Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid beta-peptide builds up in brain blood vessels. This increases the risk of brain bleeding and memory loss cerebral amyloid.
CAA is found in almost half of Alzheimer’s patients. It’s also a big reason for brain bleeding in older people. New MRI scans help spot CAA by showing tiny brain bleeds and other signs.
Knowing how to diagnose and image CAA is key to managing it. Recent studies have highlighted CAA’s importance and its effects on patients.
Key Takeaways
- CAA is a significant condition affecting Alzheimer’s disease patients.
- Advanced MRI is critical for diagnosing CAA.
- Diagnosing CAA means looking for specific signs in the brain.
- Understanding CAA is vital for managing its effects on patients.
- CAA raises the risk of brain bleeding and memory loss.
What Is Cerebral Amyloid Angiopathy? Pathophysiology and Mechanisms
CAA is a condition where amyloid beta peptides build up in blood vessel walls. This makes the vessels weak. It’s caused by amyloid beta, a protein that plays a big role in CAA.
Amyloid Beta Deposition in Cerebral Blood Vessel Walls
Amyloid beta builds up in blood vessel walls in CAA. This comes from the amyloid precursor protein (APP). It mainly happens in the walls of small to medium-sized blood vessels.
Amyloid beta deposition causes blood vessels to change. This includes damage to the blood-brain barrier and inflammation.
- Amyloid beta peptides accumulate in cerebral vessel walls.
- Deposition occurs in small to medium-sized arteries and capillaries.
- Vascular changes include disruption of the blood-brain barrier.
Vascular Weakening and Structural Changes
Amyloid beta buildup weakens blood vessel walls. This makes them more likely to break and bleed. The changes include:
- Thinning and fragility of vessel walls.
- Loss of smooth muscle cells and elastic lamina.
- Increased permeability and inflammation.
The weakening of blood vessels increases the risk of bleeding in the brain. Knowing how CAA works is key to treating it.
Key Fact #1: CAA Prevalence Varies Significantly Across Populations

The amount of Cerebral Amyloid Angiopathy (CAA) varies a lot in different groups. This change is due to age, genetics, and other health issues.
General Population Statistics
CAA is common in older people. Autopsy studies show it affects 20% to 40% of those over 60. The wide range comes from different study groups and how they define CAA.
Prevalence in Cognitively Normal Elderly
Even those who think clearly can have CAA. Studies say up to 30% of them do. This shows CAA can exist without causing obvious problems at first.
This fact shows how complex CAA and brain health are linked. It points to the need for more research. We must learn why some people with CAA stay symptom-free.
Age as the Primary Risk Factor
Age is the biggest risk for CAA. The more you age, the higher your risk, starting at 60. The aging brain is more likely to get amyloid in blood vessels, causing CAA.
Knowing how age affects CAA is key to preventing and catching it early. As more people get older, CAA’s impact on health will grow. This makes studying CAA very important.
Key Fact #2: Strong Association Between Cerebral Amyloid and Alzheimer’s Disease
Cerebral Amyloid Angiopathy and Alzheimer’s disease are closely linked. This connection is due to amyloid beta deposition in both conditions. It’s key to understanding them.
48% Prevalence in Alzheimer’s Based on Pathology
Research shows CAA is common in Alzheimer’s patients. About 48% of Alzheimer’s cases have CAA. This shows a strong link between the two.
22% Prevalence Based on MRI Microbleeds
Studies using MRI found CAA in 22% of Alzheimer’s patients. Microbleeds indicate CAA and show how severe amyloid is in blood vessels.
Shared Pathological Mechanisms
CAA and Alzheimer’s both involve amyloid beta buildup. In CAA, amyloid beta weakens blood vessels, raising hemorrhage risk. In Alzheimer’s, it forms plaques that harm neurons and cause memory loss.
|
Pathological Feature |
CAA |
Alzheimer’s Disease |
|---|---|---|
|
Amyloid Beta Deposition |
In cerebral blood vessel walls |
In brain parenchyma as plaques |
|
Consequence |
Vascular weakening, hemorrhage risk |
Neuronal damage, cognitive decline |
Understanding how CAA and Alzheimer’s are connected is vital. It helps in finding better treatments. More research could lead to new ways to prevent and treat these diseases.
Key Fact #3: CAA Is a Major Cause of Lobar Intracerebral Hemorrhage
CAA is a big reason for lobar intracerebral hemorrhage, mainly in older people. It’s key to know how CAA affects intracerebral hemorrhage.
