Last Updated on December 2, 2025 by Bilal Hasdemir
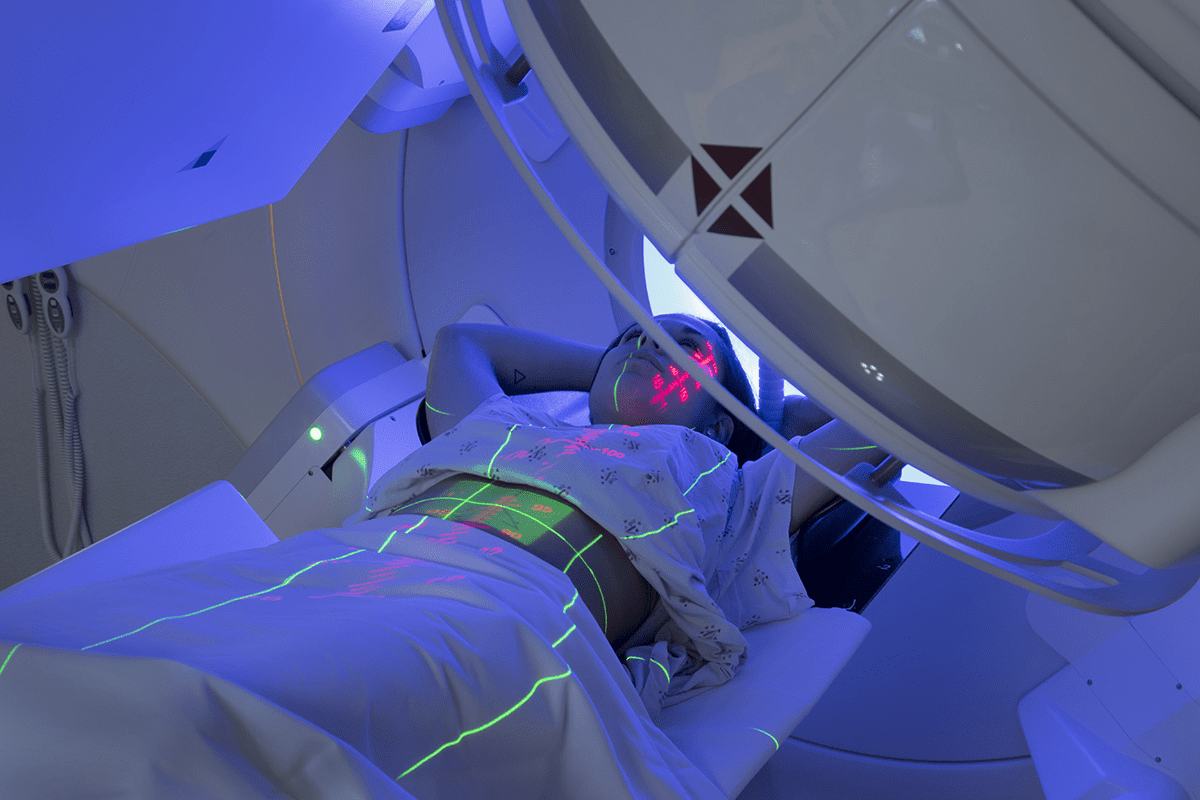
Awake brain surgery, or awake craniotomy, is a complex procedure. Patients stay awake during the surgery. This lets surgeons watch brain function in real-time. They can see how it affects speech and movement.
Did you know awake craniotomy needs special numbing methods? We use special anesthesia to numb the scalp and areas around the brain. This way, patients can stay awake and respond.
Our neurosurgical team keeps a close eye on patients’ vital signs and brain activity. They make sure the surgery goes well.
Key Takeaways
- Awake craniotomy is a complex neurosurgical procedure.
- Patients remain awake and responsive during the operation.
- Specialized numbing techniques are used for patient comfort.
- Real-time monitoring of brain function is critical.
- Our team ensures patient safety and successful outcomes.
Understanding Awake Brain Surgery
Awake brain surgery is a big step forward in neurosurgery. It lets surgeons work on the brain when the patient is awake. This method, also known as awake craniotomy, helps patients with brain tumors or lesions.
