Did you know thousands of people have colon removal surgery each year? A colectomy is a big surgical procedure that removes part or all of the colon. It’s needed when the colon gets sick or hurt. Our colorectal surgery clinic offers detailed care for those needing this complex surgery.
Having a colectomy can feel scary. Our team is here to help you at every step. We’ll guide you from learning about colectomy cancer treatment surgery to getting better after it. This surgery is key for treating colon cancer, Crohn’s disease, and diverticulitis.
The ultimate guide to the colectomy surgical procedure. Learn the different types, what happens during surgery, and essential recovery info.
Key Takeaways
- A colectomy involves removing the diseased portion of the colon.
- This surgery is often necessary for colon cancer, Crohn’s disease, and diverticulitis.
- Patients benefit from comprehensive care throughout the colectomy process
- Understanding the procedure can help ease worries and prepare patients for recovery.
- We help our patients through every part of the colectomy process.
Understanding Colectomy: Definition and Overview
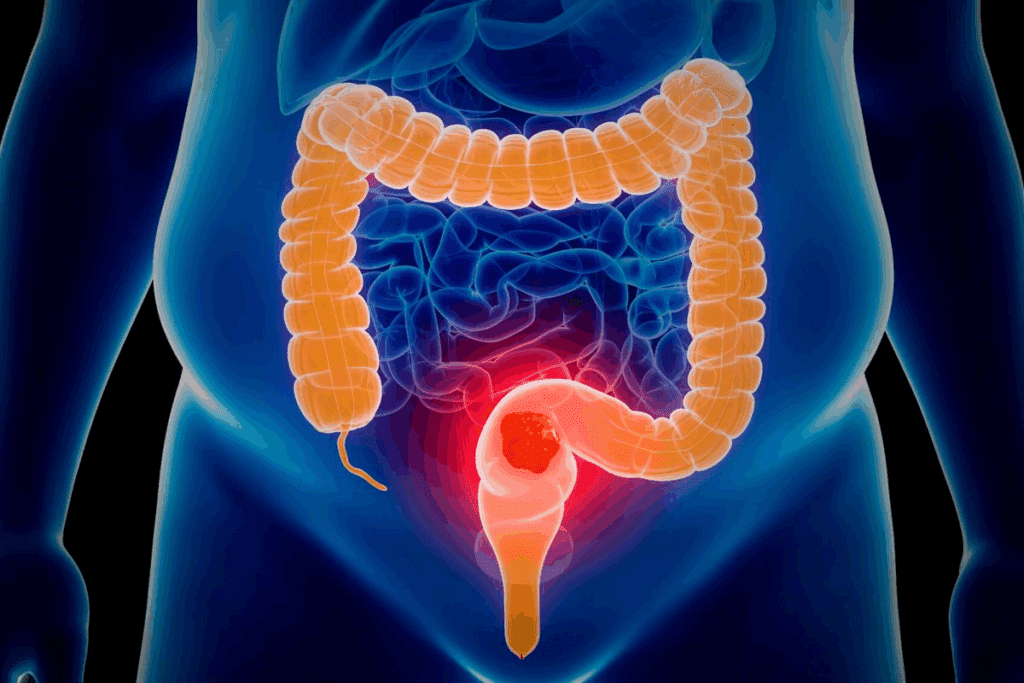
To understand colectomy, we must first look at the colon’s anatomy and its role in digestion. The colon, or large intestine, is key in absorbing water and electrolytes. It also helps form stool.
The Anatomy of the Colon and Its Function
The colon is a vital part of our digestive system. It absorbs water and electrolytes from waste material coming from the small intestine. It’s about 5 feet long and has different sections like the ascending, transverse, descending, and sigmoid colon.
The colon’s muscular walls help move waste through our body. This process is called peristalsis. It also hosts a variety of microorganisms, or gut microbiome, which is important for our health.
| Colon Section | Function |
| Ascending Colon | Absorbs water and electrolytes |
| Transverse Colon | Continues absorption and moves waste |
| Descending Colon | Stores waste until it is eliminated |
| Sigmoid Colon | Connects to the rectum, facilitating waste elimination |
Basic Definition of Colectomy Surgery
A colectomy is a surgery that removes the diseased or damaged part of the colon. It can be done in open or minimally invasive ways. The main goal is to remove the affected area while keeping as much colon function as possible.
