Last Updated on December 2, 2025 by Bilal Hasdemir
Did you know over 100,000 people in the U.S. have colon removal surgery every year? A colectomy is a big surgery that removes part or all of the colon. It’s important for patients to know why this surgery is needed.
Thinking about having a colectomy can be scary. But, this surgery is often needed to fix colon problems. By looking into why a colectomy is done, we can understand its role in treating health issues.
We will look into the details of when a colectomy is needed. We aim to give a full picture of why this surgery is done. This way, patients can make informed choices about their health.
Our critical list of colectomy surgery indications. Discover the top medical reasons, from cancer to IBD, why this surgery is recommended.
Key Takeaways
- Colectomy is a significant surgical procedure involving the removal of part or all of the colon.
- Various colon-related health issues may necessitate a colectomy.
- Understanding the indications for colectomy is key for patients facing this decision.
- The decision to undergo a colectomy is influenced by many factors.
- Patients should be empowered with knowledge to make informed decisions about their care.
Understanding Colectomy: Definition and Purpose
A colectomy is a major surgery that removes part or all of the colon. This is a key part of our digestive system. Knowing what a colectomy is and the colon’s role in health is important.
What is a Colectomy?
A colectomy means removing the colon or a part of it. It’s done for many reasons, like treating colon cancer or inflammatory bowel disease. The amount of colon removed depends on the condition and how severe it is.
Anatomy of the Colon and Its Function
The colon, or large intestine, is vital for digestion. It absorbs water and salts from food, storing waste until it’s eliminated. It has sections like the ascending and descending colon, each playing a role in digestion.
Knowing the colon’s anatomy and function helps understand why a colectomy might be needed. It also shows how it can affect a person’s life.
Types of Colectomy Procedures
It’s important for patients to know about the different colectomy procedures. Each surgery is tailored to treat various colon conditions. The type of surgery depends on the disease’s extent and location.
Total Colectomy
A total colectomy removes the entire colon. It’s often for severe cases like ulcerative colitis or FAP. Total colectomy is considered when the disease affects the entire colon, and other treatment options have been exhausted.
A medical expert notes, “Total colectomy can significantly improve the quality of life for patients with severe colon disease, but it requires careful consideration and planning.”
“The decision to undergo a total colectomy should be made after thorough evaluation and discussion with a healthcare provider.”
Partial Colectomy
Partial colectomy removes a part of the colon. It’s used for colon cancer, diverticulitis, or Crohn’s disease in a specific area. The goal is to remove the diseased part while keeping as much colon as possible.
Hemicolectomy (Right and Left)
Hemicolectomy removes one half of the colon. There are right and left hemicolectomies. Hemicolectomy is often for colon cancer or diseases affecting one side of the colon.
| Type of Hemicolectomy | Colon Section Removed | Common Indications |
| Right Hemicolectomy | Right side of the colon | Colon cancer, Crohn’s disease |
| Left Hemicolectomy | Left side of the colon | Colon cancer, diverticulitis |
Sigmoid Colectomy
Sigmoid colectomy removes the sigmoid colon, the lower part of the colon. It’s for sigmoid colon cancer, diverticulitis, or diseases in this area. Sigmoid colectomy aims to remove the diseased sigmoid colon while maintaining the integrity of the remaining colon.
In conclusion, the type of colectomy procedure depends on the disease’s specifics. Knowing these types helps patients understand their treatment options better.
Colectomy Surgery Indications: When Is It Necessary?
Understanding when colectomy surgery is needed involves looking at several key factors. Colectomy is a surgery to remove part or all of the colon. It’s used for various medical conditions that affect the large intestine.
Overview of Medical Conditions Requiring Colectomy
Several gastrointestinal diseases and disorders may need a colectomy. These include:
- Colon Cancer: Colectomy is a main treatment for colon cancer. It aims to remove the tumor and affected colon part.
- Inflammatory Bowel Disease (IBD): Conditions like ulcerative colitis and Crohn’s disease may need colectomy if other treatments fail or if complications arise.
- Diverticulitis: Complicated diverticulitis, with recurring inflammation, abscesses, or perforation, may need surgery.
- Bowel Obstruction: A significant blockage of the intestine may require colectomy to remove the blocked segment.
