
At Liv Hospital, we know how complex heart rhythm disorders can be. Cardiac arrhythmia is when the heart’s rhythm gets disrupted. This can affect how fast or steady the heart beats.
Arrhythmia happens when the heart’s electrical system goes wrong. This can mess up how well the heart pumps blood. It’s important to understand these issues to treat them right.
We focus on giving our patients the best care for heart rhythm problems. Our team works hard to make sure each patient gets the right treatment. We offer support and advanced medical care that fits each person’s needs.
Key Takeaways
- Cardiac arrhythmia refers to disturbances in the heart’s rhythm.
- Arrhythmias can lead to complications if not properly managed.
- Understanding heart rhythm disturbances is key for good treatment.
- Liv Hospital offers top-notch care for heart rhythm issues.
- We provide detailed support and cutting-edge medical treatments for our patients.
The Fundamentals of Heart Rhythm Disorders

Heart rhythm disorders, or arrhythmias, happen when the heart’s electrical system goes wrong. This system is complex and controls the heartbeat. It makes sure the heart pumps blood well all over the body. Explore define dysrhythmia cardiac meaning and learn about the top 10 common arrhythmia types.
Normal Cardiac Conduction System
The heart’s electrical system is a detailed network that sends out electrical signals. These signals are key for the heartbeat to work right. It starts with the sinoatrial (SA) node, the heart’s natural pacemaker.
It sends out electrical impulses that travel through the atrioventricular (AV) node and down to the ventricles. This makes them contract.
The key components of the cardiac conduction system include:
- The sinoatrial (SA) node
- The atrioventricular (AV) node
- The bundle of His
- The bundle branches
- The Purkinje fibers
What Happens During Rhythm Disturbances
Rhythm disturbances, or arrhythmias, happen when the heart’s electrical system doesn’t work right. This can be due to many reasons. It could be because of problems with the SA node, blockages in the pathway, or strange electrical activity in the heart.
Common causes of rhythm disturbances include:
- Abnormalities in the heart’s electrical system
- Heart disease or damage
- Electrolyte imbalances
- Certain medications
Prevalence and Impact on Public Health
Arrhythmias are a big public health issue, affecting millions globally. The Centers for Disease Control and Prevention (CDC) says atrial fibrillation, a common arrhythmia, affects 2.7 to 6.1 million in the U.S.
“Arrhythmias can be a serious condition, and in some cases, they can lead to severe complications, including stroke and heart failure.”
The effects of arrhythmias on public health are huge, with big economic and healthcare costs. Knowing about heart rhythm disorders is key to finding good ways to prevent and treat them.
How to Define Dysrhythmia Cardiac: Medical Terminology Explained
Understanding “dysrhythmia cardiac” is key for both patients and doctors. It means any problem with the heart’s rhythm. This issue often comes from a problem with the heart’s electrical system.
Let’s look at the medical terms closely. Dysrhythmia and arrhythmia are often mixed up. But they have slight differences in meaning.
Dysrhythmia vs. Arrhythmia: Medical Definitions
Dysrhythmia is about an abnormal rhythm in the heart. It points to a problem with the heart’s rhythm. Arrhythmia, on the other hand, means there’s no rhythm at all. It shows the heart’s beat is irregular or missing.
Even though both terms describe heart rhythm issues, they have different shades of meaning. Dysrhythmia is sometimes used in medical talk because it clearly shows an abnormal rhythm.
Common Terminology Variations Worldwide
Medical terms change a lot from place to place and language to language. For example, “aritmia” is used in some places for what English calls arrhythmia.
| Term | Region/Language | English Equivalent |
| Aritmia | Spanish, Italian | Arrhythmia |
| Arrythmie | French | Arrhythmia |
| Arrhythmie | German | Arrhythmia |
Cardiac Arrhythmia Abbreviations in Medical Records
In medical records, many abbreviations are used for arrhythmias. Knowing these abbreviations is key for correct diagnosis and treatment.
Some common ones are:
- AFib: Atrial Fibrillation
- AF: Atrial Flutter
- VT: Ventricular Tachycardia
- VF: Ventricular Fibrillation
These abbreviations help doctors quickly spot and handle cardiac arrhythmias.