Colectomy is often needed for issues like colorectal cancer, inflammatory bowel disease, and diverticulitis. Knowing about the colon’s anatomy and colectomy surgery helps patients understand its complexity.
The Colectomy Surgical Procedure Explained
A colectomy is a surgery that removes part or all of the colon. It needs careful planning before, during, and after the surgery. The operation is done under general anesthesia to keep the patient comfortable.
Pre-Operative Preparation
Before a colectomy, patients get many tests and medical checks. These include blood tests, imaging like CT scans, and a look at their medical history. They also learn about diet and bowel prep to lower infection risk.
Getting ready for surgery can be tough. Our medical team offers full support and advice. We make sure patients know what to expect and are ready for their surgery.
During the Operation: What Happens in the Operating Room
In the surgery, the surgeon takes out the bad part of the colon. They try to keep the good parts safe. The surgery can be open, laparoscopic, or robotic, based on the patient and surgeon.
The type of surgery affects how well the patient recovers. Our surgeons choose the best method for each patient.
Post-Operative Care in the Hospital
After surgery, patients are watched closely in the hospital. They get help with pain and learn about diet and follow-up care. The team also checks for any problems.
| Aspect of Care | Description | Benefits |
| Pain Management | Effective pain relief strategies | Enhanced patient comfort |
| Dietary Advice | Guidance on post-operative diet | Promotes healing and recovery |
| Follow-up Care | Schedule follow-up appointments | Ensures recovery is on track |
We focus on caring for patients from start to finish. Our team aims to give the best results after a colectomy surgery.
Types of Colectomy Procedures
There are many types of colectomy procedures. Each one is for different medical needs. The choice depends on the disease’s location and the patient’s health.
Total Colectomy
A total colectomy removes the whole colon. It’s needed for diseases like ulcerative colitis or familial adenomatous polyposis. Total colectomy colon removal is a big surgery that needs careful thought and preparation.
Partial Colectomy
A partial colectomy takes out only the diseased part of the colon. It’s often used for colon cancer or diverticulitis. This partial colectomy surgical option is chosen when the disease is in one area.
Hemicolectomy
A hemicolectomy removes half of the colon. It’s for cancers or diseases on one side. The surgery tries to keep as much colon as possible.
Sigmoid Colectomy
A sigmoid colectomy removes the sigmoid colon, near the rectum. It’s for cancers or severe diverticulitis in this area.
Knowing about the types of colectomy surgery helps patients and doctors choose the best surgery. It’s based on the patient’s condition and needs.
Surgical Approaches to Colectomy
There are different ways to do colectomy surgery. You can choose from open, laparoscopic, or robotic-assisted methods. The right choice depends on your health, the problem being treated, and the surgeon’s skills.
Open Colectomy
Open colectomy uses a big cut in the belly to reach the colon. It’s good for complex cases but causes more damage and takes longer to heal. It’s often used when other methods can’t be done.
Laparoscopic Colectomy
Laparoscopic colectomy is a minimally invasive surgery. It uses small cuts and special tools to work inside. This method hurts less and you heal faster. It’s best for those who can handle minimally invasive surgery.
Robotic-Assisted Colectomy
Robotic-assisted colectomy is a high-tech version of minimally invasive surgery. It uses a robotic system for better control and precision. This can lead to better results and fewer problems. It’s great for those who need precise and less invasive surgery.
| Surgical Approach | Incision Size | Recovery Time | Precision |
| Open Colectomy | Large | Longer | High |
| Laparoscopic Colectomy | Small | Shorter | High |
| Robotic-Assisted Colectomy | Small | Shorter | Very High |
Each colectomy method has its own benefits. The right one depends on your needs and the surgeon’s advice. Knowing about these options helps you make better choices for your care.