Being awake during surgery might seem scary. But, it’s key to keeping important brain functions safe during the surgery.
Definition and Purpose
Awake brain surgery means the patient is awake and can talk during parts of the surgery. The main goal is to remove brain tumors or lesions without harming brain functions. This includes speech, motor skills, and feeling.
Keeping the patient awake lets surgeons map the brain in real-time. This helps them avoid damaging important areas. It also makes the surgery safer and better for the patient.
Historical Development
The history of awake brain surgery goes back decades. But, recent years have seen big steps forward. Early tests with awake craniotomy helped create today’s methods for brain mapping and monitoring.
Advances in neurosurgery have been key. Better anesthesia, tools, and imaging tech have made these surgeries safer and more precise.
Now, awake brain surgery is a valuable option for many neurological problems. It offers a safer and more effective way to treat certain brain conditions.
When Is Awake Brain Surgery Necessary?
The choice to do awake brain surgery depends on several things. This includes the type and where the brain tumor is. Awake craniotomy is key for tumors near important brain parts. These parts control speech, movement, or feeling.
For some brain tumors, awake surgery is the best option. This is because they can’t be safely removed with regular surgery. The main aim is to remove as much of the tumor as possible. This helps keep important brain functions working well.
Types of Brain Tumors Requiring Awake Surgery
Some brain tumors need awake surgery because of where they are. These include:
- Gliomas: Tumors from brain glial cells. They need careful removal to save the brain around them.
- Meningiomas: Tumors in the meninges, the brain and spinal cord’s protective layers.
- Metastatic tumors: Tumors in the brain from other places. Awake surgery is sometimes needed for the best removal.
Neurological Conditions Treated
Awake brain surgery isn’t just for tumors. It’s also for other neurological issues. These include:
- Epilepsy: Awake surgery can find and remove the seizure cause.
- Vascular malformations: Abnormal brain blood vessels needing precise surgery.
- Movement disorders: Like Parkinson’s disease. Awake surgery can help manage symptoms by implanting devices.
Understanding awake brain surgery helps us see its complexity. The goal is always to get the best results with the least risk to the patient.
Patient Selection for Awake Craniotomy
To see if a patient is right for awake craniotomy, we do a detailed check. This check looks at both their health and mental state. It’s key to make sure the surgery goes well and the patient is safe.
Medical Criteria
When checking if a patient can have an awake craniotomy, we look at their health and the reason for surgery. Important things are the type and where the brain tumor or lesion is, how their brain is working, and if they can handle the surgery.
- The nature of the brain condition needing surgery.
- The patient’s current brain function and any problems.
- How well their body is and if they can have surgery.
Psychological Considerations
Checking the patient’s mind is just as important. We look at if they can work with us during the surgery. They need to be calm and able to talk during the operation.
Choosing who can have an awake craniotomy is a careful process. We look at both their health and mind to find the best candidates. This way, we can make sure they get the best care possible.
The Science Behind Keeping Patients Conscious During Brain Surgery
Keeping patients awake during brain surgery requires a deep understanding of brain anatomy and pain perception. The brain’s complex structure is key to the success of awake brain surgery.
Brain Anatomy and Pain Perception
The brain itself doesn’t have pain receptors. But the tissues around it, like the meninges and scalp, do feel pain. This is important for surgeons, as it lets them work on the brain while the patient is awake without causing too much pain.
It’s important to understand pain perception during brain surgery for good pain management. Surgeons use different methods to numb the scalp and other sensitive spots. This keeps the patient comfortable during the surgery.
- Local anesthetics are used to numb the scalp.
- Scalp nerve blocks are used to prevent pain.
- Advanced monitoring techniques help check the patient’s comfort.
Mapping Brain Function During Surgery
Brain mapping techniques are key in awake craniotomy. They help surgeons find and keep important brain areas. By keeping the patient awake, surgeons can have them do tasks to map brain function live.
This interactive method makes sure important areas like speech, motor control, and thinking are not harmed during surgery. Techniques include:
- Electrical stimulation to map brain areas.