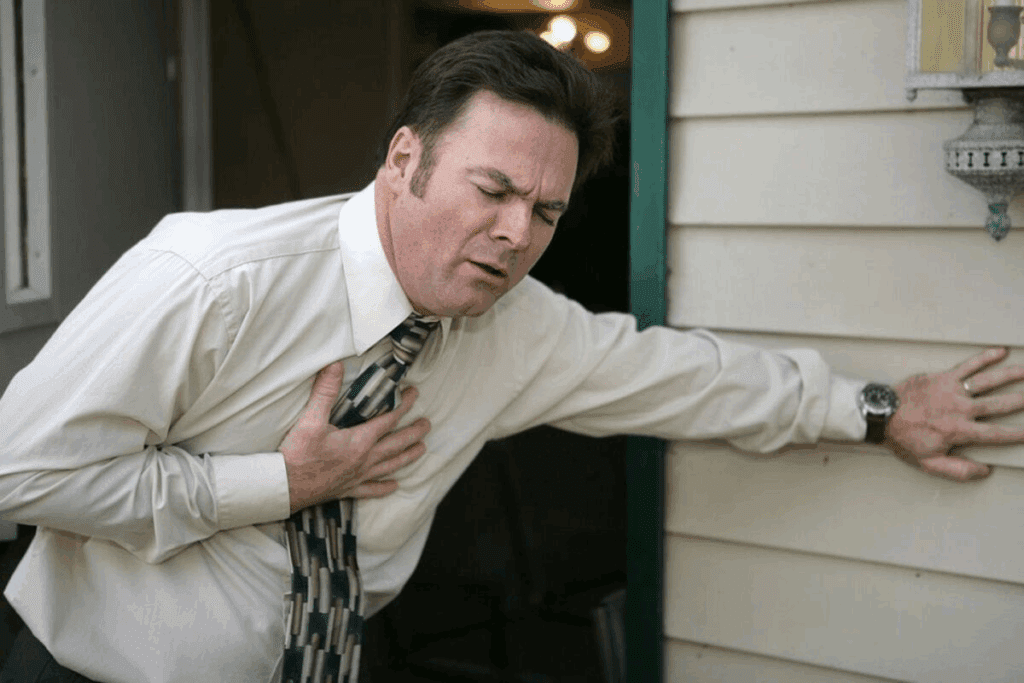
Recognizing Arrhythmia Symptoms and Warning Signs
Knowing the signs of arrhythmia can help a lot. Arrhythmias, or irregular heartbeats, can show up in different ways. It’s important for people to know the symptoms that might mean they have a problem.
Heart Palpitations and Irregular Heartbeat Sensations
Heart palpitations often go with arrhythmias. They might feel like fluttering or skipped beats. These feelings happen when the heart’s rhythm is off, making it beat too fast, too slow, or not right.
People might say their heart feels like it’s pounding or racing. This can be scary and might mean there’s something wrong that needs a doctor’s help.
Characteristic Irregular Heartbeat Sounds
Irregular heartbeat sounds can be a big clue about arrhythmia. These sounds might sound like skipping beats or an odd rhythm. Some people might feel a fluttering in their chest, which could mean they have an arrhythmia.
If you notice these sounds or feelings, it’s important to talk to a doctor. They can help figure out what’s going on.
When Symptoms Require Medical Attention
Arrhythmia symptoms can include shortness of breath, feeling weak, dizzy, or lightheaded. You might faint or feel like you’re going to faint. A racing heart or palpitations, and chest pain or discomfort are also signs.
If you have any of these symptoms, you should see a doctor right away. The table below shows when you should get help fast.
| Symptom | Severity | Action |
| Chest Pain or Discomfort | Severe | Seek Immediate Medical Attention |
| Fainting or Feeling Faint | Severe | Seek Immediate Medical Attention |
| Shortness of Breath | Moderate to Severe | Consult a Healthcare Professional |
| Dizziness or Light-headedness | Moderate | Consult a Healthcare Professional |
Knowing these symptoms and when to see a doctor can really help. If you notice anything strange with your heart, don’t wait to talk to a healthcare provider.