Medical Conditions Requiring Colectomy
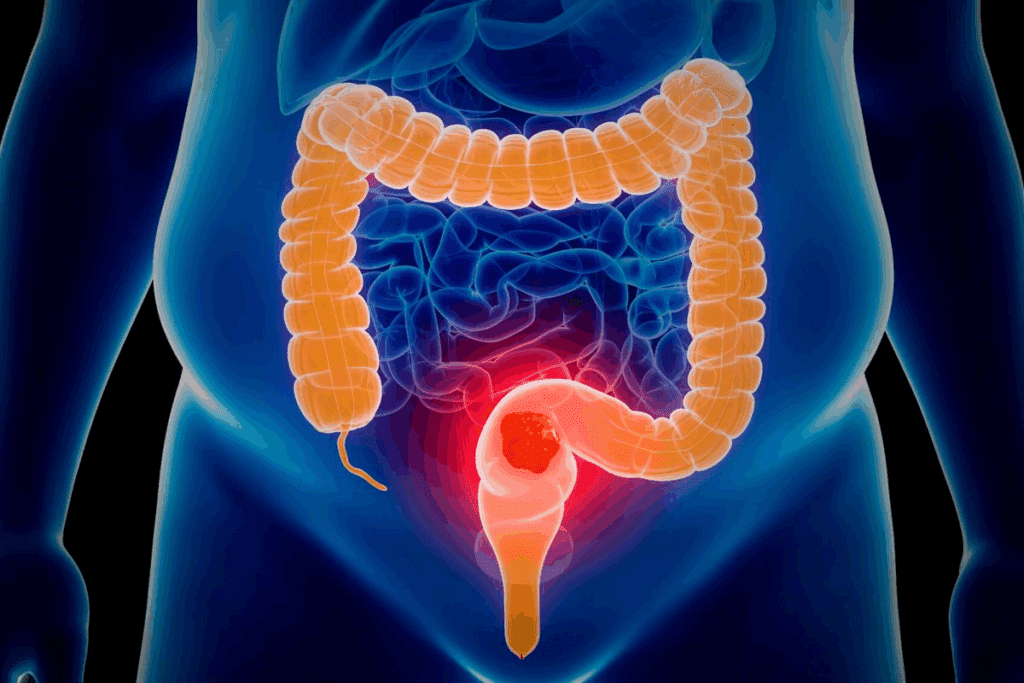
A colectomy is needed for many colon health issues. This includes colorectal cancer, inflammatory bowel disease, and diverticulitis. These conditions often require surgery.
Colorectal Cancer
Colorectal cancer is a main reason for colectomy. Removing the cancerous part of the colon is key. This surgery aims to remove the tumor and affected tissue.
Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) includes Crohn’s and ulcerative colitis. It can greatly affect life quality. When other treatments fail, a colectomy may be needed to remove the affected colon part.
Diverticulitis
Diverticulitis is inflammation of the colon wall’s diverticula. It can cause abscesses, perforations, or strictures. For severe or recurrent cases, a colectomy might be necessary.
Other Conditions
Other conditions needing a colectomy include severe colon injuries and volvulus. Also, some congenital colon conditions may require it. The choice to do a colectomy depends on the patient’s health and the condition’s severity.
Preparing for Colectomy Surgery
Getting ready for colectomy surgery involves many important steps. Each step is key to a good outcome. It’s vital to understand how each step helps you recover better.
Medical Evaluations and Tests
Before surgery, you’ll have many medical tests. These tests check your health and find any risks. They also help decide the best surgery for you.
Tests include blood work, CT scans, and heart checks. Your doctor will also look at your medical history and current medicines. This helps plan your surgery and care after.
Dietary Restrictions and Bowel Preparation
Your diet changes are important before surgery. You might eat less fiber or only liquids. Bowel prep cleans your bowel with meds or enemas.
It’s key to follow your doctor’s diet and prep advice. This gets you ready for surgery.
Mental Preparation and What to Bring to the Hospital
Mental prep is as important as physical prep. Knowing what to expect can reduce anxiety. Talk to your doctor to feel more ready.
Bring important items like comfy clothes and personal care things. Having someone with you offers emotional support and help.
Colectomy Recovery Timeline
Knowing the colectomy recovery timeline helps patients prepare for what comes next. Most people start feeling better in a few weeks. It’s important to understand this to manage expectations.
Immediate Post-Surgery Recovery
Right after surgery, patients stay in the hospital to watch for any issues. This time is key for managing pain and making sure the patient is on the right track. Effective pain management is a top priority, with doctors giving the right meds to keep pain low.
A leading surgical expert says, “The immediate post-operative period is key for a smooth recovery.”
“The key to a successful recovery lies in the meticulous care provided immediately after surgery.”