Emergency vs. Elective Colectomy
Colectomy surgeries are either emergency or elective. Emergency colectomies are for acute conditions like bowel perforation, severe bleeding, or toxic megacolon. Elective colectomies are planned for conditions that are not life-threatening right away, allowing for better preparation.
The difference between emergency and elective colectomy is key. It affects preoperative care, surgical approach, and postoperative recovery.
Determining Factors for Surgical Intervention
Several factors decide if surgery is needed for colon-related conditions. These include:
- Severity of Symptoms: The intensity of symptoms like pain, bleeding, or obstruction affects the surgery decision.
- Response to Medical Therapy: If medical treatment fails or complications arise, surgery may be needed.
- Presence of Complications: Complications like abscesses, perforation, or significant bleeding often require emergency surgery.
- Cancer Diagnosis: A colon cancer diagnosis usually means the tumor needs to be surgically removed.
Healthcare providers consider these factors to decide if colectomy surgery is right for a patient. They balance the surgery’s benefits with its risks and complications.
Colectomy for Colon Cancer Treatment
Removing part or all of the colon is called colectomy. It’s a common treatment for colon cancer, tailored for each patient. Colon cancer is a common cancer worldwide, and surgery is key in treating it.
Stages of Colon Cancer Requiring Surgery
Colectomy is usually needed for stages I, II, and III colon cancer. For stage I, surgery might cure the cancer. For stages II and III, surgery is often paired with chemotherapy.
The American Cancer Society says surgery is the main treatment for colon cancer. The surgery type depends on the cancer’s stage and location. The five-year survival rate for colon cancer is much higher if caught early, showing the need for early surgery.
| Stage | Description | Treatment Approach |
| Stage I | Cancer is limited to the colon wall | Surgery alone |
| Stage II | Cancer has grown through the colon wall | Surgery, possibly followed by chemotherapy |
| Stage III | Cancer has spread to nearby lymph nodes | Surgery combined with chemotherapy |
Surgical Approaches Based on Tumor Location
The tumor’s location in the colon affects the surgery. Tumors on the right side get a right hemicolectomy. Tumors on the left might need a left hemicolectomy or sigmoid colectomy.
A surgical oncologist notes, “New surgical methods like laparoscopic or robotic surgery have improved outcomes. They reduce recovery time and lower complication rates.”
Lymph Node Removal Considerations
Removing lymph nodes is key in colon cancer surgery. The number of nodes removed affects staging and treatment plans.
“Adequate lymph node retrieval is essential for accurate staging and may have therapeutic implications,” according to a study published in a surgical oncology journal.
It’s important to remove and analyze enough lymph nodes. This helps determine how far the cancer has spread and guides further treatment.
Inflammatory Bowel Disease and Colectomy
Inflammatory bowel disease (IBD) can really affect a person’s life. It includes conditions like ulcerative colitis and Crohn’s disease. These can cause a lot of pain and discomfort because of inflammation in the gut.
If treatments don’t work or if problems get worse, a colectomy might be needed. This is a serious surgery to remove part of the colon.
Colectomy for Ulcerative Colitis
Ulcerative colitis mainly affects the colon. If treatments don’t help or if there are serious problems like cancer, surgery might be suggested. Doctors look at how bad the disease is and how it affects the patient’s life.
Usually, the whole colon is removed. This can really help improve symptoms and quality of life.
- Indications for Colectomy:Failure of medical therapy to control symptoms
- Development of dysplasia or cancer
- Severe complications such as toxic megacolon
Colectomy for Crohn’s Disease Treatment
Crohn’s disease can affect any part of the gut but often hits the end of the small intestine and colon. Surgery isn’t a cure, but it might be needed to handle serious problems or when treatments don’t work.
Choosing to have a colectomy for Crohn’s disease is a big decision. Doctors consider how bad the disease is, past surgeries, and how it affects the patient’s life. The surgery might be partial or total, depending on the disease’s spread.
- Key Considerations:
- Extent of disease
- Previous surgical interventions
- Potential for recurrence
Knowing about colectomy in IBD helps patients and doctors decide when surgery is the best choice.
