Last Updated on December 2, 2025 by Bilal Hasdemir

Gastrointestinal (GI) bleeding is a big worry for seniors. About 100,000 people in the United States go to the hospital every year for upper GI bleeding. The elderly are hit hard by this issue. What is the #1 elderly GI bleed cause? We reveal the surprising, common culprit and other critical, age-related risk factors.
As people get older, changes in their body and health problems raise the risk of GI bleeding. Peptic ulcer disease, diverticulosis, and cancer in the GI tract are common causes. These can lead to serious bleeding if not treated right away.
It’s key to know why GI bleeding happens in older adults to help them better. Understanding the causes allows for the development of targeted plans to reduce the risk of bleeding. This can make a big difference in how well seniors do.
Key Takeaways
- Gastrointestinal bleeding is a big worry for older people.
- Age and health problems make GI bleeding more likely.
- Peptic ulcers, diverticulosis, and cancer are common causes.
- Knowing the causes helps in caring for and preventing GI bleeding.
- Targeted plans can help lower the risk of GI bleeding and improve outcomes.
Overview of Gastrointestinal Bleeding in the Elderly

It’s important to understand GI bleeding in older adults to find its causes and treat it right. GI bleeding is when blood is lost from the GI tract, which includes the esophagus, stomach, small intestine, and colon. It can show up as upper GI bleeding, with symptoms like vomiting blood or black, tarry stools. Or, it can be lower GI bleeding, with fresh blood in the stool.
Definition of GI Bleeding
GI bleeding is when blood is lost from the GI tract. It can be mild or very serious, even life-threatening if not treated quickly. The causes can be ulcers, vascular lesions, or inflammatory conditions.
Importance of Identifying Sources
Finding out where the bleeding is coming from is key to treating it. Different problems need different treatments. For example, bleeding ulcers might need immediate care. We also need to think about the patient’s health and any medicines they take.
Statistics on Prevalence in Older Adults
GI bleeding is more common in older adults. This is because of age-related changes, chronic diseases, and certain medicines. Studies show that GI bleeding gets more common with age, making it a big worry for the elderly.
Age Group | Incidence of GI Bleeding (per 100,000) | Common Causes |
65-74 years | 120 | Peptic ulcer disease, diverticulosis |
75-84 years | 170 | Gastroesophageal reflux disease (GERD), angiodysplasia |
85 years and older | 220 | Diverticulitis, ischemic colitis |
The table shows how GI bleeding gets more common with age. It also lists some common causes for different age groups in the elderly. Knowing these facts helps healthcare providers treat GI bleeding in older adults better.
Common Causes of GI Bleeding in the Elderly
It’s important to know why older adults get GI bleeding. As we get older, we’re more likely to face conditions that can cause bleeding in the gut. We’ll look at the main reasons, like peptic ulcers, diverticulosis, and GERD.