50-57% of Lobar Hemorrhage Cases Linked to CAA
Research shows that 50% to 57% of lobar intracerebral hemorrhage cases are due to CAA. This shows we need more study on how CAA and hemorrhage are linked.
A study in Neurology found CAA causes a lot of lobar hemorrhages in people over 60. It’s vital to think about CAA when diagnosing and treating intracerebral hemorrhage.
Hemorrhage Distribution and Patterns
Hemorrhage in CAA patients can vary a lot. Studies show CAA-related hemorrhages often happen in the lobar regions. These include the frontal, parietal, and occipital lobes.
|
Lobe |
Frequency of Hemorrhage |
|---|---|
|
Frontal |
35% |
|
Parietal |
25% |
|
Occipital |
20% |
|
Temporal |
15% |
|
Cerebellum |
5% |
The table shows the frontal lobe is most affected, followed by the parietal and occipital lobes. This matches the typical CAA presentation.
Risk Factors for First and Recurrent Bleeding
Several factors increase the risk of bleeding in CAA patients. Age is a big one, as the risk grows with age.
“The presence of microbleeds on MRI is a strong predictor of future hemorrhage risk in CAA patients,” according to a study published in Stroke.
Other risk factors include the apolipoprotein E ε4 allele, high blood pressure, and antithrombotic therapy. Knowing these risks helps in managing CAA patients better.
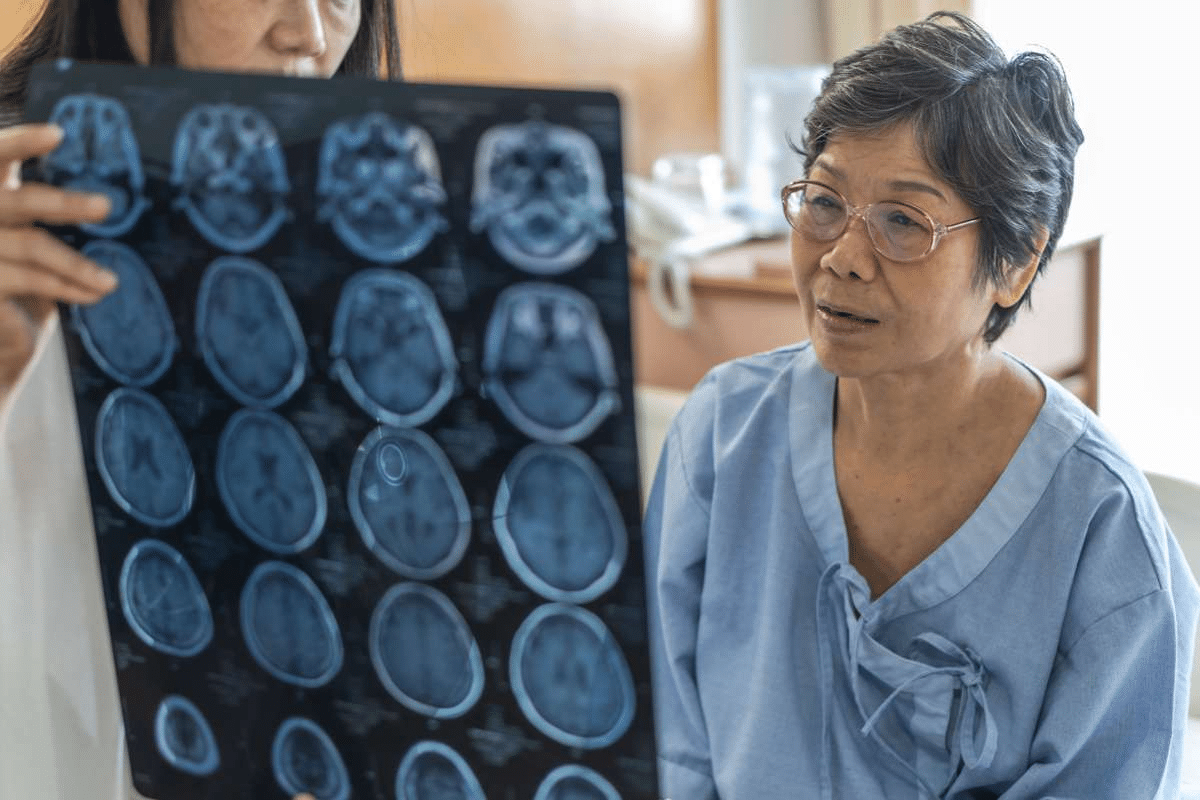
The image shows what CAA looks like on MRI, with characteristic lobar microbleeds. MRI is key for diagnosing CAA and assessing hemorrhage risk.
