Last Updated on November 26, 2025 by Bilal Hasdemir
Having colon surgery can be scary. Knowing about complications is key for patients and their families. About 28 percent of patients face colon resection complications.Discover 12 alarming colon resection complications. Learn the most common and serious problems that can occur after surgery.
Studies have found common issues after surgery. These include surgical site infections and postoperative ileus. At Liv Hospital, we focus on safety and quality in every colon operation.
Key Takeaways
- Colon resection complications affect a significant percentage of patients.
- Common complications include surgical site infections and postoperative ileus.
- Liv Hospital prioritizes patient safety and quality care.
- Understanding potential complications is crucial for effective recovery.
- Advanced protocols are in place to minimize risks.
What Happens During Colon Resection Surgery
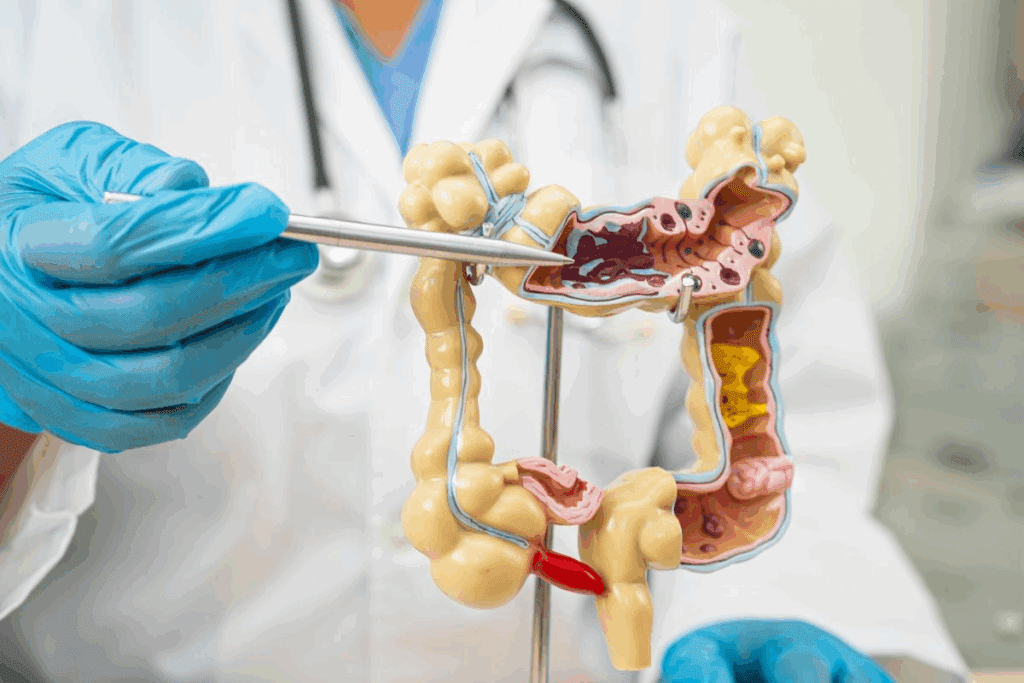
Colon resection surgery removes a part of the colon that’s sick or damaged. The exact surgery depends on the patient’s health, the disease’s extent, and the surgeon’s advice.
Knowing about surgery can make you feel better. This surgery is done for many reasons like colon cancer, diverticulitis, and inflammatory bowel disease.