Atrial Fibrillation (AFib): The Most Common Cardiac Arrhythmia
AFib, or atrial fibrillation, is a common heart rhythm disorder affecting millions. It causes an irregular and often fast heart rate. This can raise the risk of stroke, heart failure, and other heart problems.
Pathophysiology and Mechanisms
Atrial fibrillation happens when the heart’s upper chambers beat chaotically. This irregular heartbeat can lead to blood clots. These clots can then cause a stroke by being pumped to the brain.
The causes of AFib are complex. They include electrical and structural changes in the heart. These changes can be due to high blood pressure, heart valve diseases, and cardiac surgery.
Key factors contributing to AFib include:
- Hypertension
- Heart valve diseases
- Cardiac surgery
- Heart failure
- Thyroid disorders
Risk Factors and Causes
Several factors increase the risk of atrial fibrillation. Age is a big factor, with risk rising after 65. Other risks include obesity, diabetes, and sleep apnea.
Knowing these risks is key to prevention and early detection. Changing lifestyle factors and managing conditions can lower AFib risk.
Symptoms and Diagnosis
Symptoms of atrial fibrillation vary. Some people feel palpitations, shortness of breath, or chest pain. Others may not notice anything.
To diagnose AFib, doctors use an electrocardiogram (ECG). They may also use Holter monitoring, echocardiography, and blood tests.
Treatment Approaches
Treatment for AFib aims to control heart rate and rhythm. It also aims to prevent stroke. This can involve medications and procedures like cardioversion or catheter ablation.
Changing lifestyle is also important. This includes a healthy diet, regular exercise, and managing stress. In some cases, surgery may be needed.
Treatment strategies include:
- Medications to control heart rate or rhythm
- Anticoagulant therapy to prevent stroke
- Cardioversion to restore a normal heart rhythm
- Catheter ablation to destroy abnormal electrical pathways
- Lifestyle modifications for overall heart health
Atrial Flutter: Characteristics and Management
Atrial flutter has a regular heart rhythm, unlike atrial fibrillation. It’s a cardiac arrhythmia with a fast, regular heartbeat. This happens when the heart’s electrical circuit is abnormal, usually in the right atrium.
Understanding the Flutter Circuit
The flutter circuit is in the right atrium and has a macro-reentrant circuit. It can be typical (counterclockwise) or atypical (clockwise or other). Knowing how the circuit works is key to managing it.
Key characteristics of atrial flutter include:
- Regular atrial rhythm
- Rapid ventricular rate
- Characteristic “sawtooth” pattern on ECG
Symptoms and Clinical Presentation
Symptoms of atrial flutter vary but often include palpitations, shortness of breath, and fatigue. Some people may not show symptoms at all. Others might have more severe symptoms like chest pain or syncope.
“Atrial flutter is often associated with underlying heart disease, and its presence can significantly impact a patient’s quality of life.” –
A renowned cardiologist
Diagnostic Methods
Doctors use electrocardiography (ECG) to diagnose atrial flutter. The “sawtooth” or “flutter” waves are key signs. Holter monitoring or event monitoring might also be used to catch episodes.
Treatment Strategies
Treatment for atrial flutter includes rate control, rhythm control, and preventing blood clots. Rate control uses beta-blockers or calcium channel blockers. Rhythm control might involve cardioversion or anti-arrhythmic drugs.
| Treatment Approach | Description | Advantages |
| Rate Control | Using medications to control ventricular rate | Easy to implement, reduces symptoms |
| Rhythm Control | Restoring normal sinus rhythm through cardioversion or medications | Can improve quality of life, reduces risk of complications |
| Thromboembolic Prevention | Using anticoagulants to prevent stroke | Reduces risk of stroke, a major complication |
Managing atrial flutter needs a full approach. This includes the patient’s condition, symptoms, and risk factors. Understanding atrial flutter’s characteristics and management helps healthcare providers give better care.