Key Fact #4: Amyloid Angiopathy Bleeds Have Distinctive Characteristics
Amyloid angiopathy bleeds have unique features that make them different from other brain hemorrhages. Knowing these differences is key to diagnosing and treating Cerebral Amyloid Angiopathy (CAA) well.
Up to 51% of CAA Patients Develop Intracranial Hemorrhage
People with CAA face a high risk of intracranial hemorrhage. This can lead to serious brain damage. Studies show that up to 51% of CAA patients may get intracranial hemorrhage, showing the need for close monitoring and care.
The risk of intracranial hemorrhage in CAA patients comes from amyloid beta in blood vessel walls. This weakens the vessels and changes their structure. As a result, the vessels are more likely to burst.
Correlation Between Bleeding Risk and Disease Severity
The bleeding risk and disease severity in CAA patients are closely linked. As CAA gets worse, the chance of bleeding goes up. This shows how amyloid buildup damages blood vessels.
A study found that more severe CAA increases the risk of bleeding. This highlights the need to check how severe CAA is when managing patients.
|
Disease Severity |
Bleeding Risk |
|---|---|
|
Mild |
Low |
|
Moderate |
Moderate |
|
Severe |
High |
Microbleed Progression to Symptomatic Hemorrhage
CAA patients often have microbleeds, small, painless hemorrhages seen on MRI. Over time, these microbleeds can turn into symptomatic hemorrhage, causing serious health problems.
Understanding how microbleeds turn into symptomatic hemorrhages is key in managing CAA. Finding out who is at high risk helps in taking steps to prevent severe bleeding.
In conclusion, the unique features of amyloid angiopathy bleeds, like the high risk of intracranial hemorrhage and the link between bleeding risk and disease severity, are vital in managing CAA. By recognizing these traits, healthcare providers can create better strategies to help patients.
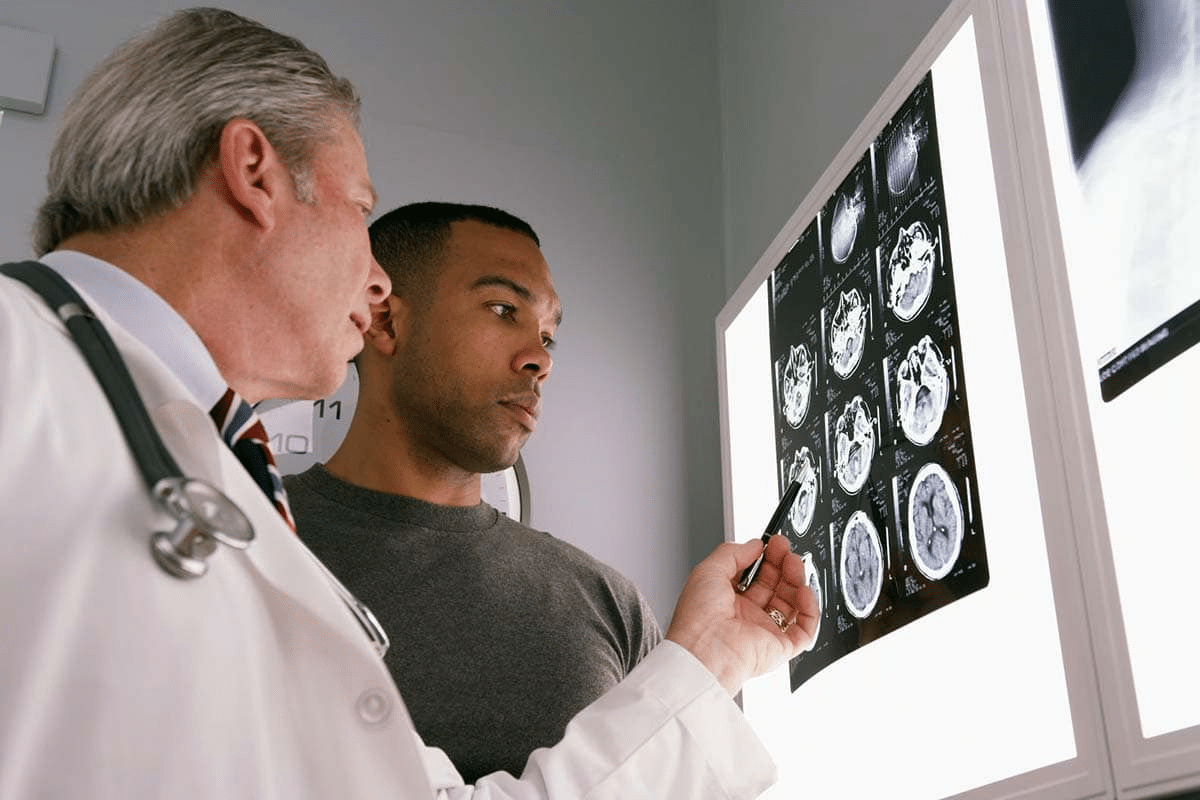
Key Fact #5: MRI Is the Gold Standard for Non-Invasive CAA Diagnosis
MRI has changed how we diagnose Cerebral Amyloid Angiopathy. It’s a non-invasive way to find the disease. MRI is key because it can spot signs of CAA well.