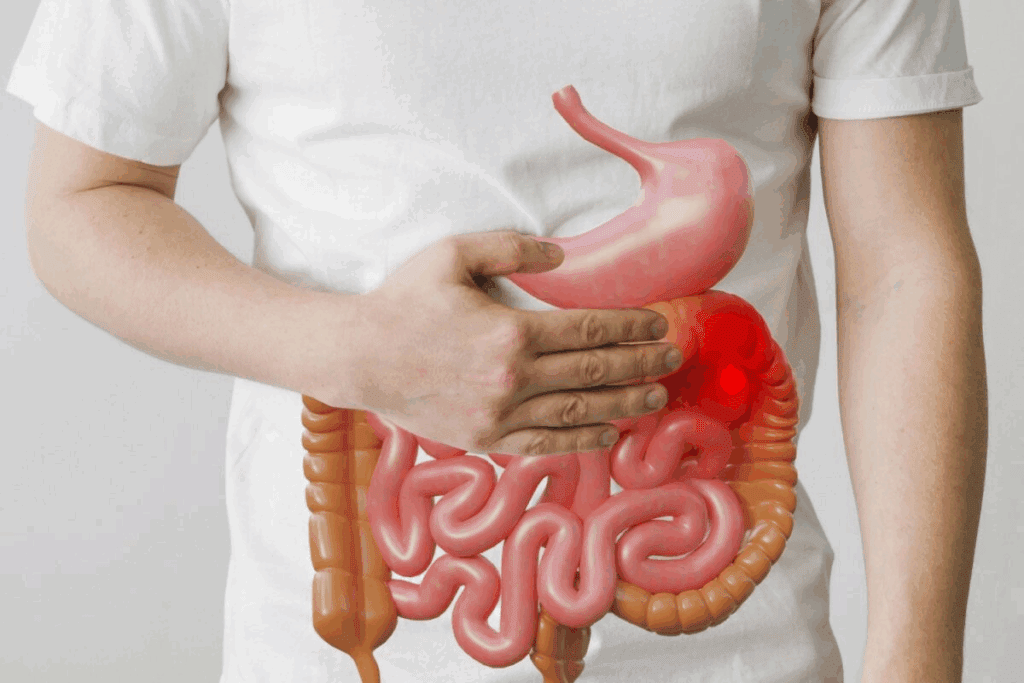
Diverticulitis as an Indication for Colectomy
Diverticulitis, a serious form of the condition, may need a colectomy. This is when a part of the colon is removed. It happens when small pouches in the colon wall get inflamed. This can lead to serious problems that need surgery.
Acute vs. Chronic Diverticulitis
Diverticulitis can be sudden or ongoing. Acute diverticulitis comes on quickly, causing severe pain, fever, and changes in bowel habits. Most cases are treated with antibiotics and care. But, if there are abscesses, perforation, or narrowing, surgery is needed.
Chronic diverticulitis is when the inflammation keeps coming back. People with this may have ongoing symptoms or keep getting acute diverticulitis. A colectomy might be an option to stop future problems and ease symptoms.
Complicated Diverticulitis Requiring Surgery
Complicated diverticulitis is when the inflammation causes big problems. These can include:
- Abscess formation
- Perforation of the colon
- Fistula formation
- Stricture or significant narrowing of the colon
When these problems happen, a colectomy is often needed. This is to remove the sick part of the colon. Surgery is usually considered after other treatments fail or if the condition is very dangerous.
| Complication | Description | Surgical Consideration |
| Abscess | A collection of pus due to infection | Drainage may be attempted first; colectomy if recurrent |
| Perforation | A hole in the colon wall, leading to leakage | Urgent colectomy often required |
| Fistula | An abnormal connection between the colon and another organ or the skin | Colectomy to remove the fistulous tract |
| Stricture | Narrowing of the colon, potentially causing bowel obstruction | Colectomy to remove the narrowed segment |
Surgery can seem scary. But for complicated diverticulitis, it can save lives. It removes the problem and helps the patient get better and go back to normal life.
Bowel Obstruction and Colectomy Surgery
When the bowel gets blocked, it can cause serious problems. Sometimes, a colectomy is needed to fix the blockage. Bowel obstruction happens when the intestine’s flow is blocked, either a bit or completely.
Causes of Intestinal Blockage
There are many reasons why the intestine might get blocked. We find out the cause to choose the right treatment.
- Tumors: Both good and bad tumors can block the intestine by physically getting in the way.
- Adhesions: Scar tissue from surgery or inflammation can twist or kink the intestine.
