Nearly 1 in 3 people with epilepsy keep having seizures even with medicine. But, epilepsy surgery is a hopeful option for seizure freedom Epilepsy surgery outcomes.
Recent studies show that surgery can greatly improve seizure control and quality of life for many. By removing or changing the brain part causing seizures, epilepsy surgery aims to lessen or stop seizures. This improves overall well-being.
The main aim of epilepsy surgery is not just to stop seizures. It’s also to boost the patient’s quality of life. Successful surgery can lead to better thinking, mental health, and more independence.
Key Takeaways
- Epilepsy surgery can significantly improve seizure control.
- Achieving seizure freedom is a primary goal of surgery.
- Quality of life often improves after successful surgery.
- Surgery is considered for patients with medication-resistant epilepsy.
- Improved cognitive function and mental health are possible benefits.
The Journey to Epilepsy Surgery
The path to epilepsy surgery starts with finding patients with drug-resistant epilepsy. It’s about checking if they can benefit from surgery. This step is key for those whose seizures don’t stop with medicine.
Drug-Resistant Epilepsy and Surgical Candidacy
People with drug-resistant epilepsy might get surgery. They’ve tried many medicines but their seizures keep coming back. Doctors look closely to see if surgery can help by removing or disconnecting the seizure source.
Pre-Surgical Evaluation Process
The pre-surgery check-up is detailed. It includes tests to see if surgery is right for the patient. Important parts are neuroimaging and electroclinical monitoring.