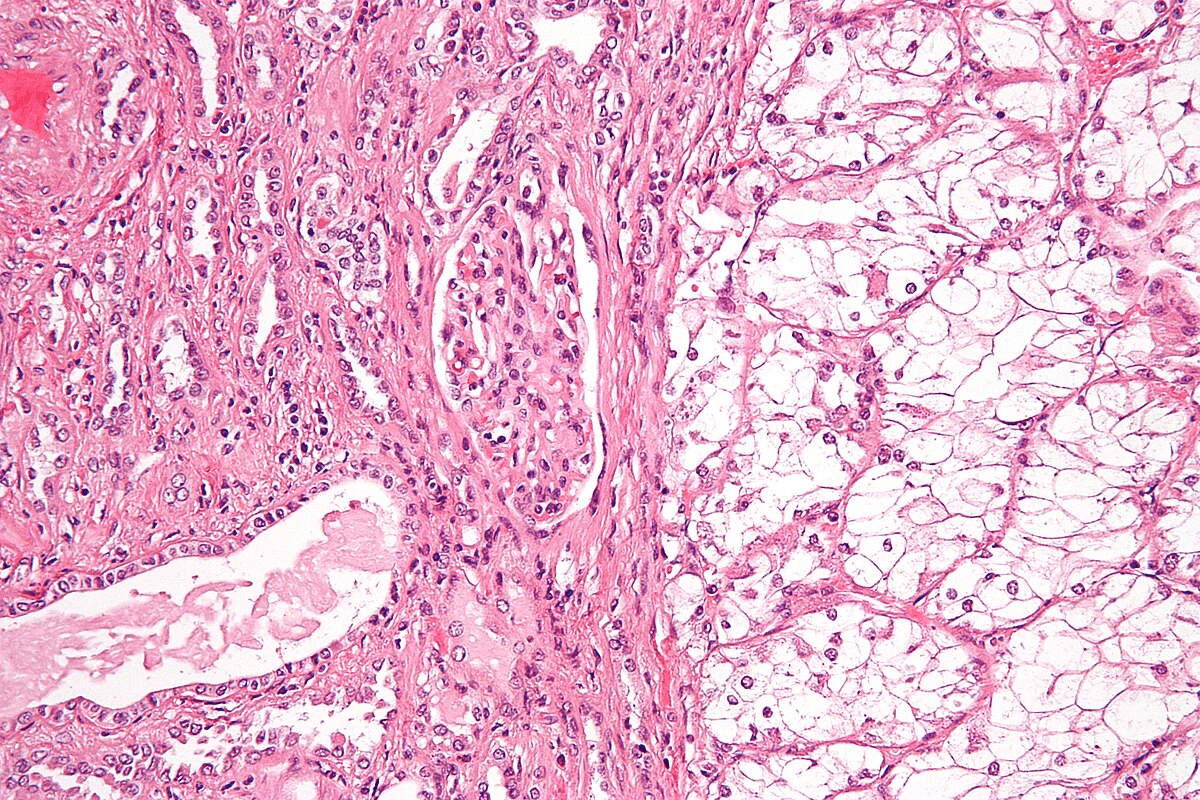
Peptic Ulcer Disease
Peptic ulcers are a big reason for GI bleeding in seniors. Peptic ulcers are sores in the stomach or small intestine. The chance of bleeding from these ulcers goes up with age, mainly for those on NSAIDs. Knowing the signs and risks of peptic ulcers is key to acting fast.
Diverticulosis and Diverticulitis
Diverticulosis is common in older adults. It’s when small pouches form in the colon wall. While often without symptoms, it can cause diverticular bleeding. Diverticulitis, an inflammation of these pouches, can make things worse.
Gastroesophageal Reflux Disease (GERD)
GERD can also lead to GI bleeding, though it’s less common. It’s when stomach acid flows back into the esophagus. This can cause inflammation and, rarely, bleeding. Treating GERD well can lower this risk.
It’s important to remember that these issues can happen together or get worse with other health problems or medicines. So, treating GI bleeding in the elderly needs a full plan.
Medications Linked to GI Bleeding
Certain medications can increase the risk of GI bleeding in older adults. As we age, our bodies change, affecting how we process drugs. This can lead to more side effects. We’ll look at the drugs that often cause GI bleeding in seniors.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are used for pain and inflammation. But, they can irritate the stomach and harm it. This risk grows with long-term use or high doses.
Anticoagulants and Antiplatelet Agents
Drugs that prevent blood clotting, like anticoagulants and antiplatelet agents, can cause GI bleeding. They’re important for heart health but can lead to bleeding. It’s key to watch their dosage closely.
Corticosteroids Impact
Corticosteroids are strong anti-inflammatory drugs. But, they can increase the risk of GI bleeding, even more with NSAIDs. It’s important to consider the risks when prescribing them to seniors.
In summary, while NSAIDs, anticoagulants, antiplatelet agents, and corticosteroids are helpful, they can cause GI bleeding in the elderly. Doctors must be aware of these risks and monitor patients to avoid harm.
The Role of Chronic Conditions in GI Bleeding
Chronic conditions like liver disease, kidney disease, and heart problems raise the risk of GI bleeding in older adults. These conditions can make diagnosing and treating GI bleeding more complex. We will look into how these conditions affect GI bleeding risk and presentation in the elderly.
Liver Disease Complications
Liver disease is a big risk factor for GI bleeding in the elderly. Conditions like cirrhosis can cause portal hypertension, raising the chance of variceal bleeding. We will talk about how liver disease leads to GI bleeding and what it means for treatment.
Kidney Disease Connections
Kidney disease, mainly in its late stages, can up the risk of GI bleeding. This is because uremia can make platelets not work right. We will dive into the link between kidney disease and GI bleeding, focusing on the management hurdles.