Strictly Lobar Microbleeds as Diagnostic Hallmarks
Lobar microbleeds are a key sign of CAA. MRI, with its gradient echo sequences, finds these microbleeds. They show up in the brain’s lobar areas, not like other conditions.
Lobar microbleeds are a main sign of CAA. Research shows that many of these microbleeds point to CAA. This is true when there’s no other reason for brain bleeding.
Cortical Superficial Siderosis: A Critical Diagnostic Marker
Cortical superficial siderosis (cSS) is also a key sign of CAA. It’s when hemosiderin builds up in the brain’s cortex. This happens after bleeding in the brain.
MRI is great at finding cSS. It looks like a dark line on T2-weighted images. Finding cSS means CAA is likely.
White Matter Hyperintensities and Other Associated Findings
MRI also shows other signs in CAA patients, like white matter hyperintensities (WMH). WMH are bright spots on T2-weighted images. They show damage to the white matter.
WMH can happen in many diseases, not just CAA. But with lobar microbleeds and cSS, WMH helps confirm CAA.
The Boston Criteria: Standardizing CAA Diagnosis
The Boston Criteria are a big step forward in diagnosing Cerebral Amyloid Angiopathy (CAA). They offer a clear guide, making CAA diagnosis more accurate and consistent everywhere.
Evolution of the Boston Criteria
The Boston Criteria were first made to standardize CAA diagnosis. They have changed over time, leading to both original and updated versions.
The original Boston Criteria set the stage with specific diagnostic categories. The modified Boston Criteria then improved these, thanks to new imaging and a deeper understanding of CAA.
Diagnostic Categories
The Boston Criteria divide CAA diagnosis into three main types: definite, probable, and possible. These are based on certain clinical and radiological signs.
|
Diagnostic Category |
Criteria |
|---|---|
|
Definite CAA |
Post-mortem examination confirming CAA |
|
Probable CAA |
Presence of strictly lobar hemorrhages and/or superficial siderosis, with supporting clinical and radiological features |
|
Possible CAA |
Presence of lobar hemorrhages or superficial siderosis, but with some uncertainty due to incomplete clinical or radiological information |
Sensitivity and Specificity Considerations
The Boston Criteria have been tested for their ability to accurately diagnose CAA. They are very specific but their sensitivity can change based on the group studied and the criteria used (original vs. modified).
It’s key for doctors to know the sensitivity and specificity of the Boston Criteria. This helps them understand diagnostic results better and make the best decisions for their patients.
Differential Diagnosis and Diagnostic Challenges
Diagnosing CAA can be tough because its symptoms can look like other brain diseases. To get it right, you need to know the unique signs of CAA and other similar conditions.
Distinguishing CAA from Hypertensive Arteriopathy
One big challenge is telling CAA apart from hypertensive arteriopathy. Both can cause small blood vessel problems in the brain. But, they have different causes and risks.
Key differences between CAA and hypertensive arteriopathy include:
- Location of microbleeds: CAA has lobar microbleeds, while hypertensive arteriopathy has deep or infratentorial ones.
- Underlying pathology: CAA is linked to amyloid in vessel walls, and hypertensive arteriopathy is caused by high blood pressure.
Other Causes of Cerebral Microbleeds
Other things can cause cerebral microbleeds too. This makes it important to figure out the exact cause. These include:
- Vasculitis
- Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)
- Other forms of amyloid angiopathy
To find the cause of microbleeds, a detailed check-up and imaging are key.
When to Consider Biopsy
At times, a brain biopsy is needed to confirm CAA. This is when other tests don’t give clear answers. A biopsy lets doctors see amyloid in the brain’s blood vessels directly.
