
Cancer diagnosis uses many lab tests to find signs of cancer. The Complete Blood Count (CBC) with differential is key. It checks the levels of red, white blood cells, and platelets.
Odd cell counts can mean cancer might be present. An abnormal CBC/diff result could lead to more tests. Understanding what a complete blood count check and other tests reveal is crucial.
Lab tests are very important in finding cancer. Knowing what to look for can help a lot. We’ll look at the CBC with differential and other tests, and what lab levels normal are.
Key Takeaways
- Complete Blood Count (CBC) with differential is a key test for cancer.
- Odd CBC/diff results might mean cancer is there.
- It’s vital to understand lab test results for accurate cancer diagnosis.
- Many lab tests help find cancer, like cancer tumor blood tests.
- Knowing normal lab levels helps spot odd results.
The Role of Laboratory Testing in Cancer
Lab tests are key for finding cancer early and planning treatment. They help spot cancer early, check how well treatments work, and find any signs of cancer coming back.
How Lab Tests Aid in Cancer Detection
Lab tests are vital for catching cancer early. They find oddities in blood cells, proteins, and biomarkers that might mean cancer is present. For example, a Complete Blood Count (CBC) test can show odd blood cell counts that hint at cancer. Also, blood tests for Carcinoembryonic Antigen (CEA) and CA-125 can help diagnose some cancers.
Lab tests also check a patient’s overall health. Tests like the Comprehensive Metabolic Panel (CMP) show how cancer might be affecting the body, like the liver and kidneys.
Laboratory Monitoring Throughout Cancer Treatment
Lab tests are key during cancer treatment. They help doctors see how well treatments are working. For instance, a CBC test can track how chemotherapy affects blood cells. Liver function tests check if treatments are too harsh.
Lab tests also help find cancer coming back. By watching tumor markers and other tests, doctors can spot recurrence early. This makes it easier to treat.
CBC with Differential: The Fundamental Blood Test for Cancer Screening
The CBC with differential blood test is key for checking health and finding signs of cancer. It looks at different blood cells like red, white, and platelets. This helps doctors see if there are any problems.
Components of a Complete Blood Count with Differential
A CBC with differential has several important parts:
- Red Blood Cell (RBC) count: Checks the number of RBCs, which carry oxygen.
- White Blood Cell (WBC) count: Looks at the number of WBCs, important for the immune system.
- Platelet count: Checks the number of platelets, key for blood clotting.
- Differential count: Shows the types of WBCs, like neutrophils and lymphocytes.
Knowing these parts is key to understanding CBC results. A medical expert says, “The differential count gives important info about the immune system. It can show infections, inflammation, or cancer.“
Normal Ranges and What Constitutes Abnormal Results
Normal CBC ranges can differ slightly by lab but are usually set. Abnormal results can mean different health issues, like:
- Anemia or polycythemia (abnormal RBC count)
- Infections or leukemia (abnormal WBC count)
- Bleeding disorders or thrombocytosis (abnormal platelet count)
It’s important to talk to a healthcare professional about abnormal CBC results.
How to Prepare for a CBC Blood Test
Getting ready for a CBC blood test is easy:
- Tell your healthcare provider about any medicines or supplements.
- Follow any special instructions from your healthcare provider.
- The test is usually done in the morning.
Good preparation leads to accurate test results.
Red Blood Cell Abnormalities in Cancer Patients
Cancer patients often face red blood cell issues that affect their treatment and life quality. These problems can show up as anemia, changes in hemoglobin and hematocrit, and odd red blood cell shapes.
Cancer-Related Anemia Patterns
Anemia is common in cancer patients, caused by the disease or treatment. Cancer-related anemia makes patients feel tired, weak, and short of breath. The type of cancer can influence the anemia pattern.
Hemoglobin and Hematocrit Changes
In cancer patients, hemoglobin and hematocrit levels often change. Hemoglobin drops in anemia, and hematocrit, which measures red blood cells, can also change. Keeping an eye on these is key to managing anemia and other red blood cell issues.
| Parameter | Normal Range | Abnormal in Cancer |
| Hemoglobin (g/dL) | 13.8-17.2 (male) | Often decreased |
| Hematocrit (%) | 40.7-50.3 (male) | Often decreased |
| RBC Morphology | Normal shape and size | Variations in size and shape |
RBC Morphology Alterations in Malignancy
Changes in red blood cell shape and size can hint at cancer. Cancer patients might have red blood cells that are not the usual size or shape. These changes can help doctors diagnose cancer.