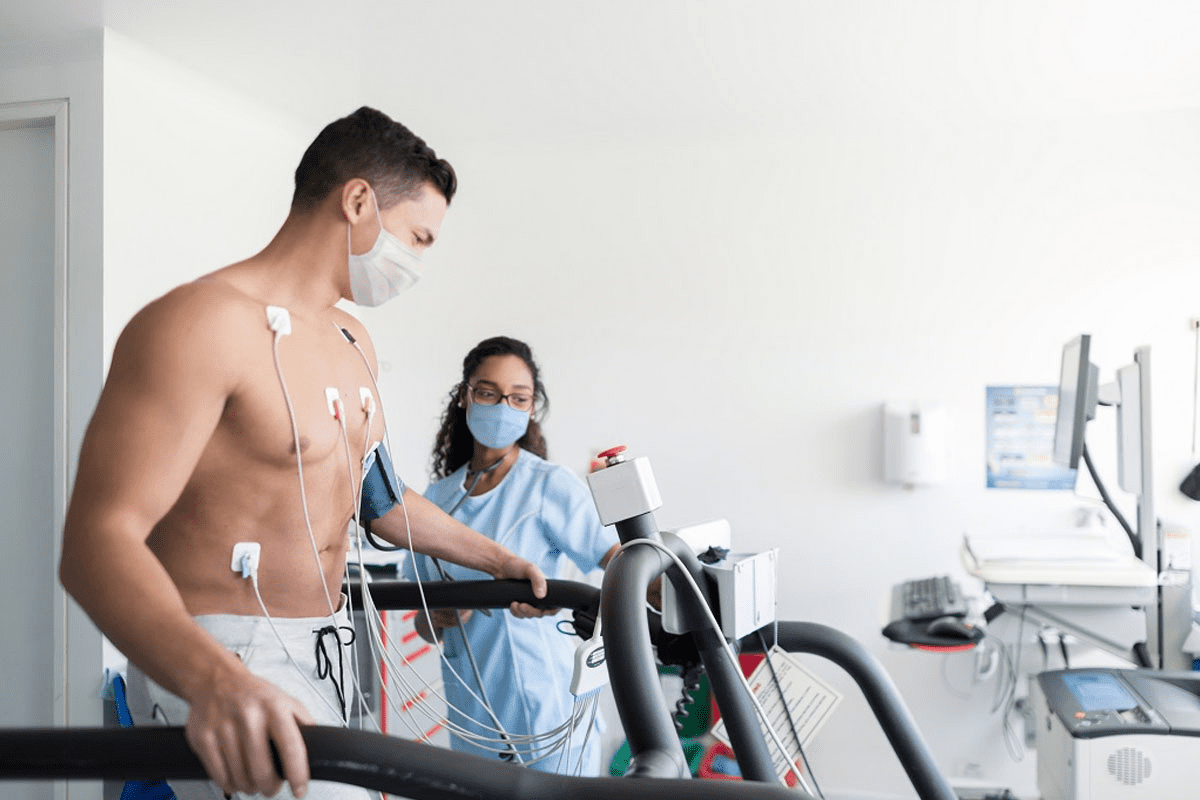
Cardiovascular Conditions Influence
Heart conditions, like atherosclerosis and heart failure, can indirectly lead to GI bleeding. This is because they often mean more use of blood thinners and less blood flow to the gut. We will discuss how these heart issues affect GI bleeding risk and management.
Chronic Condition | Mechanism Contributing to GI Bleeding | Implications for Management |
Liver Disease | Portal hypertension, variceal bleeding | Requires careful management of varices, consideration of beta-blockers |
Kidney Disease | Uremia-induced platelet dysfunction | May require adjustment of anticoagulant therapy, dialysis consideration |
Cardiovascular Conditions | Increased use of anticoagulants, reduced gut perfusion | Careful balancing of anticoagulant therapy, monitoring for GI bleeding signs |
Acute vs. Chronic GI Bleeding
It’s important to know the difference between acute and chronic GI bleeding. This knowledge helps in diagnosing and treating the condition. Gastrointestinal bleeding can be serious and needs quick action, depending on its type.
Differences in Symptoms
Acute GI bleeding starts suddenly. Symptoms include hematemesis (vomiting blood), melena (black, tarry stools), or hematochezia (passing fresh blood through the rectum). These signs can quickly get worse if not treated right away.
Chronic GI bleeding, on the other hand, has milder symptoms. It might cause iron deficiency anemia from slow blood loss. People might feel tired, weak, and short of breath, making it hard to find the cause.