- Hernias: When a part of the intestine bulges through a weak spot in the belly, it can cut off blood and block the intestine.
- Inflammatory bowel disease: Diseases like Crohn’s can narrow the intestine, causing blockage.
Colectomy for Intestinal Blockage Relief
A colectomy might be needed to fix the blockage and get the bowel working right again. The choice to do a colectomy depends on the blockage’s cause and how bad it is.
We look at a few things to decide if a colectomy is needed. These include where and how bad the blockage is, the patient’s health, and if there are any other problems.
Partial vs. Complete Obstruction Management
How we manage bowel obstruction changes based on if it’s partial or complete. Knowing the difference is key for the right treatment.
| Obstruction Type | Characteristics | Treatment Approach |
| Partial Obstruction | Some intestinal contents can pass through | May be managed conservatively with bowel rest and monitoring, or may require surgery |
| Complete Obstruction | No intestinal contents can pass through | Typically requires urgent surgical intervention, such as colectomy, to relieve the obstruction |
By understanding bowel obstruction causes and the role of colectomy, we can offer good treatment options for those affected.
Emergency Colectomy for Life-Threatening Conditions
Life-threatening colon issues need quick surgery, known as an emergency colectomy. This urgent action is key to avoid more problems and save lives.
Bowel Perforation Treatment
A bowel perforation is a serious issue where a hole forms in the intestine. This lets bacteria and other stuff leak into the belly. It can cause severe infection and needs fast surgery.
Key aspects of bowel perforation treatment include:
- Prompt diagnosis through imaging studies
- Antibiotic therapy to control infection
- Surgical repair or removal of the affected segment
Toxic Megacolon
Toxic megacolon is a dangerous condition where the colon gets very big. It’s often linked to inflammatory bowel disease or infection. It needs quick medical and surgical help.
Treatment strategies for toxic megacolon include:
- Aggressive medical management with antibiotics and bowel rest
- Close monitoring for signs of deterioration
- Surgical intervention, such as colectomy, in refractory cases
Massive Hemorrhage
A massive hemorrhage in the GI tract is very dangerous and might need emergency colectomy. The cause can be many things, like diverticulosis or cancer.
Management of massive hemorrhage involves:
- Rapid resuscitation with fluids and blood products
- Localization of the bleeding source through endoscopy or imaging
- Surgical intervention to control the bleeding
Ischemic Bowel
Ischemic bowel happens when the intestines don’t get enough blood, causing damage. Severe cases might need emergency colectomy to remove the damaged part.
Critical factors in managing ischemic bowel include:
- Early recognition of symptoms
- Restoration of blood flow when possible
- Surgical resection of non-viable bowel segments
In conclusion, emergency colectomy is a critical surgery for serious colon problems. Quick action is vital to improve patient outcomes in these urgent cases.
Colectomy for Polyps and Precancerous Conditions
When polyps are too big or complex, or if there’s a high cancer risk, a colectomy might be needed. This can be scary, but we’re here to help you understand what’s happening.
When Polyps Cannot Be Removed Endoscopically
Some polyps are too big or complex for endoscopic removal. In these cases, surgery to remove part of the colon might be necessary. This often applies to large sessile polyps that are hard to remove safely.
We look at several things to decide if a colectomy is needed. These include:
- The size and location of the polyp
- The presence of dysplasia or cancer within the polyp
- The patient’s overall health and surgical risk
Large Sessile Polyps
Large sessile polyps are flat and wide, making endoscopic removal risky. A colectomy can remove the polyp and any cancerous tissue. We use advanced tools to check the polyp and decide the best course.
Dysplasia in Inflammatory Bowel Disease
People with IBD, like ulcerative colitis or Crohn’s disease, face a higher risk of dysplasia and cancer. Regular checks are key, and a colectomy might be needed to stop cancer. We closely monitor patients and decide on surgery timing together.
Managing dysplasia in IBD involves:
- The extent and duration of the IBD
- The presence and grade of dysplasia
- The patient’s response to medical therapy
Prophylactic Colectomy for Polyposis Syndromes
People with genetic syndromes like Familial Adenomatous Polyposis (FAP) face a high cancer risk. A prophylactic colectomy can prevent cancer. We offer genetic counseling and support to help patients make informed choices.
Understanding the risks and benefits of colectomy helps patients make informed decisions. We’re dedicated to providing personalized care and support every step of the way.