Ventricular Tachycardia: A Potentially Life-Threatening Arrhythmia
Understanding ventricular tachycardia is key. It’s a heart rhythm problem that can affect your life and survival. It happens when the heart’s ventricles beat too fast due to abnormal electrical activity.
Types and Classifications
Ventricular tachycardia is divided into types based on how long it lasts and symptoms. It’s mainly split into:
- Nonsustained ventricular tachycardia: Lasts less than 30 seconds.
- Sustained ventricular tachycardia: Goes on for more than 30 seconds or needs quick medical help.
It’s also split into monomorphic and polymorphic types based on its shape.
Causes and Risk Factors
Several things can cause ventricular tachycardia, including:
| Cause | Description |
| Coronary artery disease | Less blood flow to the heart muscle. |
| Cardiomyopathy | Disease of the heart muscle. |
| Electrolyte imbalance | Abnormal levels of potassium, magnesium, or calcium. |
Symptoms and Diagnosis
Symptoms of ventricular tachycardia vary from mild to severe. They can include palpitations, dizziness, and shortness of breath. Doctors usually use an electrocardiogram (ECG) to diagnose it.
“Prompt diagnosis and treatment of ventricular tachycardia are critical to prevent complications and improve patient outcomes.”
Treatment and Management
Treatment for ventricular tachycardia depends on the cause, symptoms, and how well the heart is working. Options include:
- Cardioversion or defibrillation to fix the heart rhythm.
- Antiarrhythmic drugs to stop it from happening again.
- Catheter ablation to destroy the bad electrical pathway.
- Implantable cardioverter-defibrillator (ICD) for ongoing care.
It’s vital to get medical help quickly for ventricular tachycardia to avoid serious problems.
Ventricular Fibrillation: The Most Critical Arrhythmia
Ventricular fibrillation is a serious heart rhythm problem that needs quick medical help to avoid death. It happens when the heart’s ventricles beat too fast and erratically. This makes the heart unable to pump blood well.
Pathophysiology and Mechanism
The heart’s ventricles have abnormal electrical activity in ventricular fibrillation. This makes the ventricles shake instead of pumping blood. Factors like ischemia, electrolyte imbalances, and structural heart diseases often cause this.
Risk Factors and Triggers
Many things can lead to ventricular fibrillation. These include:
- Coronary artery disease
- Previous myocardial infarction
- Cardiomyopathy
- Electrolyte imbalances (e.g., hypokalemia, hyperkalemia)
- Certain medications
Clinical Presentation
Ventricular fibrillation shows up suddenly with loss of consciousness and no pulse. It’s a serious emergency that needs fast action.
Emergency Management
Handling ventricular fibrillation means starting cardiopulmonary resuscitation (CPR) and defibrillation right away. Using automated external defibrillators (AEDs) can help save lives. Also, following advanced cardiac life support (ACLS) rules is key.
| Management Step | Description |
| CPR | Immediate cardiopulmonary resuscitation to maintain circulation |
| Defibrillation | Use of AED or manual defibrillator to restore normal heart rhythm |
| ACLS | Advanced cardiac life support protocols for further management |
Bradyarrhythmias: When the Heart Beats Too Slowly
The heart’s rhythm is key for blood flow. Bradyarrhythmias happen when this rhythm is too slow. This can cause symptoms like fatigue, dizziness, and shortness of breath. Knowing the causes and types of bradyarrhythmias is vital for treatment.
Sinus Bradycardia
Sinus bradycardia is when the heart beats slower than usual. It’s common in athletes but can also be caused by medications or heart disease. Symptoms include dizziness, fainting, and fatigue. Doctors use an electrocardiogram (ECG) to diagnose it.
Atrioventricular (AV) Blocks
Atrioventricular (AV) blocks happen when there’s a delay in electrical signals between the heart’s chambers. They can be mild or severe. They’re often caused by aging, heart disease, or medications. Treatment depends on the block’s severity and symptoms.
Pacemaker Therapy Indications
Pacemakers are often used to treat bradyarrhythmias. They’re small devices that help the heart beat at a normal rate. They’re used for symptoms like slow heart rate and severe AV blocks. The decision to get a pacemaker depends on symptoms and heart health.