Types of Colon Resection Procedures
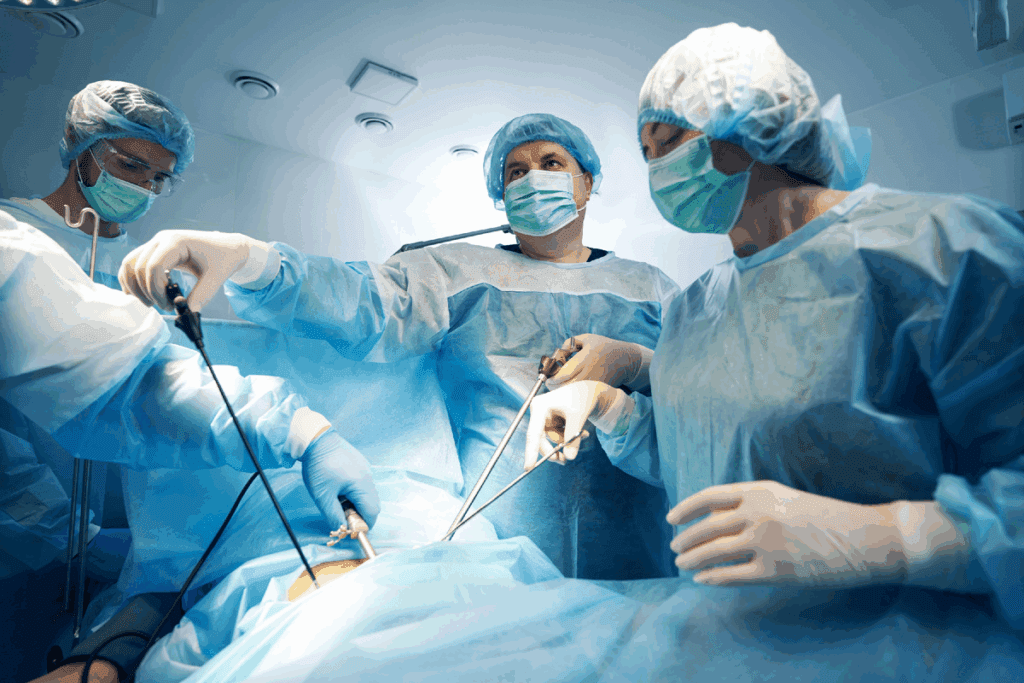
There are two main types of colon resection surgeries: open colectomy and minimally invasive colectomy.
- Open Colectomy: This traditional method uses a big incision in the belly to reach the colon.
- Minimally Invasive Colectomy: This uses smaller cuts, like with laparoscopic or robotic surgery, for quicker healing.
| Procedure Type | Description | Recovery Time |
| Open Colectomy | Single, larger incision | Typically longer |
| Laparoscopic Colectomy | Smaller, multiple incisions | Generally shorter |
| Robotic-Assisted Colectomy | Smaller incisions with robotic aid | Often shorter |
Common Reasons for Colon Surgery
Colon surgery is done for many health issues. Here are some common ones:
- Colon Cancer: It removes the cancer part of the colon.
- Diverticulitis: It treats inflammation in the colon’s pouches.
- Inflammatory Bowel Disease (IBD): It’s for conditions like Crohn’s disease and ulcerative colitis.
“Choosing colon resection surgery is a big step. It’s after trying other treatments. It can really improve a patient’s life.”
Knowing why and how colon resection surgery is done can make patients feel more ready and calm about it.
Understanding Colon Resection Complications
Colon resection surgery is usually safe but can have complications. About 28 percent of patients face issues after surgery. It’s important to know about these problems.
Statistics on Complication Rates
Complication rates after colon surgery vary. They depend on the patient’s health, the surgery method, and any existing conditions. Some patients are more likely to face complications, showing the need for tailored care.
Complication rates can be quite different. But, it’s key to remember that complications can greatly affect recovery and quality of life. Knowing these rates helps manage patient expectations and improve results.
- Overall complication rates range from 20% to 40% in various studies.
- Certain complications, such as surgical site infections, are more common in patients with specific risk factors.
- The severity of complications can vary, with some requiring additional surgical intervention.
Risk Factors for Developing Complications
Several factors can increase the risk of complications after colon resection surgery. These include:
- Age: Older patients are generally at higher risk.
- Comorbidities: Presence of other health conditions, such as diabetes or heart disease.
- Surgical technique: The method used for the surgery can influence complication rates.
- Patient’s overall health status: Nutritional status and other health factors play a role.
Identifying these risk factors early allows us to implement targeted strategies to minimize their impact.
Preventive Measures
To reduce the risk of complications, several preventive measures can be taken. These include:
- Preoperative optimization of the patient’s health status.
- Use of appropriate surgical techniques and technologies.
- Implementation of enhanced recovery after surgery (ERAS) protocols.
- Close monitoring for potential complications during the postoperative period.
By understanding the risk factors and implementing these preventive measures, we can significantly reduce the incidence of complications and improve patient outcomes after colon resection surgery.
Surgical Site Infections After Colon Surgery
Surgical site infections are a big worry for those having colon surgery. These infections can cause longer hospital stays, more surgeries, and higher costs. We’ll talk about symptoms to watch for, treatment options, and how to prevent them.