Genetic Disorders Requiring Preventive Colectomy
People with certain genetic conditions are at higher risk of colon cancer. This makes talking about preventive colectomy very important. Conditions like Familial Adenomatous Polyposis (FAP) and Lynch syndrome greatly raise the risk of colon cancer. We will look at these conditions and how preventive colectomy helps manage this risk.
Familial Adenomatous Polyposis (FAP)
FAP is a rare genetic disorder. It causes hundreds to thousands of polyps in the colon and rectum. Without treatment, people with FAP almost surely get colon cancer by age 40. Preventive colectomy is the main treatment for FAP to stop colon cancer.
Lynch Syndrome (HNPCC)
Lynch syndrome, also known as Hereditary Nonpolyposis Colorectal Cancer (HNPCC), raises the risk of colon cancer. People with Lynch syndrome are more likely to get colon cancer and other cancers like endometrial and ovarian cancer. The choice of preventive colectomy in Lynch syndrome is more complex. It depends on the person’s cancer risk and family history.
Timing of Prophylactic Surgery
The timing of prophylactic surgery is key for genetic disorders like FAP and Lynch syndrome. For FAP patients, prophylactic colectomy is usually suggested in the teenage years or early twenties. For Lynch syndrome, the decision for preventive colectomy is more complex. It’s based on the individual’s cancer risk and family history.
Quality of Life Considerations
Preventive colectomy can change a person’s quality of life. It can involve an ostomy, changes in bowel function, and the emotional impact of surgery. We work with patients to understand these effects. This helps them make informed decisions about their care.
| Genetic Disorder | Colon Cancer Risk | Preventive Colectomy Recommendation |
| FAP | Nearly 100% by age 40 | Typically recommended during teenage years or early twenties |
| Lynch Syndrome | Significantly increased, but variable | Considered on a case-by-case basis |
High-Risk Cases and Special Considerations
High-risk cases, like elderly patients and those with many health issues, face unique challenges in colectomy surgery. They need careful evaluation and management to lower risks and improve results.
Elderly Patients
Elderly patients face higher risks in colectomy due to age-related health decline, other health conditions, and possible brain issues. Preoperative assessment should include a detailed geriatric evaluation. This helps identify risks and find ways to reduce them.
Multiple Comorbidities
Patients with many health problems, like heart disease, diabetes, or COPD, need special care before, during, and after surgery. Multidisciplinary care involving surgeons, anesthesiologists, and other experts is key. It helps improve these patients’ health and lowers surgery risks.
Immunocompromised Patients
Patients with weakened immune systems, due to medication, disease, or other reasons, are at higher risk of infections and complications after surgery. Perioperative antibiotic prophylaxis and watching for infection signs are vital in managing these patients.
Colectomy as a Last Resort Treatment
In some cases, colectomy is considered only when other treatments have failed or are not possible. This choice weighs the benefits against the risks, considering the patient’s quality of life. It also involves talking with the patient and their family about the implications.
Understanding the complexities and challenges of high-risk colectomy cases helps healthcare providers manage these patients better. This improves their outcomes.
Preparing for Colectomy Surgery
Getting ready for colectomy surgery can make you feel less anxious and improve your results. We know surgery is scary, but we’re here to help you through every step. We want to make sure you’re comfortable and prepared.
Preoperative Testing and Evaluation
We do many tests and checks before your surgery to make sure you’re ready. This includes blood tests, scans like CT or MRI, and looking at your health history. We aim to find any risks and make your health the best it can be before surgery.
“The preoperative evaluation is key for a successful colectomy surgery,” says Dr. [Last Name], a top colorectal surgeon. “By checking your health and fixing any issues, we lower the chance of problems.”
Bowel Preparation Protocols
Getting your bowel ready for surgery is very important. You’ll follow a special diet, use laxatives, and might take antibiotics. We’ll give you all the details on how to get your bowel ready, so you feel confident and comfortable.
- Dietary changes to reduce residue
- Laxatives to empty your bowel
- Antibiotics to prevent infection
Nutritional Optimization
Eating well is also key before your surgery. We suggest a diet full of nutrients to help your health and recovery. Good nutrition is important for healing and getting better after surgery.
| Nutrient | Food Sources | Benefits |
| Protein | Lean meats, fish, eggs, legumes | Helps with healing and recovery |
| Fiber | Fruits, vegetables, whole grains | Good for your digestive system |
What to Expect Before Surgery
We’ll give you all the details on what to do before your surgery. This includes how to manage your meds, when to arrive, and what to bring. We want to make sure you’re ready and comfortable every step of the way.