In conclusion, red blood cell issues are a big worry for cancer patients. They need close monitoring and care to do better.
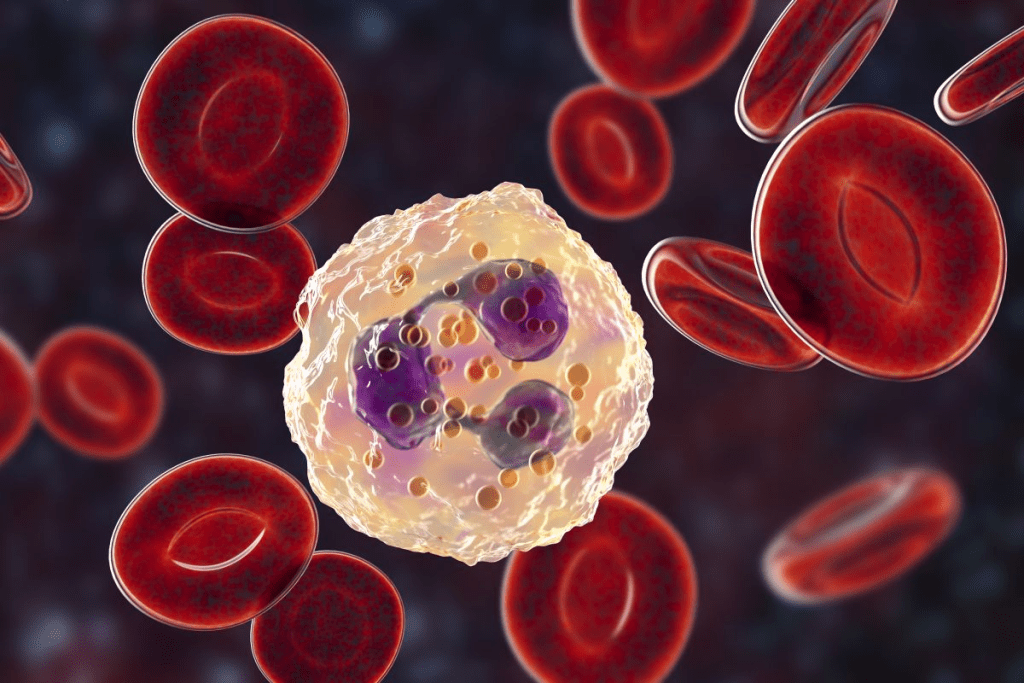
White Blood Cell Alterations Associated with Different Cancers
White blood cell changes are common in many cancers. These changes can affect how doctors diagnose and treat the disease. They often involve changes in the number or function of neutrophils and lymphocytes.
Leukocytosis vs. Leukopenia in Cancer
Cancer patients often see changes in their white blood cell counts. This can be either an increase (leukocytosis) or a decrease (leukopenia). Leukocytosis might happen due to infection, inflammation, or as a side effect of some cancers. On the other hand, leukopenia makes it harder for the body to fight off infections and can be caused by cancer or chemotherapy.
Knowing whether a patient has leukocytosis or leukopenia is key. It helps doctors choose the right treatment. This could mean treating an infection or adjusting the dose of chemotherapy.
Neutrophil Count and Function Abnormalities
Neutrophils are important for fighting infections. In cancer patients, problems with neutrophils can be serious. An increase in neutrophils (neutrophilia) might mean the body is fighting an infection or has cancer. A decrease (neutropenia) makes it harder to fight off infections and is a common side effect of chemotherapy.
| Condition | Description | Clinical Significance |
| Neutrophilia | Elevated neutrophil count | May indicate infection, inflammation, or certain cancers |
| Neutropenia | Low neutrophil count | Increases risk of infections, common in chemotherapy |
Lymphocyte Abnormalities and Their Significance
Lymphocytes are also affected in cancer. An increase (lymphocytosis) or decrease (lymphopenia) in lymphocytes can happen. Some cancers, like lymphomas, directly affect lymphocytes. Others might cause lymphopenia by weakening the bone marrow.