Recognizing Infection Symptoms
Surgical site infections show up in different ways. It’s important for patients to know:
- Increased pain or tenderness around the surgical site
- Redness or swelling
- Pus or discharge
- Fever or chills
- A general feeling of being unwell
Treatment Approaches
Treatment for these infections usually involves antibiotics. Sometimes, more surgery is needed to clear the infection. We’ll explain the common treatments and what to expect during recovery.
The treatment often includes:
- Antibiotics tailored to the infection type
- Draining the infected site, either surgically or through a tube
- Supportive care, like pain management and wound care
Prevention Strategies
Preventing these infections is a team effort. It involves steps before, during, and after surgery. We’ll cover the ways healthcare providers work to lower infection risks.
Prevention strategies include:
- Preoperative antibiotics
- Proper skin preparation
- Keeping the surgery area clean and sterile
- Postoperative wound care and monitoring
Anastomotic Leakage: A Serious Complication
Colon resection surgery is often lifesaving but comes with risks. One major risk is anastomotic leakage. This is when intestinal contents leak through a surgical join. It can cause severe infections, sepsis, and even death.
Why Leaks Occur
Leaks can happen due to several reasons. Technical problems during surgery and patient health issues are common causes. Issues like inadequate blood supply or tension on the anastomotic site can occur. Also, diabetes, malnutrition, or certain medications can affect healing.
Knowing these risks helps surgeons and healthcare providers prevent and manage complications after surgery.
Diagnosis and Detection
Diagnosing anastomotic leakage involves clinical checks and imaging. Patients might show fever, abdominal pain, or signs of sepsis. CT scans with contrast can confirm the leak by showing contrast material leakage.
Spotting the problem early is key to effective management and reducing severe complications.
Management Options
Managing anastomotic leakage depends on several factors. These include the leak’s severity, the patient’s health, and any complications. Treatment can range from conservative management with antibiotics and drainage to surgical intervention to fix or remove the anastomosis.
In some cases, placing a stent or a drain may be needed to manage the leak and aid in healing.
Postoperative Ileus and Bowel Function Disruption
After colon surgery, a common issue is postoperative ileus. It stops the bowel muscles from moving normally. This leads to a buildup of food, fluids, and gas in the intestines.
Postoperative ileus is a big worry for those recovering from colon surgery. It’s important to know what causes it, how long it lasts, and how to treat it.
Causes of Ileus After Colon Surgery
Many things can cause postoperative ileus, like surgery trauma, anesthesia, and opioid pain meds. Surgery can cause inflammation and stop bowel movements.
Key factors contributing to postoperative ileus include:
- Surgical stress and trauma
- Anesthesia and pain management medications
- Electrolyte imbalances
- Pre-existing medical conditions
Duration and Recovery Timeline
How long postoperative ileus lasts varies. It usually goes away in a few days to a week. But, recovery time can depend on the surgery and the patient’s health.
| Day Post-Surgery | Expected Recovery Progress |
| 1-3 Days | Initial recovery; bowel sounds may be absent or reduced |
| 3-5 Days | Bowel movements may start to return; patients may pass gas |
| 5-7 Days | Bowel function typically improves; patients may start having bowel movements |
Treatment Approaches
Managing postoperative ileus involves several strategies. We suggest a mix of methods to help restore bowel function and ease symptoms.
Conservative management: This includes rest, hydration, and medications to help bowel movements.
Advanced treatments: Sometimes, more steps are needed. This might include prokinetic agents or a nasogastric tube to relieve stomach pressure.
Bleeding Complications Following Colon Resection
After colon resection surgery, bleeding can be a serious issue. It worries both patients and doctors. We will look at when bleeding happens, how to spot it, and how to handle it.
Early vs. Late Bleeding
Bleeding after colon surgery is divided into early and late types. Early bleeding happens right after surgery, often because of bad hemostasis or surgical mistakes. Late bleeding occurs days or weeks later, possibly due to infection or other issues. Knowing when and why bleeding happens is key to managing it well.

Identifying Internal Bleeding
Finding internal bleeding can be tough, as symptoms may not show up right away. Signs include belly pain, swelling, and signs of not enough blood like fast heart rate and low blood pressure. Sometimes, people might see melena (black, tarry stools) or hematemesis (vomiting blood), which means bleeding in the gut. Spotting these signs quickly is crucial for quick action.