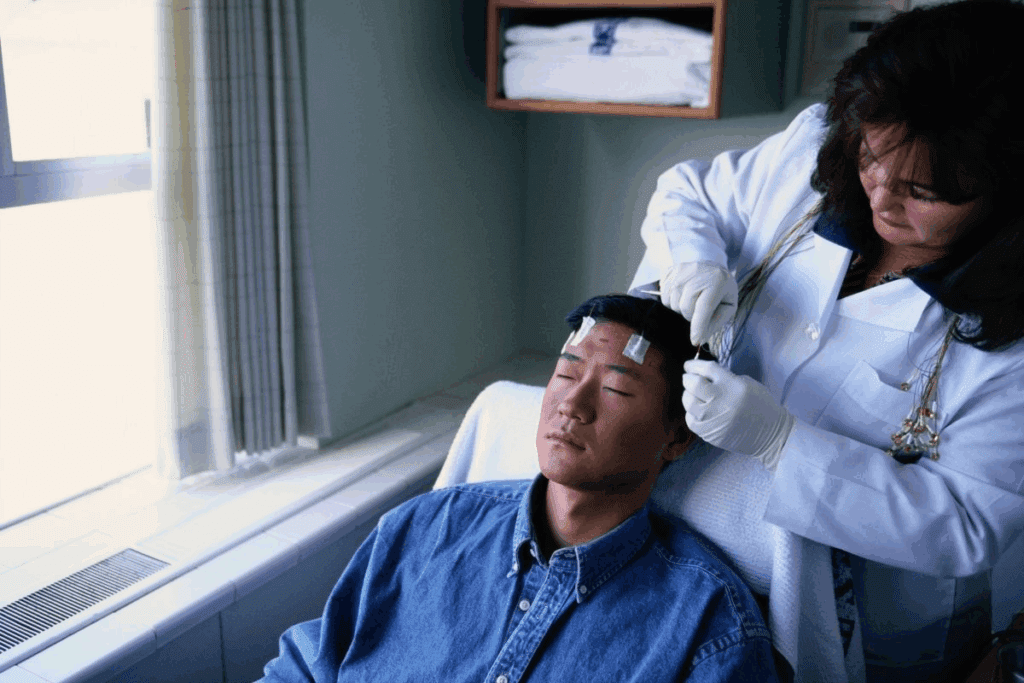
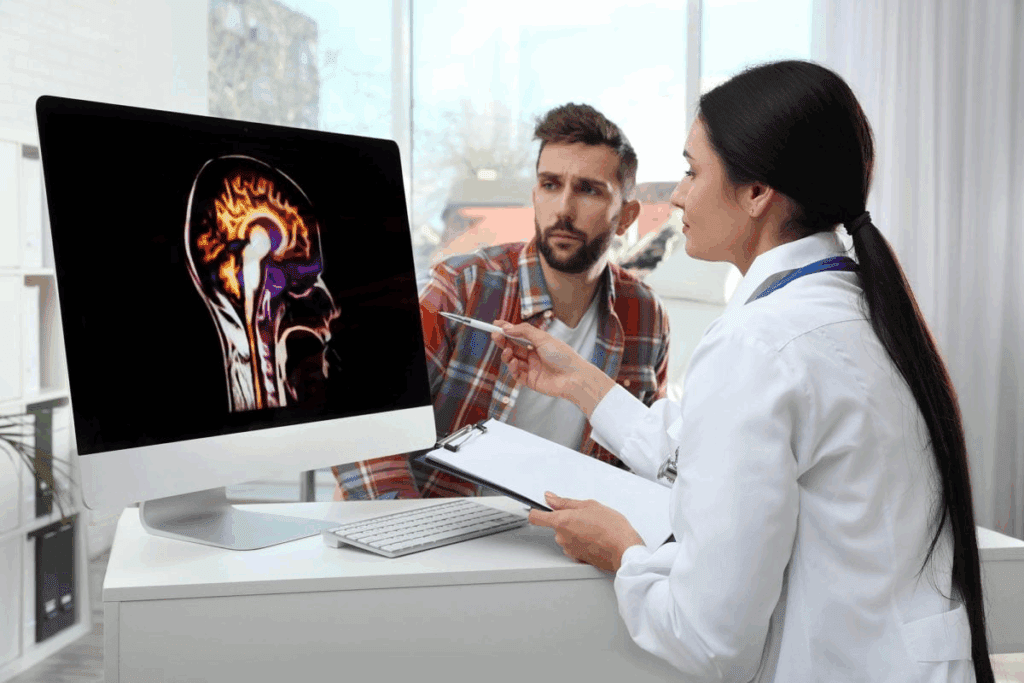
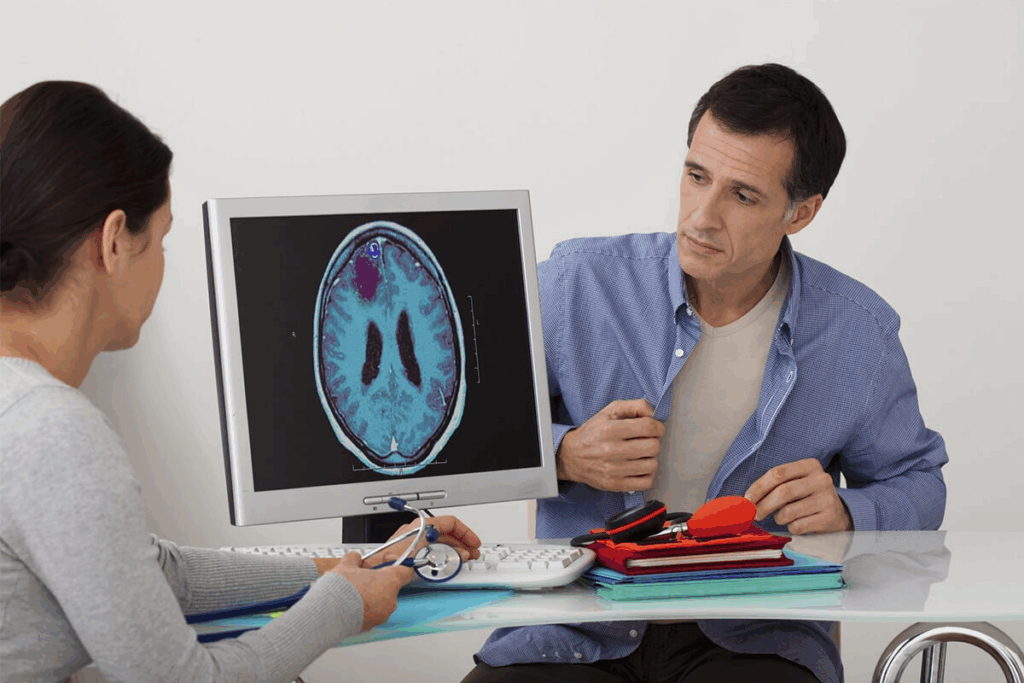
Neuroimaging and Electroclinical Monitoring
Neuroimaging like MRI and PET scans helps find the seizure source. Electroclinical monitoring, including EEG, links seizures to symptoms. This helps pinpoint where seizures start.
Functional mapping techniques check the brain’s function near the surgery area. This is important to avoid brain damage after surgery.
Doctors use all this info to choose the best surgery for each patient. They weigh the chance of fewer seizures against the surgery’s risks.
Types of Epilepsy Surgery Procedures
Epilepsy surgery has many procedures to help reduce or stop seizures. The right surgery depends on where and why seizures start, and the patient’s health.
Resective Surgery Techniques
Resective surgery removes the brain part where seizures start. It’s often chosen for those with drug-resistant epilepsy.
Temporal Lobe Resection
Temporal lobe resection is common for temporal lobe epilepsy. It removes the affected temporal lobe part.
Extratemporal Resection
Extratemporal resection is for seizures outside the temporal lobe. It needs exact location of the seizure area.
Disconnection Procedures
Disconnection procedures stop seizures from spreading without removing brain tissue. They’re used when other surgeries aren’t possible.
Corpus Callosotomy
Corpus callosotomy cuts or partially divides the corpus callosum. This major brain connection is severed. It’s used to lessen seizure severity.