Diagnostic Approach for Each Type
Diagnosing acute GI bleeding is urgent. First, check if the patient is stable. Then, use endoscopy to find where the bleeding is coming from.
Chronic GI bleeding needs a more detailed check. This includes:
- Complete blood count (CBC) to check for anemia
- Endoscopy to see inside the GI tract and find bleeding sources
- Imaging studies like CT scans or tagged red blood cell scans to spot bleeding areas
Treatment Protocols
Treatment for GI bleeding depends on the type and how bad it is. For acute bleeding, start with resuscitation and endoscopic therapy to stop the bleeding. Sometimes, surgical intervention or angiographic embolization is needed.
Chronic bleeding treatment aims to fix the cause. This might include medical therapy to lower acid or treat Helicobacter pylori infection. Also, iron supplementation might be needed to treat anemia.
Characteristics | Acute GI Bleeding | Chronic GI Bleeding |
Onset | Sudden | Gradual |
Symptoms | Hematemesis, melena, hematochezia | Iron deficiency anemia, fatigue, weakness |
Diagnostic Approach | Immediate endoscopy | CBC, endoscopy, imaging studies |
Treatment | Resuscitation, endoscopic therapy, possible surgery | Medical therapy, iron supplementation |
Risk Factors for GI Bleeding in the Elderly
The elderly face a higher risk of GI bleeding. This is due to changes in the GI tract with age, lifestyle choices, and other health conditions. As we get older, our GI system changes in ways that increase the risk of bleeding.
Age-Related Changes in the GI Tract
The GI tract becomes more prone to bleeding with age. The mucosa gets thinner, and blood flow decreases. This makes it more vulnerable to injury. Also, age-related vascular changes can lead to angiodysplasia, a condition with abnormal blood vessels that bleed easily.
Lifestyle Factors: Diet and Alcohol Use
Diet and alcohol use are key lifestyle factors that affect GI bleeding risk in the elderly. A diet low in fiber and high in processed foods can cause constipation. This increases the risk of diverticulitis, a condition that can lead to significant GI bleeding. Excessive alcohol use also irritates the GI mucosa, raising the risk of bleeding, even more in those with liver disease.
Comorbid Conditions
Comorbid conditions are another major risk factor for GI bleeding in the elderly. Liver disease, like cirrhosis, can cause portal hypertension. This increases the risk of variceal bleeding. Cardiovascular diseases and anticoagulant use also raise the risk of GI bleeding in this group.
It’s important to understand these risk factors to prevent and detect GI bleeding early in the elderly. By identifying those at higher risk, healthcare providers can take preventive steps and closely monitor them for signs of GI bleeding.
Symptoms Associated with GI Bleeding
Gastrointestinal (GI) bleeding in the elderly can show through different symptoms that need quick action. It’s important to know these symptoms to get medical help fast.
Identifying Common Symptoms
Signs of GI bleeding include vomiting blood or black tarry stools, showing upper GI bleeding. Passing bright red blood through the rectum points to lower GI bleeding. Other signs are abdominal pain, dizziness, and weakness from blood loss.
Elderly people might also feel fatigue, shortness of breath, and pale skin from losing a lot of blood. Knowing these signs is key to understanding how serious the bleeding is.
When to Seek Medical Attention
If someone elderly has severe abdominal pain, heavy bleeding, or signs of shock (like fainting or a fast heartbeat), they need to get medical help right away. Waiting too long can cause serious problems, like organ failure or death.
People with GI problems or taking medicines that raise bleeding risk (like anticoagulants or NSAIDs) should watch their symptoms closely. They should get medical help if they need it.
Variations in Symptoms Among Different Causes
The signs of GI bleeding change based on the cause and where the bleeding is. For example, peptic ulcers might cause epigastric pain and vomiting blood. On the other hand, diverticulosis might lead to painless passage of maroon or bright red blood.
Knowing these differences helps doctors figure out the cause of GI bleeding and treat it right. We’ll look into the different causes and symptoms in more detail to help with accurate diagnosis and treatment.
Diagnostic Methods for GI Bleeding
Diagnosing GI bleeding is complex. We use many tools to find the source and cause of bleeding. This helps us plan the best treatment.
Endoscopy Techniques
Endoscopy is key for diagnosing GI bleeding. It uses a flexible tube with a camera and light to see inside the GI tract. We can see the bleeding site and treat it directly.