First Week After Surgery
The first week is all about slowly getting better. Patients should rest and avoid hard work. Gradual mobilization helps prevent blood clots. Doctors also suggest easy-to-digest foods.
| Day | Activity Level | Dietary Recommendations |
| 1-2 | Rest | Liquid diet |
| 3-4 | Gradual mobilization | Soft foods |
| 5-7 | Increased activity | Gradual introduction to normal diet |
Weeks 2-6 After Surgery
Over the next few weeks, patients keep getting better. Most get back to normal in 6-8 weeks. It’s vital to follow post-operative care instructions closely. Patients should slowly get back to their usual activities and diet.
Long-Term Recovery
Long-term recovery means staying healthy and going to follow-up visits. It’s important to monitor health and tell the doctor about any odd symptoms. Eating well and staying active are key for overall health.
By knowing the colectomy recovery timeline and following care advice, patients can get back to their normal life. Following post-operative instructions and having support are key to recovery.
Potential Complications and Risks of Colectomy
Colectomy, like any big surgery, comes with risks and complications. It’s usually safe, but knowing these risks helps patients make better choices. This is key for their care.
Short-Term Complications
Right after surgery, you might face infection, bleeding, or bad reactions to anesthesia. These can happen during or right after the surgery. Infections might need antibiotics, and bleeding could need more surgery.
Other quick problems might be breathing issues like pneumonia or heart problems. People with health issues before surgery are more at risk. So, checking health before surgery is very important.
Long-Term Complications
Long-term issues after colectomy can be serious. These include bowel obstruction, hernias, and problems with absorbing nutrients. Bowel obstruction might need more surgery because of adhesions or narrow intestines.
Hernias, like incisional hernias, can happen through the scar. If a lot of colon is removed, it can lead to trouble absorbing water and salts.
Risk Factors for Complications
Some things make you more likely to face problems after colectomy. Being older or having health issues like diabetes or heart disease increases risk.
Also, smoking and being overweight can raise your risk. Knowing these can help doctors prevent and watch over patients more closely.
Life After Colectomy: Adjusting to a New Normal
The time after colectomy surgery is key for patients. They must make lifestyle changes to manage their health well.
Dietary Changes and Recommendations
After surgery, changing your diet is vital. Patients should stick to a diet that’s easy to digest. They should slowly add new foods to their meals.
At first, a low-fiber diet may be needed to help the bowel heal. As they get better, they can add more fiber-rich foods. Drinking lots of water is also important.
Physical Activity Guidelines
Starting to be active again should be slow. Patients should begin with light activities like short walks. They can then increase the intensity and time as they get stronger.
It’s important to listen to your body and not overdo it. Always check with healthcare providers before starting any new exercise.
Emotional and Psychological Adjustments
Adjusting to life after colectomy also means dealing with emotions. Patients may feel many things, from relief to anxiety.
Getting support from healthcare, support groups, or loved ones is key. It helps manage emotional changes. Being patient with oneself and allowing time to adjust is also important.
By making these changes and following healthcare advice, patients can live fulfilling lives after surgery.
Colectomy Surgery Costs and Insurance Coverage
It’s important for patients to know about the costs of colectomy surgery. The price can change a lot based on several things. These include the type of surgery, how long you stay in the hospital, the surgeon’s fees, and aftercare.
Average Costs of Different Colectomy Procedures
The cost of colectomy surgery can vary a lot. This is because each surgery is different. Here’s a look at the average costs for different types of colectomy procedures:
| Type of Colectomy | Average Cost Range |
| Total Colectomy | $15,000 – $30,000 |
| Partial Colectomy | $10,000 – $25,000 |
| Hemicolectomy | $12,000 – $28,000 |
| Laparoscopic Colectomy | $18,000 – $35,000 |
Insurance Coverage for Colectomy
Insurance is a big help in covering the costs of colectomy surgery. Most plans do cover these surgeries. But, how much they cover can differ a lot.
Key factors to consider:
- Make sure your insurance covers the surgery your doctor recommends.
- Know what you’ll have to pay out of pocket, like deductibles and copays.
- Check if your insurance needs you to get approval before the surgery.
Financial Assistance Options
If you’re worried about money, there are ways to get help:
- Look into patient assistance programs at hospitals or non-profit groups.
- Use financial counseling services to help with insurance and costs.
- Some places offer fees based on how much you make.
Knowing about the costs of colectomy surgery and the help available can make things easier. It helps patients get ready for the financial side of their care.