Management Strategies
Handling bleeding after colon surgery needs a few steps. First, stabilize the patient with fluids and maybe blood transfusions. For bleeding that won’t stop, endoscopic procedures can find and fix the problem. If it’s really bad, surgical intervention might be needed. It’s important to watch the patient closely and tailor the treatment for each case.
Intra-abdominal Abscesses: Formation and Treatment
Intra-abdominal abscesses are a serious issue that can happen after colon surgery. They need quick diagnosis and treatment. These are pockets of pus in the belly, often from bacteria during surgery.
Risk Factors for Abscess Development
Some things make getting intra-abdominal abscesses more likely after colon surgery. These include:
- Pre-existing conditions like diabetes or weakened immune systems, which can slow healing and raise infection chances.
- Surgical complexity: More complex or longer surgeries might raise the risk of abscesses.
- Anastomotic leakage: Leaks at the surgical connection can cause abscesses.
Diagnostic Approaches
Diagnosing intra-abdominal abscesses involves a mix of clinical checks and imaging. We use:
- CT scans: To see the abscess and where it is in the belly.
- Ultrasound: Sometimes for the first check or to help with drainage.
- Clinical symptoms: Like fever, belly pain, and high white blood cell count, which suggest an abscess.
Drainage and Antibiotic Therapy
Treating intra-abdominal abscesses usually means draining the abscess and using antibiotics. We:
- Start with broad-spectrum antibiotics, which might change based on culture results.
- Do drainage to get rid of the infected stuff, helping healing and lowering complication risk.
- Keep a close eye for signs of getting better or new problems, adjusting treatment as needed.
Urinary Complications After Bowel Surgery
Urinary problems are a big worry for people having bowel surgery. They can make recovery harder and affect life quality. Issues like infections, trouble with urine flow, and lasting problems can happen.
Urinary Tract Infections
Urinary tract infections (UTIs) are common after bowel surgery. UTIs happen when bacteria get into the urinary system, leading to infection and pain. Symptoms include painful urination, needing to pee a lot, and belly pain.
We suggest keeping an eye out for UTI signs after surgery. Spotting and treating UTIs early is key to stop them from getting worse.
Urinary Retention
Urinary retention is another issue after bowel surgery. It means you can’t fully empty your bladder. It might be due to surgery damage, anesthesia effects, or pain.
Dealing with urinary retention includes using catheters, medicines to help the bladder, and exercises to strengthen pelvic muscles.

Long-term Urinary Dysfunction
Some people face long-term urinary problems after surgery. This can be ongoing incontinence, smaller bladder, or constant UTIs. The chance of lasting issues depends on surgery type, bladder health before surgery, and aftercare.
We stress the need for follow-up care for urinary problems. It’s important for patients to tell their doctors about any ongoing symptoms. This way, they can get the right help.
Respiratory Complications: Pneumonia and Pulmonary Issues
Patients having colon surgery often face respiratory problems like pneumonia. These issues can stem from the surgery itself or the patient’s health.
Knowing the risks of respiratory problems is important. We need to identify what increases these risks, prevent them, and know how to treat them.
Risk Factors for Developing Pneumonia
Several factors can make pneumonia more likely after colon surgery. These include:
- Advanced age
- Pre-existing lung disease
- Smoking history
- Obesity
- Type of anesthesia used
Knowing these risk factors helps us provide better care to reduce these risks.
Prevention Strategies
Preventing pneumonia and other lung problems is crucial. We use several strategies, including:
- Preoperative smoking cessation
- Optimizing lung function before surgery
- Using appropriate anesthesia techniques
- Early mobilization after surgery
- Respiratory therapy
These strategies help lower the risk of respiratory complications.
Treatment Approaches
If pneumonia or lung problems occur, quick treatment is key. Treatment may include:
- Antibiotic therapy for infections
- Respiratory support, such as oxygen therapy or mechanical ventilation
- Pain management to facilitate easier breathing
- Physical therapy to improve lung function
The treatment choice depends on the complication’s severity and type.
Here’s a summary of the key points regarding respiratory complications after colon surgery:
| Complication | Risk Factors | Prevention Strategies | Treatment Approaches |
| Pneumonia | Advanced age, pre-existing lung disease, smoking | Smoking cessation, optimizing lung function | Antibiotic therapy, respiratory support |
| Pulmonary Issues | Obesity, type of anesthesia | Early mobilization, respiratory therapy | Pain management, physical therapy |
By understanding the risks and taking proactive steps, we can minimize respiratory complications after colon surgery.