By following these steps and working with our team, you’ll be well-prepared for your surgery. We’re here to support you, giving you the care and advice you need for the best results.
Surgical Approaches and Techniques
Surgical methods for colectomy have grown, giving patients many options. The right technique depends on the condition, disease extent, and patient health.
Traditional Open Colectomy
Traditional open colectomy uses a big incision in the belly. It lets the surgeon see and work on the colon directly.
Benefits: It’s good for complex cases, allowing for direct handling of tissues.
Drawbacks: It leaves a big wound, leading to longer healing times and more risks.
Laparoscopic Colectomy
Laparoscopic colectomy, or minimally invasive surgery, uses small incisions. A laparoscope and tools are inserted through these small cuts.
Benefits: It causes less damage, less pain, and faster healing. Patients often leave the hospital sooner.
Drawbacks: It needs special training for surgeons. Not all patients are good candidates due to past surgeries or complex diseases.
Robotic-Assisted Colectomy
Robotic-assisted colectomy is a laparoscopic surgery upgrade. It uses a robotic system to improve the surgeon’s skills. This method offers better precision and control.
Benefits: It gives better views, precision, and flexibility. It might lead to less blood loss and fewer problems.
Drawbacks: It needs special equipment and training. It can also be more expensive than other methods.
Single-Incision Laparoscopic Surgery
Single-incision laparoscopic surgery is done through one incision, usually in the belly button. It aims to make the surgery even less invasive.
Benefits: It might leave less scarring, less pain, and faster healing.
Drawbacks: It’s technically hard, with a longer learning curve for surgeons. It’s not right for all patients or complex cases.
| Surgical Approach | Benefits | Drawbacks |
| Traditional Open Colectomy | Direct visualization, straightforward for complex cases | Larger wound, longer recovery, increased risk of complications |
| Laparoscopic Colectomy | Less invasive, reduced pain, quicker recovery | Specialized training required, not suitable for all patients |
| Robotic-Assisted Colectomy | Enhanced precision, less blood loss, fewer complications | Specialized equipment and training, potentially more costly |
| Single-Incision Laparoscopic Surgery | Less visible scarring, reduced postoperative pain | Technically challenging, not suitable for complex cases |
Risks and Complications of Colectomy
Colectomy, like any major surgery, has risks and complications. We aim to make the surgery safe and smooth. But knowing these risks helps patients make informed choices.
Short-Term Complications
Short-term complications happen during or right after surgery. These include:
- Infection: Surgery can lead to infection. We take strict measures to prevent this.
- Bleeding: Too much bleeding is a possible complication.
- Adhesions: Fibrous tissue can form between organs or the abdominal wall.
- Bowel obstruction: The intestine can get blocked by adhesions or other reasons.
- Anastomotic leakage: There’s a risk of leakage at the junction of joined colon sections.
We watch patients closely for these issues and act quickly if they happen.
Long-Term Complications
Long-term complications can show up weeks, months, or years later. Some are:
- Permanent ostomy: Some patients need a permanent ostomy bag after surgery.
- Bowel function changes: Bowel habits can change, leading to diarrhea or constipation.
- Nutritional deficiencies: Without the colon, some nutrients are harder to absorb.
- Hernias: Hernias can form at surgical sites due to weak spots in the abdominal wall.
Following post-op instructions and attending follow-ups is key to catching long-term issues early.
While colectomy comes with risks, many patients do well without major problems. Our team works hard to reduce risks and support patients during recovery.
Recovery and Life After Colectomy
Recovering from colectomy surgery is a journey with many steps. It includes both immediate care after surgery and making lifestyle changes. We’ll help you understand what to expect during recovery. This includes immediate care, long-term lifestyle changes, diet adjustments, and living with an ostomy.
Immediate Post-Operative Period
The first days after surgery are very important. Patients usually stay in the hospital for a few days. Our team watches for any problems, manages pain, and helps you move to prevent blood clots.