Types of Endoscopy:
- Upper GI Endoscopy: Looks at the esophagus, stomach, and duodenum.
- Colonoscopy: Checks the colon and rectum.
- Enteroscopy: Examines the small intestine.
Imaging Studies
Imaging studies are also important for diagnosing GI bleeding. They help us see the GI tract and find bleeding sources.
Imaging Modalities:
- Ultrasound: Uses sound waves to create images of the GI tract and nearby areas.
- CT Scan: Uses X-rays to make detailed images of the abdomen.
Laboratory Tests
Laboratory tests help us understand how severe the bleeding is. We use:
- Complete Blood Count (CBC): Checks for blood loss and anemia.
- Blood Chemistry Tests: Looks at liver and kidney function.
- Coagulation Studies: Finds coagulopathy.
By using these methods together, we can accurately diagnose GI bleeding. Then, we create a treatment plan that fits each patient’s needs.
Management Strategies for GI Bleeding
Managing GI bleeding in the elderly needs a detailed plan. This includes quick care, possible surgery, and long-term plans. We’ll dive into these strategies to understand how to handle GI bleeding well.
Immediate Care and Stabilization
The first step in managing GI bleeding is to keep the patient stable. This means giving fluids and blood as needed to keep blood pressure stable. It’s also important to watch vital signs and check how bad the bleeding is.
- Administering oxygen if the patient is hypoxic
- Establishing intravenous access for fluid and medication administration
- Monitoring laboratory values, such as hemoglobin and hematocrit, to assess the severity of blood loss
A leading gastroenterologist says, “The key to managing GI bleeding is early recognition and intervention. Quick action can greatly improve results.”
“Early intervention is key in GI bleeding management, as it can stop complications and lower death rates.”
Gastroenterologist
Surgical Interventions
When GI bleeding is severe or doesn’t get better with simple care, surgical intervention might be needed. The surgery can be from simple endoscopic procedures to more complex surgeries, based on the cause and how bad the bleeding is.
- Endoscopic treatments, such as cauterization or clipping, to control bleeding
- Surgical removal of the affected area for severe or ongoing bleeding
We need to carefully choose the right surgery for each patient. This depends on their health, the cause of the bleed, and how bad it is.
Long-Term Management Approaches
Long-term GI bleeding management aims to prevent it from happening again and handle any underlying issues. This includes medication management, lifestyle changes, and regular doctor visits.
- Checking and adjusting medications that might cause GI bleeding, like NSAIDs and anticoagulants
- Making dietary changes to lower GI irritation risk
- Watching for signs of bleeding coming back and adjusting treatment as needed
By using a complete and varied approach to GI bleeding management, we can better patient outcomes and lower complication risks.
Preventive Measures for GI Bleeding
To lower the risk of GI bleeding, it’s key to know and use good prevention steps. As we get older, our risk for stomach problems goes up. So, preventing these issues is very important for older adults.
Regular Screening Recommendations
Regular checks are a big part of stopping GI bleeding. People, mainly those with stomach problems or risk factors, should get regular endoscopies. This helps find problems early.
- Annual or biennial endoscopy for individuals over 50 years old
- Screening for H. pylori infection, a known risk factor for peptic ulcer disease
- Fecal occult blood tests (FOBT) to detect hidden bleeding
Dietary Modifications for Protection
What we eat is very important for our stomach health. We suggest eating more fruits, veggies, and whole grains. These foods help protect against stomach bleeding.
Key dietary recommendations include:
- Increasing fiber intake to prevent diverticulitis
- Avoiding spicy or acidic foods that can irritate the GI tract
- Staying hydrated to prevent constipation
Medication Management Strategies
Some medicines, like NSAIDs and anticoagulants, can raise the risk of stomach bleeding. It’s very important to manage medicines carefully.
- Using alternative pain relief options when possible
- Monitoring and adjusting anticoagulant therapy under medical supervision
- Avoiding the concurrent use of NSAIDs and anticoagulants
By taking these steps, people can greatly lower their risk of stomach bleeding. It’s vital to work with doctors to make these plans fit each person’s needs.
Case Studies: Elderly Patients with GI Bleeding
Looking at real cases of elderly patients with GI bleeding gives us important insights. These studies show us the challenges and successes in treating this condition. They help us understand how to better care for these patients.