Common symptoms of bradyarrhythmias include:
- Fatigue
- Dizziness
- Shortness of breath
- Fainting
“The use of pacemakers has revolutionized the treatment of bradyarrhythmias, significantly improving the quality of life for many patients.”
– Dr. John Smith, Cardiologist
Supraventricular Tachycardias: Rapid Heart Rhythms
Supraventricular tachycardias are heart rhythm disorders with fast heartbeats starting above the ventricles. They happen due to odd electrical activity in the heart’s atria. This leads to different symptoms and how they show up clinically.
AVNRT (Atrioventricular Nodal Reentrant Tachycardia)
AVNRT is a common type of supraventricular tachycardia. It happens when there’s a loop in the AV node causing a fast heart rate. People often feel sudden palpitations with a regular beat. Doctors use an ECG to spot it, showing a narrow complex tachycardia.
AVRT (Atrioventricular Reciprocating Tachycardia)
AVRT is when there’s an extra electrical path between the atria and ventricles. This can make the heart beat too fast. Wolff-Parkinson-White syndrome is a known cause of AVRT. An ECG can show delta waves and a short PR interval during normal heart rhythm.
Atrial Tachycardia
Atrial tachycardia is a fast heart rhythm starting in the atria. It can be due to heart disease, imbalances in electrolytes, or some medicines. Doctors use ECG to find a P wave that looks different from normal, often with a fast heart rate.
Diagnosis and Differentiation
Doctors use a mix of clinical checks, ECGs, and sometimes more tests like Holter monitoring or electrophysiological studies to diagnose. It’s key to tell the different types apart for the right treatment. Treatments include vagal maneuvers, medicines, or catheter ablation for severe cases.
Premature Beats: PACs and PVCs
Premature beats, like PACs and PVCs, are irregular heartbeats from different heart parts. They can feel like a skipped beat or a flutter in the chest. Many people experience them.
Premature Atrial Contractions (PACs)
PACs start in the atria, causing early heart contractions. They are usually harmless and can be caused by stress, caffeine, or some medicines.
People with PACs might feel skipped beats or an irregular heartbeat. Usually, they don’t need treatment. But, cutting down on stress and caffeine can help.
Premature Ventricular Contractions (PVCs)
PVCs start in the ventricles, causing early heartbeats. They can feel like skipped beats or palpitations. Stress, caffeine, or heart issues can trigger them.
Even though PVCs are often okay, too many can mean a health issue. To treat PVCs, try reducing stress and avoiding stimulants.
Management and Lifestyle Modifications
Managing premature beats often means changing your lifestyle. This includes cutting down on caffeine and alcohol, managing stress, and exercising regularly.
In some cases, doctors might prescribe medicine. Always follow your doctor’s advice and report any changes in symptoms or how often they happen.
| Lifestyle Modification | Benefit |
| Reducing Caffeine Intake | Decreases frequency of premature beats |
| Managing Stress | Reduces triggers for PACs and PVCs |
| Regular Exercise | Improves overall heart health |
Inherited Arrhythmia Syndromes
Inherited arrhythmia syndromes are genetic disorders that can cause serious heart rhythm problems. These conditions happen when genes that control the heart’s electrical system are mutated.
Long QT Syndrome
Long QT syndrome is a well-known inherited arrhythmia syndrome. It’s marked by a long QT interval on an electrocardiogram (ECG). This condition raises the risk of a dangerous heart rhythm called Torsades de Pointes, which can lead to sudden cardiac death.
Key Features of Long QT Syndrome:
- Prolonged QT interval on ECG
- Risk of Torsades de Pointes and sudden cardiac death
- Often presents with syncope or seizures
- Can be triggered by exercise, stress, or certain medications
Brugada Syndrome
Brugada syndrome is another significant inherited arrhythmia syndrome. It’s known for a unique ECG pattern with ST-segment elevation in leads V1-V3. This condition increases the risk of ventricular fibrillation and sudden cardiac death, often at rest or during sleep.