It’s important to understand lymphocyte changes for diagnosing and managing blood cancers. Knowing about lymphocyte subsets can help doctors understand the immune system better. This information can guide treatment choices.
Platelet Abnormalities and Cancer Correlation
Platelet abnormalities are key in diagnosing and tracking different cancers. The platelet count, part of a complete blood count (CBC), offers insights into cancer presence and growth.
Thrombocytosis as a Cancer Marker
Thrombocytosis, or high platelet counts, signals some cancers. It’s linked to poor outcomes in lung, gastrointestinal, and ovarian cancers. The reasons behind this are complex, involving cytokines and growth factors that boost platelet making.
“Thrombocytosis in cancer patients often means a more aggressive disease,” studies say. It may need more tests to diagnose.
Thrombocytopenia in Advanced Malignancies
Thrombocytopenia, or low platelet counts, happens in advanced cancers. It’s often due to cancer cells in the bone marrow or from treatments like chemotherapy and radiation. This condition raises the risk of bleeding, a big worry for cancer patients.
Mean Platelet Volume (MPV) Changes
MPV, a measure of platelet size, changes in cancer patients. These changes suggest problems with platelet making or destruction. Some research links MPV changes to certain cancers and their outcomes.
The link between platelet issues and cancer is complex. Platelet counts and functions can be affected by cancer, and vice versa. Grasping these connections is vital for better cancer diagnosis and care.
Comprehensive Metabolic Panel Findings in Cancer
The CMP is a key tool for diagnosing cancer. It checks liver and kidney function. This helps doctors make treatment plans and watch for side effects.
Liver Function Test Abnormalities
Liver tests in the CMP show how the liver is doing in cancer patients. If these tests are off, it might mean liver damage or cancer spread.
- Elevated Liver Enzymes: High ALT and AST levels mean liver damage or cancer spread.
- Bilirubin Levels: Too much bilirubin can mean liver problems or blocked bile ducts, linked to some cancers.
- Alkaline Phosphatase (ALP): High ALP levels suggest liver or bone cancer.
Kidney Function Parameters in Cancer Patients
The CMP also checks kidney function. This is important for patients getting treatments that might harm their kidneys.
- Creatinine Levels: High creatinine means kidney problems, possibly from cancer or treatment.
- Blood Urea Nitrogen (BUN): Changes in BUN levels show kidney function. They can be affected by many things, like how hydrated you are or your meds.
- Electrolyte Balance: Kidney function affects how well your body balances electrolytes. Problems can cause heart issues or muscle weakness.
Electrolyte Imbalances Associated with Malignancies
Electrolyte problems are common in cancer patients. They can come from the cancer itself, treatments, or other issues.
- Hyponatremia: Low sodium can happen for many reasons, like SIADH syndrome linked to some cancers.
- Hypokalemia: Low potassium can be caused by treatments or the cancer itself.
- Hypercalcemia: High calcium levels can be linked to cancer, either from bone metastasis or paraneoplastic syndromes.
Knowing about CMP findings is key for managing cancer patients. It helps doctors understand the metabolic changes caused by cancer and its treatment.
Tumor Markers: Blood Tests Specific to Cancer Detection
Blood tests for tumor markers are key in finding and tracking cancer. These tests look for substances in the blood that might mean cancer is present. These substances, or markers, are proteins or other signs that could point to a tumor.
Carcinoembryonic Antigen (CEA) and Its Clinical Significance
CEA is a marker linked to many cancers, like colorectal cancer. High CEA levels can show cancer has come back or spread. It’s important to watch CEA levels to manage colorectal cancer and see if treatments are working.
CEA’s role goes beyond just finding cancer. It helps track how the disease is growing and how well treatments are doing. But, it’s important to remember that high CEA levels can also show up in conditions that aren’t cancer, like inflammatory bowel disease.