Advancements in Colectomy Techniques
The field of colectomy surgery is changing fast. New techniques are making care better for patients. These changes are moving towards less invasive and more advanced methods.
Minimally Invasive Innovations
Minimally invasive colectomy has changed colorectal surgery a lot. Laparoscopic and robotic-assisted colectomy are now common. They offer shorter recovery times, less pain, and better looks.
Key advancements in minimally invasive colectomy include:
- Enhanced visualization through high-definition cameras
- Increased precision with robotic instrumentation
- Reduced trauma to the patient, resulting in less post-operative pain
- Shorter hospital stays and faster recovery times
Future Directions in Colectomy Surgery
Technology keeps getting better, and so will colectomy surgery. We’re seeing new trends like artificial intelligence, better imaging, and more personalized surgery. These changes promise even better care and treatment plans for patients.
| Future Direction | Description | Potential Benefit |
| Artificial Intelligence | Integration of AI for predictive analytics and surgical planning | Improved accuracy in diagnosis and treatment planning |
| Advanced Imaging | Enhanced imaging techniques for better visualization during surgery | More precise surgical interventions |
| Personalized Surgery | Tailored surgical approaches based on individual patient characteristics | Better patient outcomes through customized care |
We’re dedicated to leading in these advancements. We want to make sure our patients get the best and newest treatments.
When to Contact Your Doctor After Colectomy
Knowing when to see a doctor after colectomy surgery is key for a good recovery. After surgery, it’s important to watch your health closely. Look out for signs that might mean you need more medical help.
Warning Signs of Complications
Some symptoms after colectomy surgery need quick doctor visits. These include:
- Severe abdominal pain that doesn’t get better with medicine
- Fever over 101.5°F (38.6°C)
- Signs of infection at the cut site, like redness, swelling, or discharge
- Bleeding or discharge from the rectum
- Nausea or vomiting that keeps going
- Constipation or trouble passing gas
If you notice any of these signs, call your doctor right away.
Routine Follow-up Schedule
Seeing your doctor regularly is important to check on your recovery. This schedule usually includes:
- A check-up within 1-2 weeks after surgery to see how the cut is healing and how you’re doing
- More visits if needed, based on how you’re feeling and what your doctor says
- Talks about changing your diet, starting to move more, and other post-surgery care
Sticking to this schedule helps catch and fix any problems early. This supports a smooth recovery.
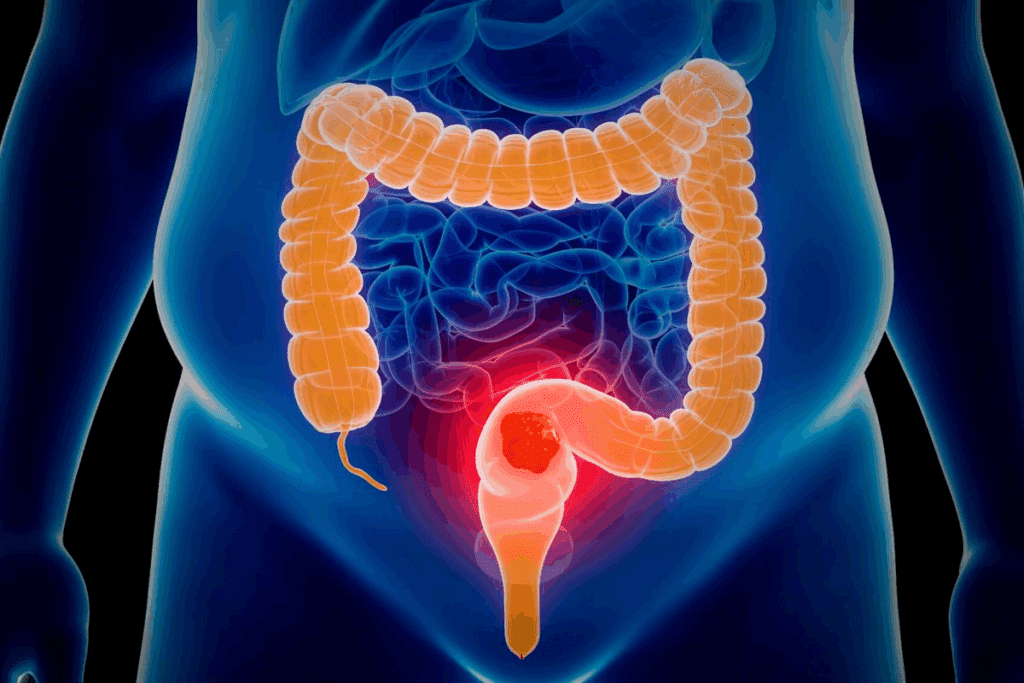
Alternative Treatments to Consider Before Colectomy
Looking into alternative treatments before colectomy can give patients more choices. Colectomy might be needed sometimes, but other treatments can work too. They might even stop surgery from being necessary.