- Task-based activities to check cognitive and motor functions.
- Continuous communication with the patient to watch their neurological status.
By using advanced brain mapping techniques and the patient’s feedback, surgeons can safely remove brain tumors or lesions. This leads to better results for the patient.
Pre-Surgical Preparation for Awake Craniotomy
Awake craniotomy needs careful planning before surgery. We check each patient’s health and prepare them well. This makes sure they are safe and the surgery goes well.
Physical Assessments
Checking the body is very important before surgery. We look at the heart and brain health. This helps us spot any risks during the surgery.
We also look at the patient’s medical history and what medicines they take. This helps us plan the anesthesia and surgery just right for them.
Assessment Type | Purpose | Components |
Cardiovascular Examination | Evaluate heart health and risk factors | ECG, Blood Pressure Monitoring, Heart Rate Variability |
Neurological Examination | Assess neurological function and possible deficits | Cognitive Tests, Motor Function Tests, Sensory Tests |
Psychological Preparation
Getting ready mentally is just as important. We offer counseling to help patients understand the surgery. We also teach them how to deal with anxiety and recovery.
We talk to patients about their fears and worries. This helps them feel ready for the surgery. It makes their experience better.
Patient Education Process
Telling patients what to expect is key. We explain the surgery, what they might feel, and how they can help. This makes them feel more in control.
We make our information easy to understand. This helps patients know what’s happening. It lets them make good choices and feel more confident.
By doing thorough checks, preparing mentally, and educating patients, we get them ready for surgery. This helps them have a good outcome and feel supported during their journey.
Numbing Techniques for Awake Brain Surgery
Numbing techniques are key in awake brain surgery. They help patients stay comfortable and able to follow instructions. This is vital for the success of awake craniotomy, as it lets patients handle the surgery while awake.
Scalp Nerve Blocks
Scalp nerve blocks are a main part of numbing in awake brain surgery. We inject local anesthetics around scalp nerves for the incision area. This greatly reduces pain at the start of surgery.
These blocks target nerves like the supraorbital and greater occipital nerves. By blocking these, we numb the scalp well. This makes the patient less uncomfortable.
Local Anesthetics Used
Local anesthetics are vital in awake brain surgery. They’re used for scalp blocks and more anesthesia as needed. Lidocaine, ropivacaine, and bupivacaine are common choices. They’re picked for their effectiveness and safety.
The right local anesthetic depends on the patient’s needs and how long it’s needed. This ensures the best pain control during surgery.
Pain Management Strategies
Pain management in awake brain surgery is complex. We use many strategies to keep patients comfortable. This includes watching their pain, adjusting anesthetics, and using extra meds when needed.
Pain Management Strategy | Description | Benefits |
Scalp Nerve Blocks | Injection of local anesthetics around scalp nerves | Effective pain relief during incision and craniotomy |
Local Anesthetic Application | Direct application of anesthetics to exposed brain areas | Minimizes pain during brain manipulation |
Monitoring and Adjustment | Continuous monitoring of patient pain and adjustment of anesthesia | Ensures optimal pain control throughout the procedure |
By using these strategies together, we make sure patients have little pain. This lets them work well with the surgical team.
The Asleep-Awake-Asleep Technique
The asleep-awake-asleep technique is a complex method used in awake craniotomies. It ensures patient comfort and safety. The technique involves three phases: initial sedation, awakening, and post-procedure sedation.
Initial Sedation Phase
In the initial sedation phase, patients are given anesthetics to relax. This helps reduce discomfort. It’s key for preparing the patient for surgery, allowing the team to start without causing distress.
Awakening Process
The awakening process is a vital part of the asleep-awake-asleep technique. Patients are slowly brought to a state where they can respond to commands. They can also participate in brain mapping. This phase needs careful control over anesthesia to keep the patient comfortable and cooperative.
Post-Procedure Sedation
After the surgery’s critical part is done, patients are sedated again. This phase aims to reduce discomfort and stress. It helps make the end of the surgery less traumatic for the patient.