CA-125, PSA, AFP and Other Common Tumor Markers
There are other tumor markers used in medicine too. CA-125 is mainly for ovarian cancer, while PSA is for prostate cancer screening. Alpha-fetoprotein (AFP) is linked to liver cancer and some germ cell tumors. Each marker has its own use and limitations.
- CA-125 helps track ovarian cancer treatment and find any signs of it coming back.
- PSA levels are key for prostate cancer screening and tracking.
- AFP is used in diagnosing and tracking liver cancer and certain germ cell tumors.
Limitations and Proper Interpretation of Tumor Marker Tests
Tumor markers are helpful in fighting cancer, but they have their limits. No single marker is only for cancer, and sometimes they can show false positives. So, understanding what these tests mean needs a deep look at the patient’s situation and other test results.
Getting the most from these tests means knowing their strengths and weaknesses, the patient’s health history, and other test results. Remember, tumor markers are just part of a bigger plan to diagnose and treat cancer. This plan also includes imaging, biopsies, and a doctor’s evaluation.
Flow Cytometry in Cancer Diagnosis and Classification
In cancer diagnosis, flow cytometry is key. It helps understand hematologic malignancies. This method looks at cells in a sample, giving insights into their traits.
Principles and Applications of Flow Cytometry
Flow cytometry works by analyzing cells with lasers. It measures cell size, complexity, and protein presence. This is vital for diagnosing and classifying cancers like leukemia and lymphoma.
It’s not just for diagnosis. Flow cytometry also tracks disease progress and treatment effects. It helps tailor treatments to cancer types.
Interpreting Flow Cytometry Results in Hematologic Malignancies
Understanding flow cytometry results is complex. It involves knowing the cell surface markers of cancers. This helps spot abnormal cells and diagnose diseases like ALL or CLL.
Healthcare professionals compare patient cell profiles to known cancer types. This helps choose the right treatment.
Flow Cytometry vs. Traditional Blood Tests
Flow cytometry beats traditional blood tests in cancer diagnosis. It gives detailed cell information, unlike general blood tests. This leads to more accurate diagnoses.
It also finds minimal residual disease. This is key for tracking treatment success and predicting relapse.
Coagulation Profile Abnormalities in Cancer
Cancer can cause many changes in how blood clots, making it more likely to form clots. These changes can affect how well cancer is managed and the patient’s outlook.
Cancer-Associated Hypercoagulability
In cancer patients, blood clots more easily. This can lead to venous thromboembolism (VTE), a serious condition. Tumors, the body’s clotting system, and inflammation all play a role in this.
Some cancers, like pancreatic and brain cancer, are more likely to cause VTE. High risk of clotting can also mean a worse prognosis.
D-dimer Elevation in Malignancy
D-dimer is a sign of blood clot breakdown. In cancer patients, high D-dimer levels often mean thrombosis or tumor growth. It’s not specific to cancer but helps assess VTE risk and disease progression.
D-dimer’s role in cancer is important. It helps identify patients at high risk of clots and guides treatment to prevent them.
PT, PTT, and INR Changes in Cancer Patients
Cancer and its treatment can alter blood clotting tests like PT, PTT, and INR. These changes can signal a higher risk of bleeding or clotting.
Prolonged PT or INR might point to coagulopathy or liver issues. Elevated PTT could mean anticoagulant therapy or a clotting factor problem. Keeping an eye on these tests is key for managing cancer patients, mainly those on chemotherapy or at risk of bleeding.
Inflammatory and Acute Phase Reactants in Cancer
Inflammatory and acute phase reactants are key in the body’s fight against cancer. These proteins rise when there’s inflammation or cancer. They give important clues about the patient’s health.
C-Reactive Protein and ESR Elevations
C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) show inflammation levels. High CRP and ESR levels are linked to many cancers and a worse prognosis. Monitoring these markers helps gauge disease severity and treatment success.
In cancer, CRP rises due to pro-inflammatory cytokines. ESR goes up with acute phase protein production. Knowing this helps manage cancer patients better.
Ferritin and Other Acute Phase Proteins
Ferritin, an acute phase protein, goes up in cancer patients. It’s seen in many cancers, including blood cancers. Other proteins like haptoglobin and ceruloplasmin also rise, showing inflammation.