Medical Management Options
For some conditions, medical management is a good alternative. This includes:
- Medications to manage symptoms and disease progression
- Lifestyle changes, such as dietary adjustments and increased physical activity
- Alternative therapies, including acupuncture and stress management techniques
These options are often helpful for inflammatory bowel disease (IBD). A mix of medicine and lifestyle changes can control symptoms. This might avoid the need for surgery.
| Condition | Medical Management Options | Potential Benefits |
| Inflammatory Bowel Disease (IBD) | Medications, dietary changes, stress management | Reduced symptoms, improved quality of life |
| Diverticulitis | Antibiotics, dietary adjustments, bowel rest | Avoidance of surgery, reduced complications |
| Colorectal Cancer | Chemotherapy, radiation therapy, targeted therapy | Reduced tumor size, improved survival rates |
When Surgery Becomes Necessary
Even with alternative treatments, sometimes surgery is needed. This can happen if the condition is severe, medical management fails, or complications arise. Surgery is often the best way to treat the condition and improve life quality.
Indications for Surgery include severe disease not helped by medicine, significant complications, and colorectal cancer needing tumor removal.
Choosing to have colectomy is a big decision. It should be made after trying all other options. By looking into alternative treatments and knowing when surgery is needed, patients can make better choices for their care.
Conclusion: Making Informed Decisions About Colectomy
Understanding colectomy is key to making good choices. Our colorectal surgery clinic offers support and guidance. We help patients understand their options and aim for the best results.
Knowing about colectomy surgery is important. This includes the types of procedures and what to expect during recovery. We tailor care to each patient’s needs, whether it’s a total or partial colectomy.
Our team is committed to top-notch healthcare for international patients. We aim to clearly explain colectomy surgery. This helps patients make informed decisions and recover well.
FAQ
What is a colectomy, and why is it performed?
A colectomy is a surgery to remove part of the colon. It treats conditions like colon cancer and Crohn’s disease. It’s also used for diverticulitis and ulcerative colitis.
What are the different types of colectomy procedures?
There are several colectomy procedures. These include total colectomy, partial colectomy, and hemicolectomy. The choice depends on the disease’s location and extent.
What is the difference between open and laparoscopic colectomy?
Open colectomy uses a big incision. Laparoscopic colectomy uses small incisions and special tools. It causes less damage and leads to quicker healing.
How long does it take to recover from a colectomy?
Recovery from a colectomy takes about 6-8 weeks. The first week is key for managing pain. Gradually, you can start doing normal activities again.
What are the possible complications and risks of colectomy surgery?
Colectomy surgery can have risks like infection and bleeding. Other risks include reactions to anesthesia and bowel obstruction. Hernias and malabsorption issues are also possible.
How can I prepare for colectomy surgery?
To prepare for surgery, you’ll have medical tests and follow dietary rules. Bowel preparation is also necessary. Mental preparation helps reduce anxiety and aids in recovery.
What dietary changes are recommended after a colectomy?
After surgery, follow specific diets to manage bowel movements. A healthy diet and lifestyle are key for recovery.
Can I return to my normal activities after a colectomy?
Yes, you can return to normal activities after a colectomy. But, always follow your surgeon’s advice on physical activity and lifestyle changes.
How much does colectomy surgery cost, and what are the insurance coverage options?
The cost of colectomy surgery varies. Insurance coverage is important in managing costs. Explore your insurance options and financial help programs.
Are there alternative treatments to colectomy surgery?
For some conditions, treatments like medications and lifestyle changes are options. But, for severe or unresponsive cases, surgery is often needed.
References
Nature. Evidence-Based Medical Insight. Retrieved from https://www.nature.com/articles/s41572-020-0171-y