The asleep-awake-asleep technique requires teamwork from neurosurgeons, anesthesiologists, and nurses. Each phase is managed with precision to achieve the best results for the patient.
Phase | Description | Patient State |
Initial Sedation | Anesthetics are administered to relax the patient. | Sedated |
Awakening | The patient is gradually awakened for brain mapping. | Conscious |
Post-Procedure Sedation | The patient is sedated again after the critical surgery portion. | Sedated |
What Patients Experience During Awake Brain Surgery
Patients having awake brain surgery might feel pressure or mild discomfort. But they don’t feel pain because of special numbing methods. Each person’s experience is different, based on the surgery type and their pain tolerance.
Sensations and Awareness
During the surgery, patients are usually aware of what’s happening around them. They might feel some pressure or mild discomfort. But thanks to local anesthetics and scalp nerve blocks, they don’t feel pain. Effective numbing is key for a successful surgery, keeping patients comfortable.
Communication with the Surgical Team
It’s important for patients to talk with the surgical team during awake brain surgery. They might be asked to answer questions or do simple tasks. This helps surgeons check brain function in real-time and reduces the risk of damage.
We make sure patients know how important their help is. We explain the tasks they’ll do, like naming objects or counting. We reassure them that their help is critical for the surgery’s success.
Cognitive and Motor Testing
Cognitive and motor tests are a big part of awake brain surgery. These tests help find and keep safe important brain areas. Patients might be asked to do tasks like naming objects or moving their limbs.
These tasks are simple but tell a lot. They help the surgical team watch brain function closely. This way, they can make changes during the surgery if needed.
Task Type | Purpose | Examples |
Cognitive Tasks | Assess language and cognitive functions | Naming objects, reading, simple arithmetic |
Motor Tasks | Evaluate motor function and response | Moving limbs, gripping, releasing |
Sensory Tasks | Test sensory perception | Feeling touch, temperature changes |
By involving patients in their surgery, we can make it more successful. This way, we can remove the needed brain area while keeping important functions safe.
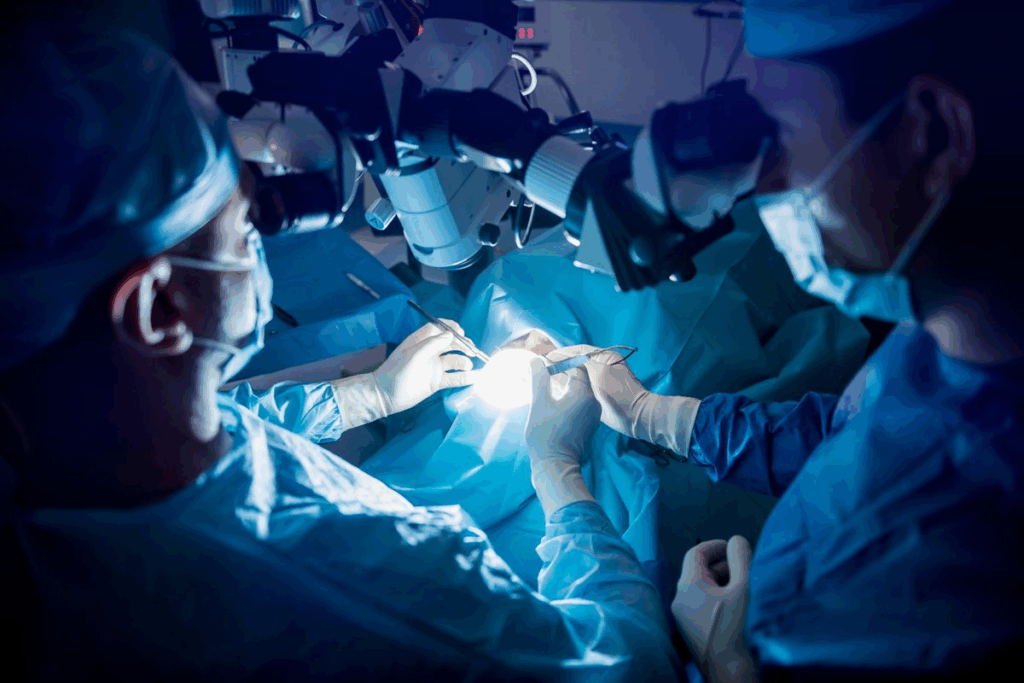
The Surgical Team’s Role in Awake Procedures
The success of awake brain surgery depends on the team’s skill and teamwork. Awake craniotomy is a complex procedure that needs a team effort. Neurosurgeons, anesthesiologists, neuropsychologists, and speech pathologists must work together.
