone Marrow |
| Antibiotics | Sulfonamides, Chloramphenicol | Suppresses production of red and white blood cells |
| Anticonvulsants | Carbamazepine, Valproate | Can cause aplastic anemia |
| Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) | Ibuprofen, Indomethacin | Can affect platelet production |
Benzene, Radiation, and Other Environmental Toxins
Exposure to toxins like benzene and radiation can also harm bone marrow. Benzene is a carcinogen that can damage bone marrow, causing aplastic anemia and blood disorders.
Effects of Environmental Toxins on Bone Marrow:
- Benzene: Aplastic anemia, leukemia
- Radiation: Bone marrow failure, increased risk of cancer
- Pesticides and Heavy Metals: Various blood disorders
It’s important to know the risks of medications and toxins to prevent bone marrow suppression. Talk to your healthcare provider about any concerns to reduce risks.
Nutritional Deficiencies and Metabolic Causes
Metabolic causes and nutritional deficiencies can harm bone marrow. The bone marrow needs nutrients to work right. Without them, it can cause anemia, low platelet count, and weak immune system.
Vitamin B12 and Folate Deficiencies
Vitamin B12 and folate help make red blood cells. Not having enough can cause anemia. This makes you feel tired, weak, and short of breath.
Vitamin B12 deficiency can happen from not eating enough, not absorbing it well, or certain health issues. Folate deficiency can come from not eating enough, needing more, or not absorbing it well.
We will look closer at these deficiencies. The table below shows the main differences between Vitamin B12 and Folate deficiencies.
| Characteristics | Vitamin B12 Deficiency | Folate Deficiency |
| Causes | Dietary lack, malabsorption, medical conditions | Inadequate diet, increased requirement, malabsorption |
| Symptoms | Fatigue, weakness, neurological changes | Fatigue, weakness, diarrhea |
| Treatment | Vitamin B12 supplements, dietary changes | Folate supplements, dietary adjustments |
Iron Deficiency and Its Effect on Hemoglobin
Iron is key for making hemoglobin, which carries oxygen. Iron deficiency often causes anemia, more in women of childbearing age. It can come from not eating enough iron, losing blood, or needing more during pregnancy.
Iron deficiency anemia can make you very tired, affect work, and hurt your brain. To fix it, you need iron supplements and to eat more iron.
Copper Deficiency and Alcoholism
Copper helps make red blood cells. Copper deficiency can cause anemia and other blood problems. It’s rare but can happen in those who don’t absorb it well or eat too much zinc.
Drinking too much alcohol can lead to not getting enough nutrients, including copper. It can make it hard to absorb nutrients and lose them too.
We’ve seen how important nutrients are for bone marrow health. Eating right is key to keeping bone marrow working well.
Bone Marrow Infiltration and Replacement
Bone marrow issues can cause big problems with blood. When it’s filled with abnormal cells, it can’t make blood right. This happens in cancers and other diseases.
Leukemia and Bone Marrow Function
Leukemia is a blood and bone marrow cancer. It makes too many bad white blood cells. These cells fill the marrow and mess up normal blood making.
Acute leukemia needs quick treatment, like chemotherapy. Chronic leukemia moves slower, so there are more treatment choices.
Multiple Myeloma and Other Plasma Cell Disorders
Multiple myeloma is a cancer of plasma cells in the bone marrow. It makes bad plasma cells grow, causing bone damage and anemia. Other disorders like MGUS also affect the marrow.
- Symptoms include bone pain and fatigue.
- Treatment options range from medication to stem cell transplantation.
Metastatic Cancer to the Bone Marrow
Metastatic cancer spreads to the bone marrow from other cancers. It messes with marrow function, causing anemia and pain. Common cancers include breast, prostate, and lung.
Diagnosis uses bone marrow biopsy. Treatment depends on the cancer’s location and spread.