Key Features of Brugada Syndrome:
- Distinctive ECG pattern with ST-segment elevation
- Risk of ventricular fibrillation and sudden cardiac death
- More common in males
- Often diagnosed in adulthood
Catecholaminergic Polymorphic Ventricular Tachycardia
Catecholaminergic polymorphic ventricular tachycardia (CPVT) is a rare but dangerous inherited arrhythmia syndrome. It causes ventricular tachycardia triggered by physical or emotional stress.
Key Features of CPVT:
- Ventricular tachycardia triggered by stress or exercise
- Often presents with syncope or sudden cardiac arrest
- Can be difficult to diagnose due to normal resting ECG
- Requires genetic testing for diagnosis
Genetic Testing and Family Screening
Genetic testing is key in diagnosing and managing inherited arrhythmia syndromes. Finding the genetic cause in a family allows for targeted screening of relatives. This can prevent sudden cardiac death.
| Inherited Arrhythmia Syndrome | Key Genetic Features | Clinical Presentation |
| Long QT Syndrome | Mutations in KCNQ1, KCNH2, SCN5A | Syncope, seizures, sudden cardiac death |
| Brugada Syndrome | Mutations in SCN5A | Ventricular fibrillation, sudden cardiac death at rest |
| Catecholaminergic Polymorphic Ventricular Tachycardia | Mutations in RYR2, CASQ2 | Syncope, ventricular tachycardia during stress or exercise |
We suggest genetic testing and screening for those with a family history of inherited arrhythmia syndromes. Early detection and proper management can greatly reduce the risk of dangerous arrhythmias.
Conclusion: Living With and Managing Cardiac Arrhythmias
Managing cardiac arrhythmia well means knowing a lot about it and sticking to treatment plans. We stress the need for lifestyle changes, medicines, and devices to handle arrhythmias.
People with arytmia or arrythmic issues need to team up with their doctors to create a treatment plan that fits them. Knowing the arrhythmia abbreviation and medical terms helps patients be more involved in their care.
By being proactive in managing cardiac arrhythmias, people can live better and avoid serious problems. We urge patients to stay informed and involved in their care to get the best results.
FAQ
What is cardiac arrhythmia?
Cardiac arrhythmia is when your heartbeat is not regular. It happens because of abnormal electrical signals in your heart.
What is the difference between dysrhythmia and arrhythmia?
Dysrhythmia and arrhythmia are often used the same way. But, some doctors make a small difference. Dysrhythmia means any abnormal heart rhythm. Arrhythmia means an irregular or missing heartbeat.
What are the symptoms of atrial fibrillation?
Symptoms of atrial fibrillation include heart palpitations and irregular heartbeat. You might also feel short of breath, tired, or dizzy. Some people don’t feel any symptoms at all.
How is ventricular tachycardia treated?
Treatment for ventricular tachycardia depends on the cause and how severe it is. It might include cardioversion, medicines like anti-arrhythmics or beta blockers, or an implantable cardioverter-defibrillator (ICD).
What is the most common type of cardiac arrhythmia?
Atrial fibrillation (AFib) is the most common type. It’s when your heart beats fast and irregularly.
What are the risk factors for developing cardiac arrhythmias?
Risk factors include age, high blood pressure, heart disease, diabetes, obesity, and a family history of arrhythmias.
Can cardiac arrhythmias be inherited?
Yes, some arrhythmias like long QT syndrome and Brugada syndrome can be passed down through genes.
How are premature atrial contractions (PACs) and premature ventricular contractions (PVCs) managed?
Managing PACs and PVCs involves lifestyle changes. This includes reducing stress, avoiding stimulants, and exercising regularly. Medicines can also help control symptoms.
What is the purpose of a pacemaker in treating bradyarrhythmias?
A pacemaker helps regulate the heartbeat in people with bradyarrhythmias. It does this by sending electrical impulses to the heart.
How can I manage my cardiac arrhythmia and improve my quality of life?
Managing cardiac arrhythmia means understanding your condition and following your treatment plan. Making lifestyle changes and working with your doctor are also key. This helps monitor and adjust your treatment as needed.
References:
- Chaudhry, R. (2022). Physiology, Cardiovascular. In StatPearls. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK493197/