Neurosurgeon Responsibilities
Neurosurgeons are key in awake brain surgery. They remove tumors while keeping brain functions intact. They need to communicate with the patient during surgery, using feedback to make decisions.
Anesthesiologist’s Critical Function
The anesthesiologist’s role is vital, managing pain and sedation. They keep the patient comfortable and safe. Effective pain management is essential for the success of awake craniotomy.
Neuropsychologist and Speech Pathologist Involvement
Neuropsychologists and speech pathologists play a big role in the team. They check the patient’s brain and language skills. Real-time cognitive and motor testing helps the team adjust during surgery. Their work is key to avoiding long-term brain or language problems.
Together, the team works to get the best results for patients. The skills of neurosurgeons, anesthesiologists, neuropsychologists, and speech pathologists are vital for success.
Comparing Awake and Traditional Brain Surgery Approaches
Choosing between awake and traditional brain surgery is key. It affects the patient’s outcome and recovery. We’ll look at the differences in anesthesia and the results of each method.
Anesthesia Protocols: A Key Differentiator
Awake and traditional brain surgeries differ mainly in anesthesia. Traditional surgery uses general anesthesia, making the patient sleep through it. Awake surgery, or awake craniotomy, uses local anesthesia and sedation. This lets the patient stay awake and respond during parts of the surgery.
Awake brain surgery uses local anesthetics to numb the scalp and brain area. This lets the team watch the brain work in real-time. It can lead to more accurate surgery.
Outcomes and Success Rates
Awake surgery often preserves brain function better than traditional surgery. It allows for adjustments during the surgery. This can improve cognitive and motor skills after surgery.
A study showed awake craniotomy patients had “significantly better outcomes in terms of neurological function and quality of life” than those under general anesthesia.
“The awake craniotomy technique allows for a more nuanced approach to brain surgery, potentially reducing the risk of damage to critical brain areas.”
The success of awake surgery also depends on the team’s expertise. Neurosurgeons, anesthesiologists, and neuropsychologists work together. This ensures patients get care that fits their needs.
In summary, both awake and traditional surgeries have their roles. The choice depends on the condition, patient health, and the benefits of monitoring brain function in real-time.
Risks and Complications of Awake Brain Surgery
Awake brain surgery is a cutting-edge procedure but comes with risks. It’s important to know about these challenges. This way, patients can be better prepared for the surgery and recovery.
Anesthesia-Related Risks
One big worry is anesthesia-related complications. Even though patients are awake, local anesthesia is used. This can lead to breathing or heart problems. We keep a close eye on our patients to reduce these risks.
Anesthesia-Related Risk | Description | Mitigation Strategy |
Respiratory Complications | Issues related to breathing during the procedure. | Continuous monitoring of oxygen levels and respiratory rate. |
Cardiac Complications | Heart-related issues during surgery. | Close monitoring of heart rate and blood pressure. |
Intraoperative Seizures
Intraoperative seizures are another risk. These seizures can happen when the brain is stimulated during surgery. We do our best to prevent them, but it’s good for patients to know about this risk. Our team is ready to handle any seizures that might happen.
Psychological Effects
The surgery can also affect patients’ minds. Being awake during surgery can be stressful and cause anxiety. We offer support to help patients deal with these effects. This ensures their mental health during recovery.
In summary, awake brain surgery is safe but has risks. Knowing about these complications helps patients prepare for surgery and recovery. Our team is dedicated to providing top care to reduce risks and ensure the best results.
Recovery After Awake Craniotomy
The journey to recovery after an awake craniotomy has many stages. Each stage is tailored to the patient’s needs and surgery specifics. Understanding these stages helps manage expectations and ensures the best outcomes.