Pain Management is key. We use medicines and other methods to keep you comfortable. Early mobilization helps avoid serious issues like deep vein thrombosis.
Long-term Lifestyle Adjustments
After leaving the hospital, you’ll need to make big changes in your life. These changes help you stay healthy and improve your quality of life. We guide you on how to slowly get back to normal activities, like work and exercise, but avoid heavy lifting.
Managing your diet is also important. We help you adjust your eating habits to fit your new needs.
Dietary Modifications
Your diet is very important for recovery and long-term health. We suggest a diet that’s easy to digest, full of nutrients, and meets your specific needs. This might mean eating smaller meals more often, avoiding foods that upset your stomach, and drinking plenty of water.
| Dietary Recommendation | Benefit |
| Eating smaller, frequent meals | Reduces strain on the digestive system |
| Avoiding high-fiber foods initially | Minimizes discomfort and complications |
| Adequate hydration | Supports overall health and digestion |
Living with an Ostomy
Some people need an ostomy after surgery. With the right support, living with an ostomy can be fulfilling. We teach you how to care for your ostomy, including managing the bag, skin care, and daily life with an ostomy.
Conclusion
We’ve looked at why colectomy surgery is needed for many colon issues. This surgery helps treat colon cancer, inflammatory bowel disease, and more. It’s also used for diverticulitis, bowel obstructions, and genetic disorders.
Knowing when a colectomy is needed is key. Doctors decide on surgery after checking the patient’s health carefully. This ensures the surgery is the right choice.
In short, a colectomy greatly improves life for those with severe colon problems. We’ve covered the main reasons for this surgery. This should help you understand its importance and what to expect.
Colectomy is used for many different reasons, and it’s customized for each patient. It can be urgent or planned. Either way, it needs careful planning and care after the surgery.
FAQ
What is a colectomy, and why is it performed?
A colectomy is a surgery where part or all of the colon is removed. It treats conditions like colon cancer, inflammatory bowel disease, and diverticulitis. It’s also used for life-threatening issues like bowel perforation or massive bleeding.
What are the different types of colectomy procedures?
There are several colectomy procedures. These include total colectomy, partial colectomy, and hemicolectomy (right and left). The choice depends on the condition and how far the disease has spread.
When is a colectomy considered an emergency surgery?
A colectomy is urgent for life-threatening issues. This includes bowel perforation, toxic megacolon, massive hemorrhage, or ischemic bowel. These need immediate surgery to avoid serious problems or death.
Can a colectomy be performed for colon cancer treatment?
Yes, a colectomy is a common treatment for colon cancer. The surgery aims to remove the tumor and nearby tissue. It also removes lymph nodes to stop cancer spread.
How does a colectomy help in managing inflammatory bowel disease?
A colectomy can manage inflammatory bowel disease. It removes the diseased colon part. This can reduce symptoms, lower medication use, and improve life quality.
What is the role of colectomy in treating diverticulitis?
A colectomy treats complicated diverticulitis. This includes abscesses, perforations, or narrowing. Surgery removes the affected area to prevent future issues.
Can a colectomy relieve bowel obstruction?
Yes, a colectomy can relieve bowel obstruction. It removes the blockage or affected colon part. This restores normal bowel function and eases symptoms.
What are the risks and complications associated with colectomy surgery?
Colectomy surgery has risks like infection, bleeding, and adhesions. There’s also a chance of bowel obstruction and ostomy complications. Patients should talk to their healthcare provider about these risks.
How do I prepare for colectomy surgery?
Preparing for colectomy surgery includes tests, bowel prep, and nutrition planning. Patients should follow their healthcare provider’s instructions to prepare well.
What can I expect during the recovery period after a colectomy?
The recovery after a colectomy involves post-operative care and lifestyle changes. Patients need to manage pain, watch for complications, and make dietary adjustments. They might also need to adapt to living with an ostomy.
Are there any special considerations for high-risk patient groups undergoing colectomy?
Yes, high-risk patients, like the elderly or those with many health issues, need special care. They may need closer monitoring and tailored treatment to reduce risks and complications.
Can genetic disorders increase the risk of colon cancer, and is a colectomy recommended?
Yes, genetic disorders like Familial Adenomatous Polyposis (FAP) and Lynch Syndrome raise colon cancer risk. A prophylactic colectomy might be suggested to prevent cancer in these cases.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9839829/