These proteins’ rise is tied to tumor growth and spread. Monitoring their levels sheds light on disease progression and treatment response.
Cytokine Profiles in Cancer Patients
Cytokines are vital in the immune fight. In cancer, certain cytokine levels hint at disease severity. For example, high IL-6 and TNF-alpha levels are linked to poor outcomes.
Grasping cytokine profiles aids in creating targeted treatments. Analyzing cytokine levels offers insights into the immune response and immunotherapy success.
Hormone and Endocrine Function Tests in Cancer Diagnosis
It’s key to know how hormone and endocrine tests work in finding cancer. These tests spot problems in hormone making and endocrine system work linked to cancer.
Hormone-Producing Tumors and Their Laboratory Signatures
Hormone-making tumors can cause too much or too little hormone, leading to symptoms. Blood or urine tests are vital to find these tumors by checking hormone levels.
- Pheochromocytomas, which produce catecholamines
- Thyroid carcinomas, which can produce thyroid hormones
- Pancreatic neuroendocrine tumors, which can produce insulin, gastrin, or other hormones
Paraneoplastic Endocrine Syndromes
Paraneoplastic endocrine syndromes happen when cancer cells make substances that act like hormones. These syndromes show signs of cancer and can cause hormone-related symptoms.
- Ectopic Cushing’s syndrome due to ACTH production by non-pituitary tumors
- Hypercalcemia of malignancy due to parathyroid hormone-related protein (PTHrP) production
Endocrine Function Disruption by Cancer Treatments
Cancer treatments like surgery, chemo, and radiation can mess with hormone balance. This can cause long-term health problems, like thyroid issues after neck radiation or hormone imbalances after gland surgery.
- Monitoring endocrine function before, during, and after cancer treatment
- Managing treatment-induced endocrine dysfunction to improve quality of life
Advanced Molecular and Genetic Testing in Oncology
Oncology is changing fast with new molecular and genetic tests. These tools help doctors tailor treatments to each patient’s cancer. This makes care more personal and effective.
Circulating Tumor DNA and Liquid Biopsy
Circulating tumor DNA (ctDNA) and liquid biopsy are big steps forward in cancer care. They let doctors check on cancer without invasive tests. ctDNA is DNA from tumors found in blood, helping track cancer and treatment.
Liquid biopsy analyzes ctDNA in blood or fluids. It’s great for checking how well treatments work and spotting new mutations.
Next-Generation Sequencing in Cancer Diagnostics
Next-generation sequencing (NGS) is a fast way to read DNA or RNA. In cancer, it finds genetic changes that help tumors grow. This helps doctors find the right treatments.
NGS shows what genes are changed in tumors. It helps predict how well treatments will work. It also spots cancer cells left behind after treatment.
Genetic Mutation Profiles and Targeted Therapy Selection
The genetic makeup of a tumor affects how it grows and responds to treatment. Advanced tests find specific mutations that guide therapy choices.
Matching treatments to a tumor’s genetic profile improves results and reduces side effects. For example, EGFR testing helps choose treatments for lung cancer.
| Genetic Mutation | Associated Cancer Type | Targeted Therapy |
| EGFR mutation | Non-small cell lung cancer | Erlotinib, Gefitinib |
| HER2 amplification | Breast cancer | Trastuzumab |
| BRAF V600E mutation | Melanoma | Vemurafenib |
Advanced molecular and genetic tests are changing cancer care. They help doctors give more precise treatments. As these technologies get better, they will keep improving patient care.
Interpreting Abnormal Lab Results: Cancer vs. Other Conditions
When lab results show something’s off, figuring out if it’s cancer or not can be tough. It’s important to look at the big picture and understand what the tests mean. Knowing about different lab tests and their meanings is key.
Common Lab Abnormalities That May Indicate Cancer
Some lab results might hint at cancer, but they don’t always mean it. For example, a Complete Blood Count (CBC) with Differential can show odd blood cell counts. These could point to cancer, but they can also mean other things.
| Lab Test | Abnormality | Possible Cancer Association |
| CBC with Differential | Anemia | Cancer-related anemia, leukemia |
| CBC with Differential | Leukocytosis | Leukemia, lymphoma |
| Platelet Count | Thrombocytopenia | Bone marrow metastasis, leukemia |
A medical expert says, “Lab results need to be seen in the light of the patient’s whole story and health history.”