Long-Term Complications from Colon Resection
Colon resection surgery can save lives but comes with long-term risks. It’s important for patients and doctors to know these risks. This way, we can work together to get the best results.
Adhesions and Bowel Obstruction
Adhesions are a big risk after colon surgery. They are like scar tissue that can twist or block the intestine. This can cause severe pain, vomiting, and constipation.
In some cases, surgery is needed to fix the blockage. This can help repair damaged parts of the intestine.
Altered Bowel Habits
Colon surgery can change how you go to the bathroom. You might have diarrhea or constipation. These changes can really affect your life and might need special diets or medicines.
Metabolic and Nutritional Disturbances
Removing part of the colon can mess with how your body absorbs nutrients. The colon helps with water and nutrient absorption. This can lead to nutrient deficiencies over time.
- Vitamin and mineral deficiencies
- Electrolyte imbalances
- Changes in bowel function affecting nutrient absorption
Port-Site Metastases
For cancer patients, there’s a rare but serious risk called port-site metastases. This happens when cancer cells grow at the surgical port sites. It’s a serious issue that needs quick action.
Knowing about these risks helps us all. It lets us work together to make life better for those who have colon surgery.
Conclusion: Managing Recovery and Improving Outcomes
Managing recovery after colon surgery is key to better patient outcomes. Knowing about possible complications like infections and ileus helps patients take action. This can reduce risks.
Studies show that complete care and follow-up are vital after colon surgery. We work with patients to prevent problems and catch them early. This way, we can help them recover well and improve their results.
Helping patients understand and support them is crucial. By focusing on recovery and better outcomes, we aim for the best results. This way, patients can get back to their lives quickly.
FAQ
What are the most common complications after colon resection surgery?
Common issues include infections at the surgical site, leaks from the joined parts of the colon, and problems with bowel movement. Other complications are bleeding, abscesses in the abdomen, urinary issues, and breathing problems.
How can I identify signs of infection after colon surgery?
Look out for fever, redness, swelling, or discharge from the surgical area, and abdominal pain. If you notice these signs, get medical help right away.
What is anastomotic leakage, and how is it managed?
Anastomotic leakage is when the joined parts of the colon start leaking. Treatment might include antibiotics, draining, or even more surgery, based on how bad it is.
What is postoperative ileus, and how long does it last?
Postoperative ileus is when bowel movements stop temporarily. It can last a few days. Treatment includes rest, staying hydrated, and sometimes medicine to help the bowel move again.
How can bleeding complications be identified and managed after colon resection?
Bleeding issues show as bloody stools, pain in the abdomen, or feeling dizzy. Getting medical help quickly is key. Treatment might include blood transfusions, endoscopy, or surgery.
What are the risk factors for developing intra-abdominal abscesses after colon surgery?
Risks include leaks from the joined parts of the colon, contamination during surgery, and conditions like diabetes or weakened immune systems.
How can urinary complications be managed after bowel surgery?
Urinary problems, like infections or not being able to urinate, can be treated with antibiotics, catheters, or other interventions as needed.
What are the long-term complications of colon resection surgery?
Long-term issues might include adhesions, changes in bowel habits, metabolic and nutritional problems, and rare cases of cancer spreading to the surgical site. Regular check-ups and management can help manage these problems.
How can I minimize the risk of complications from colon resection surgery?
To reduce risks, follow all instructions before and after surgery, stay healthy, and keep up with follow-up appointments.
What are the signs of internal bleeding after colon surgery?
Signs of internal bleeding include severe pain in the abdomen, feeling dizzy, fainting, or seeing blood in the stool. If you notice these, seek medical help immediately.
Can colon resection surgery lead to long-term bowel problems?
Yes, surgery can cause changes in bowel habits, like diarrhea, constipation, or blockages. There are ways to manage these symptoms.
How are respiratory complications, such as pneumonia, prevented and treated after colon surgery?
Preventing respiratory issues involves early movement, breathing therapy, and quitting smoking. Treatment for pneumonia might include antibiotics, oxygen, or other treatments as needed.
References
Ljubičić, N., et al. (2015). Biliary leakage after urgent cholecystectomy. Journal of Hepato-Biliary-Pancreatic Sciences. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4436923