Deciding on a biopsy must balance its risks and benefits. This depends on the patient’s health and how it might affect treatment.
Management Strategies and Treatment Considerations
Managing CAA is complex. It involves understanding risks of antithrombotic therapy, managing blood pressure, and exploring new treatments. Effective treatment balances risks and benefits of different options.
Antithrombotic Therapy Risks in CAA Patients
Antithrombotic therapy is common in heart disease. But for CAA patients, it raises the risk of bleeding in the brain. Studies show that anticoagulants can lead to severe brain bleeds in CAA patients.
“The risk of ICH associated with anticoagulant use in CAA patients highlights the need for careful consideration of antithrombotic therapy’s benefits and risks.” Doctors must consider the heart benefits against the risk of bleeding, mainly in those likely to have CAA.
Blood Pressure Management Guidelines
Managing blood pressure is key for CAA patients. High blood pressure increases the risk of brain bleeds. Keeping blood pressure in a target range helps prevent both brain bleeds and heart problems.
- Regular blood pressure checks are vital.
- Changes in lifestyle and medications may be needed.
- The right blood pressure target varies by patient.
Emerging Therapeutic Approaches
New research on CAA is promising. It focuses on reducing amyloid buildup, improving blood vessel function, and removing amyloid beta from the brain.
“Recent advances in understanding CAA have led to new treatments targeting the disease’s causes.”
New treatments may offer hope for CAA patients. They could lower the risk of brain bleeds and slow disease progress. Ongoing trials will show if these treatments are safe and effective.
Conclusion: Implications for Clinical Practice and Future Research
Cerebral Amyloid Angiopathy is a complex condition. It has big implications for how we practice medicine and for future research. Knowing how CAA works, how to diagnose it, and how to manage it is key to better patient care.
Diagnosing CAA often depends on MRI scans. These scans show lobar microbleeds and cortical superficial siderosis. The Boston Criteria help standardize diagnosis. But, it’s hard to tell CAA apart from other causes of cerebral microbleeds.
In treating patients, it’s important to know CAA’s link to Alzheimer’s disease and its role in bleeding in the brain. This knowledge helps doctors decide on treatments like blood thinners and controlling blood pressure. Future studies should look into new ways to lower the risk of bleeding in CAA patients. They should also explore the connection between CAA and cerebral amyloidosis.
More research on CAA will help us understand it better. This will lead to better ways to diagnose and treat it. It will guide how we practice medicine and shape future research in cerebral amyloidosis.
FAQ
What is Cerebral Amyloid Angiopathy (CAA)?
Cerebral Amyloid Angiopathy (CAA) is a condition where amyloid beta builds up in blood vessel walls. This weakens the vessels and changes their structure.
What are the primary risk factors for developing CAA?
The main risk factor for CAA is age. The risk grows as people get older.
How is CAA related to Alzheimer’s disease?
CAA is closely linked to Alzheimer’s disease. They share similar causes and are common in Alzheimer’s patients. Studies show 48% of Alzheimer’s patients have CAA based on pathology, and 22% based on MRI.
What is the role of CAA in lobar intracerebral hemorrhage?
CAA is a big cause of lobar intracerebral hemorrhage. It’s responsible for 50-57% of cases. The location and pattern of hemorrhage are influenced by CAA.
How is CAA diagnosed using MRI?
MRI is the best way to diagnose CAA without surgery. It looks for specific signs like lobar microbleeds and cortical superficial siderosis.
What are the Boston Criteria for CAA diagnosis?
The Boston Criteria help doctors diagnose CAA. They use clinical and MRI findings to categorize cases as definite, probable, or possible. There are both original and modified versions.
How is CAA distinguished from other causes of cerebral microbleeds?
CAA is different from other causes of cerebral microbleeds. It’s based on where and how the microbleeds appear, along with clinical and MRI findings.
What are the management strategies for CAA?
Managing CAA involves careful thought about antithrombotic therapy risks. It also includes managing blood pressure and exploring new treatments.
Can CAA be treated?
There’s no cure for CAA, but doctors can manage it. They aim to reduce the risk of bleeding and slow the disease’s progress.
What is the significance of cerebral amyloid angiopathy MRI findings?
MRI findings like lobar microbleeds and cortical superficial siderosis are key for diagnosing CAA. They help understand how severe the disease is.
How does CAA affect cerebral blood vessels?
CAA causes amyloid beta to build up in blood vessel walls. This weakens the vessels and changes their structure, raising the risk of bleeding.
Reference
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6501479/