Immediate Post-Operative Period
Right after surgery, patients are watched closely in a recovery unit. Medical staff manage pain, swelling, and any complications. Effective pain management is key, using a mix of medicines and other methods to keep patients comfortable.
They also look for any neurological issues or complications. Advanced monitoring and teamwork among healthcare professionals help address problems quickly.
Hospital Stay Duration
The time spent in the hospital after an awake craniotomy varies. It depends on the surgery’s extent, the patient’s health, and how quickly they recover. Usually, patients stay a few days for close monitoring and initial recovery.
- Initial recovery in the post-anesthesia care unit (PACU)
- Transfer to a neurosurgical ward for further care
- Discharge planning based on the patient’s progress
Long-Term Recovery Timeline
Recovery after an awake craniotomy takes time, often weeks to months. Patients are told to gradually increase their activity levels. They also follow a rehabilitation plan, which might include physical or speech therapy.
Regular follow-up appointments are key. They help monitor the patient’s progress and address any issues. This way, we can offer personalized care and support throughout their recovery.
Conclusion
Awake brain surgery, or awake craniotomy, is a complex neurosurgical procedure. It needs a team effort from many experts. Patients and their families can better understand this by knowing the steps from start to finish.
We’ve looked at the key parts of awake brain surgery. This includes what it is, its history, and the conditions it helps. A skilled team, like neurosurgeons and anesthesiologists, work together to help patients.
In short, awake brain surgery is a special procedure that helps some patients a lot. As neurosurgery gets better, knowing about awake craniotomy is key. This summary shows how teamwork is vital for good results.
FAQ
What is awake brain surgery?
Awake brain surgery, also known as awake craniotomy, is a complex procedure. The patient stays awake and alert during the operation. This allows for real-time monitoring of brain function.
Why is awake brain surgery necessary?
It’s needed for certain brain tumors or lesions near important brain areas. These areas control speech, movement, or sensation. The goal is to remove the tumor while keeping brain function intact.
How is pain managed during awake brain surgery?
Pain is managed with numbing techniques. Scalp nerve blocks and local anesthetics are used. They numb the scalp to prevent pain during the incision and craniotomy.
What is the asleep-awake-asleep technique?
This technique is used in some awake craniotomies. The patient is first sedated, then awakened during the critical part of the surgery. They are sedated again to ensure comfort and safety.
What sensations do patients experience during awake brain surgery?
Patients might feel pressure or mild discomfort, but not pain. This is due to effective numbing and anesthesia. They are also asked to perform tasks to assess brain function.
Who is involved in the surgical team for awake brain surgery?
The team includes neurosurgeons, anesthesiologists, neuropsychologists, and speech pathologists. They work together to ensure the surgery’s success and preserve brain functions.
What are the risks associated with awake brain surgery?
Risks include anesthesia-related complications, such as respiratory or cardiac issues. There’s also the risk of intraoperative seizures and psychological effects from the stress and uniqueness of the experience.
How long does recovery take after awake craniotomy?
Recovery involves monitoring in the immediate post-operative period. The hospital stay varies. Long-term recovery depends on the surgery’s extent and individual factors.
Can anyone undergo awake brain surgery?
Not everyone can have awake brain surgery. Selection involves medical and psychological evaluations. It’s to ensure the patient can tolerate the procedure and cooperate during surgery.
How is brain function monitored during awake brain surgery?
Brain function is monitored in real-time. Advanced brain mapping techniques are used. Patients also perform cognitive and motor tasks during surgery.
What is the role of the anesthesiologist during awake brain surgery?
The anesthesiologist manages pain and sedation. They ensure patient comfort throughout the surgery, including the asleep-awake-asleep technique.
Are there any long-term effects of awake brain surgery?
Long-term effects vary based on the surgery’s extent and individual factors. The goal is to preserve brain functions and minimize long-term deficits.
References
ScienceDirect. Evidence-Based Medical Insight. Retrieved from https://www.sciencedirect.com/science/article/pii/B9780444534972000158