“Lab results aren’t just looked at on their own. They need to be matched with what’s happening in the body and sometimes more tests are needed to be sure.”
Non-Cancer Causes of Similar Lab Abnormalities
It’s important to remember that odd lab results can mean many things, not just cancer. For instance, anemia can be from lack of iron, chronic illness, or not enough vitamins. Leukocytosis might be from an infection, inflammation, or stress.
- Infection or inflammation causing leukocytosis
- Chronic disease or nutritional deficiencies leading to anemia
- Medication side effects or bone marrow disorders affecting platelet counts
Knowing these other reasons is vital for making the right diagnosis and treatment plan.
When to Pursue Further Testing for Cancer
Figuring out if more tests are needed for cancer depends on several things. These include the patient’s risk factors, how they’re feeling, and the first lab results. If tests show something that could be cancer, more tests like scans, biopsies, or more lab work might be needed.
More tests can confirm if cancer is there, how far it’s spread, and help decide the best treatment. A doctor must think about the benefits and risks of more tests. They also need to consider the patient’s overall health and what they want.
Conclusion: The Future of Laboratory Testing in Cancer Care
Laboratory testing is key in cancer care. It helps doctors diagnose and treat cancer accurately. As cancer care grows, so will the role of lab tests in improving patient results.
New technologies like liquid biopsy and next-generation sequencing are changing cancer care. They make it possible for treatments to be more tailored to each patient. This leads to better and more effective cancer care.
Lab tests are getting smarter as research moves forward. Soon, doctors will be able to find cancer early and track how treatments work better. This will be a big step forward in cancer care.
Healthcare providers are using the latest lab tests to make cancer care better. As these tests keep getting better, they will play an even bigger role in fighting cancer. It’s clear that lab tests will always be important in cancer treatment.
FAQ
What is a CBC with differential, and how is it used in cancer diagnosis?
A CBC with differential is a blood test. It checks the levels of different blood cells. This includes red, white, and platelets. It helps find signs of cancer.
What are tumor markers, and how are they used in cancer detection?
Tumor markers are blood tests for cancer. Examples are Carcinoembryonic Antigen (CEA) and CA-125. They help see how well treatment is working and if cancer comes back.
How does flow cytometry aid in cancer diagnosis?
Flow cytometry is a test that looks at blood cells. It’s great for finding cancers like leukemia and lymphoma.
What is the significance of coagulation profile abnormalities in cancer patients?
Coagulation problems can make cancer patients more likely to get blood clots.
How do inflammatory and acute phase reactants relate to cancer?
Inflammatory and acute phase reactants, like C-reactive protein, go up with inflammation or cancer.
What is the role of hormone and endocrine function tests in cancer diagnosis?
Hormone tests find tumors that make hormones. They also find endocrine syndromes caused by cancer.
How do advanced molecular and genetic tests aid in cancer diagnosis and treatment?
Tests like circulating tumor DNA help monitor cancer without surgery. They help choose the right treatment.
How do I interpret abnormal lab results, and when should I pursue further testing for cancer?
Understanding abnormal lab results needs careful thought. Look at your medical history and current health. Get more tests if results suggest cancer.
Do I need to fast for a CBC blood test?
No, fasting is not needed for a CBC blood test.
Can stomach cancer be detected in blood work?
Blood tests can spot some signs of stomach cancer. But, they’re not enough to confirm it.
What is the normal range for a CBC test?
Normal CBC ranges vary by lab. They cover red, white, and platelet counts.
Can a CBC with differential detect cancer?
A CBC with differential can find signs of cancer. But, it’s not a sure way to diagnose it.
What is the difference between a CBC and a CBC with differential?
A CBC with differential looks at white blood cell types. A CBC doesn’t.
References
National Cancer Institute. (2024). Leukemia – StatPearls. Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK560490


