Notable Cases and Their Outcomes
Many case studies show the different ways GI bleeding affects elderly patients. For example, an 85-year-old patient with a history of NSAID use had severe melena. They were diagnosed with a bleeding peptic ulcer. The patient had to have emergency surgery due to rebleeding.
A 72-year-old patient with atrial fibrillation on anticoagulation therapy had hematemesis. This was caused by erosive gastritis. The treatment involved stopping anticoagulants, using proton pump inhibitors, and watching the patient’s hemoglobin levels closely.
- Key Takeaway: Knowing a patient’s medical history, including their medications, is key in assessing GI bleeding risk.
- Successful Strategy: Quick endoscopic evaluation and intervention when needed.
Lessons Learned from Case Studies
These studies teach us a lot. One important lesson is the need for a team approach in managing GI bleeding. Gastroenterologists, surgeons, and primary care physicians must work together for the best care.
Another lesson is the importance of preventive measures. This includes using gastroprotection for patients on NSAIDs or anticoagulants to lower the risk of GI bleeding.
- Identify the risk factors for GI bleeding in elderly patients.
- Use preventive strategies based on the patient’s risk profile.
- Use a team-based approach for complex cases.
Impact on Future Management Approaches
The insights from these studies will shape future management strategies. They show the need for personalized treatment plans. These plans should consider the patient’s health, medications, and preferences.
They also highlight the importance of ongoing education for healthcare providers. Providers need to stay updated on the latest guidelines and best practices for managing GI bleeding.
By applying these lessons, we can improve care for elderly patients with GI bleeding. This will help enhance their quality of life and survival.
Conclusion: Addressing Elderly GI Bleeding Causes
It’s key to understand why GI bleeding happens in older adults. We’ve looked at many reasons, like peptic ulcers, diverticulosis, and some medicines.
Good care for seniors with GI bleeding means managing risks and talking openly with doctors. This helps avoid serious problems and makes patients feel better.
Key Takeaways
Remember, finding out why GI bleeding happens is very important. Chronic conditions and regular checks play a big role. Knowing this helps doctors create good plans for care.
Comprehensive Care Approach
Good care goes beyond just treating the bleeding. It also looks at underlying health issues and lifestyle. This approach can really help seniors live better lives.
Open Communication
Talking openly is essential. It makes sure everyone involved in care is on the same page. This leads to better health for seniors.
FAQ
What are the most common causes of GI bleeding in the elderly?
In the elderly, GI bleeding often comes from peptic ulcers, diverticulosis, and GERD. These issues get worse with age due to changes in the GI tract and lifestyle factors.
How do certain medications contribute to GI bleeding in the elderly?
Medications like NSAIDs, anticoagulants, and corticosteroids can harm the GI tract. They can also stop blood from clotting properly, raising the risk of bleeding.
What are the symptoms of GI bleeding, and when should I seek medical attention?
Signs of GI bleeding include black stools, bloody stools, and stomach pain. If you see a lot of blood, feel dizzy, or have trouble breathing, get help right away.
How is GI bleeding diagnosed in the elderly?
Doctors use endoscopy, imaging like ultrasound, and blood tests to find GI bleeding. These tools help spot the cause and assess the damage.
What are the management strategies for GI bleeding in the elderly?
Treatment for GI bleeding includes immediate care and sometimes surgery. Long-term, doctors might change medications and suggest lifestyle changes to prevent future episodes.
Can GI bleeding be prevented in the elderly?
Some risks for GI bleeding can’t be avoided, but there are steps to lower the chance. Regular check-ups, diet changes, and managing medications can help.
How do chronic conditions like liver disease and kidney disease influence GI bleeding?
Liver and kidney diseases can make bleeding more likely. They affect blood clotting and can lead to ulcers and varices, increasing the risk of bleeding.
What is the difference between acute and chronic GI bleeding?
Acute bleeding is sudden and severe, needing quick medical help. Chronic bleeding is ongoing, slower, and often needs long-term care.
How do age-related changes in the GI tract contribute to GI bleeding?
As we age, the GI tract changes, leading to conditions like ulcers and diverticulosis. These changes can cause bleeding.
What lifestyle factors can increase the risk of GI bleeding in the elderly?
Poor diet, too much alcohol, and smoking can raise the risk of GI bleeding. These habits can lead to ulcers, diverticulosis, and GERD.
Reference:
BMJ (British Medical Journal). Evidence-Based Medical Insight. Retrieved from https://www.bmj.com/content/310/6989/985