Myelofibrosis and Bone Marrow Scarring
Myelofibrosis scars the bone marrow. This scarring hurts blood cell making, causing anemia and low platelets. Symptoms vary, and treatment tries to ease them and improve life quality.
| Condition | Effect on Bone Marrow | Common Symptoms |
| Leukemia | Infiltration by abnormal white blood cells | Fatigue, infections, bleeding |
| Multiple Myeloma | Proliferation of malignant plasma cells | Bone pain, fatigue, infections |
| Myelofibrosis | Scarring of bone marrow | Anemia, fatigue, splenomegaly |
Conclusion: Diagnosis, Treatment, and Living with Bone Marrow Disorders
It’s important to understand bone marrow disorders to manage them well. Doctors use tests like complete blood count and reticulocyte count to find the cause. These tests help see how blood cell production is affected.
When someone is diagnosed, treatment depends on the disorder. Hematopoietic stem cell transplantation and immunosuppressive therapy are common treatments. These are often used for conditions like aplastic anemia.
Living with these disorders needs a lot of care and support. Patients must stay in close touch with their doctors. This helps manage symptoms, avoid complications, and improve life quality.
FAQ
What are the main functions of the bone marrow in blood cell production?
The bone marrow makes red blood cells, white blood cells, and platelets. These are key for carrying oxygen, fighting infections, and stopping bleeding.
What is bone marrow failure, and how does it affect the body?
Bone marrow failure means the marrow can’t make enough blood cells. This leads to tiredness, more bleeding, and frequent infections.
What are the symptoms of low hemoglobin, low platelets, and low white blood cells?
Symptoms include feeling tired and weak, more bleeding and bruising, and getting sick often.
What is aplastic anemia, and how does it affect blood cell production?
Aplastic anemia is when the bone marrow can’t make blood cells. It affects all types of blood cells, including red, white, and platelets.
How do myelodysplastic syndromes (MDS) impact blood cell production?
MDS are disorders that make it hard for the bone marrow to produce healthy blood cells. This leads to low hemoglobin and platelets.
What are inherited bone marrow failure syndromes, and how do they affect blood cell production?
Inherited bone marrow failure syndromes, like Fanconi anemia and Diamond-Blackfan anemia, are genetic. They affect the bone marrow’s ability to make blood cells.
Can autoimmune disorders affect bone marrow function, and if so, how?
Yes, autoimmune disorders can harm bone marrow function. This includes conditions like pure red cell aplasia and systemic lupus erythematosus, leading to poor blood cell production.
How do infections, such as viral and bacterial infections, impact bone marrow activity?
Some infections, like parvovirus B19, EBV, and CMV, can slow down bone marrow activity. This results in fewer blood cells being made.
Can medications and toxins induce bone marrow suppression, and if so, how?
Yes, some drugs, like chemotherapy and antibiotics, and toxins, like benzene and radiation, can weaken the bone marrow.
What role do nutritional deficiencies play in bone marrow malfunction?
Lack of nutrients, such as vitamin B12 and folate, can harm the bone marrow. This leads to fewer blood cells being made.
How does bone marrow infiltration and replacement affect blood cell production?
Conditions like leukemia, multiple myeloma, and metastatic cancer can fill and replace the bone marrow. This makes it hard to produce blood cells.
What is the relationship between anemia, low white blood cell count, and bone marrow failure?
Anemia and low white blood cell count are signs of bone marrow failure. The marrow isn’t making enough blood cells.
Can anemia cause low white blood count, and vice versa?
Yes, some conditions, like bone marrow failure, can cause both anemia and low white blood count.
What is the impact of low hemoglobin and low platelets on overall health?
Low hemoglobin and platelets can make you tired, bleed more, and bruise easily. This affects your health and quality of life.
How are bone marrow disorders diagnosed and treated?
Doctors use medical history, physical exams, and lab tests to diagnose bone marrow disorders. Treatment depends on the condition and may include medicines, transfusions, or bone marrow transplants.
References
- Miano, M., & Dufour, C. (2020). The diagnosis and treatment of aplastic anemia: a review. International Journal of Hematology, *111*(1), 34-44. https://pubmed.ncbi.nlm.nih.gov/31720909/