Hemispherectomy and Hemispherotomy
Hemispherectomy and hemispherotomy remove or disconnect a big part of one brain hemisphere. They’re for severe, one-sided epilepsy.
In conclusion, there are many epilepsy surgery options. Each one is tailored to the patient’s needs. Knowing about these surgeries helps make better choices.
Epilepsy Surgery Outcomes: Seizure Control Rates
Epilepsy surgery is a treatment for those with drug-resistant epilepsy. It aims to control seizures, improving life quality. Seizure control rates show how well surgery works.
Short-term Seizure Freedom
Research shows epilepsy surgery can lead to short-term seizure freedom. Many see a big drop in seizures right after surgery. A lot of patients stop having seizures in the short term, but what’s short term can differ.
Long-term Seizure Control Statistics
Long-term data is key to seeing surgery’s lasting effects. Studies say 47% of patients stayed seizure-free for 5 years and 38% for 10 years after surgery. These numbers show surgery can control seizures long-term, but results vary.
Factors Affecting Seizure Freedom
Many things can affect if surgery will stop seizures. These include:
- The cause of epilepsy
- Where and how big the seizure area is
- The surgery type
- The patient’s health and brain status
Seizure Recurrence Patterns
Knowing when seizures might come back is important. Studies show seizures can return at any time after surgery. Things like leftover seizure tissue and stopping meds can affect when seizures come back.
Looking at both short and long-term seizure control helps doctors advise patients. They can better guide those thinking about epilepsy surgery.
Age-Specific Outcomes and Considerations
Epilepsy surgery results vary by age. It’s important to look at outcomes for different age groups.
Pediatric Epilepsy Surgery Results
Children who have epilepsy surgery often see big improvements. Pediatric epilepsy surgery outcomes are usually good. Many kids stop having seizures.
Developmental Outcomes in Children
Epilepsy surgery can help kids develop better. It reduces seizures, allowing kids to grow and reach their goals.
School Performance After Surgery
Good epilepsy surgery can help kids do better in school. With fewer seizures and less medicine, they can focus and learn more.
Adult Epilepsy Surgery Outcomes
Adults can also see big improvements from surgery. Adult epilepsy surgery outcomes show many patients have fewer and less severe seizures.
Employment and Independence
For adults, better seizure control means more work and independence. It opens up employment opportunities and helps them live on their own.
Age-Related Surgical Risks
While surgery is good for any age, older adults face special risks. These risks must be weighed against surgery’s benefits.
A recent study shows the importance of age in surgery decisions. “The outcomes of epilepsy surgery in children and adults demonstrate the importance of considering age-specific factors in the surgical evaluation process”
This highlights the need for treatment plans tailored to each patient’s unique situation.
Medication Management After Surgery
After surgery for epilepsy, managing your medication is key. The aim is to control seizures while reducing side effects from drugs.
Timeline for Medication Adjustments
Most patients stay on seizure medicines for at least two years after surgery. The time needed for adjusting medications varies. It depends on the surgery type and if seizures happen after surgery.
Complete Medication Freedom Possibilities
Some people hope to stop taking epilepsy drugs completely. But, this is not possible for everyone. The chance of stopping medication depends on several factors.
Factors Predicting Medication Reduction Success
Several things can predict if you can reduce or stop epilepsy drugs. These include the surgery’s success, any neurological issues, and your overall health.
Managing Medication Withdrawal
Stopping epilepsy drugs needs careful medical supervision. This is to avoid seizures. The process involves slowly reducing the drug amount.
| Factors | Influence on Medication Reduction |
| Surgical Outcome | Successful surgery increases chances of medication reduction |
| Seizure Activity Post-Surgery | Auras or seizures may necessitate continued medication |
| Patient Health | Overall health and absence of neurological deficits can favor reduction |
Cognitive and Neuropsychological Changes
Epilepsy surgery can change how we think and feel. It might help stop seizures but can also affect our brain. This is something patients and doctors need to think about.
Memory and Language Function Outcomes
Memory and language can change after surgery. How much and in what way depends on the surgery type.
Temporal Lobe Surgery Effects
Temporal lobe surgery can impact memory. Verbal memory might be affected, mainly if the surgery is on the dominant side. Research shows a higher risk of memory loss for those with surgery on the left side.
Extratemporal Surgery Effects
Extratemporal surgeries affect different parts of the brain. They can impact executive functions and motor skills. This depends on where the surgery is done.
Neuropsychological Assessment Results
Neuropsychological tests are key after surgery. They show how our brain works before and after surgery.
Pre-surgical vs. Post-surgical Cognitive Function
It’s important to compare brain function before and after surgery. Tests done before and after surgery help see any changes. This includes how memory, language, and other brain skills might improve or get worse.
Rehabilitation Strategies
Rehabilitation can help if brain function changes after surgery. Programs can improve memory, language, and other skills. A personalized plan can greatly improve a patient’s life and independence.
Quality of Life Improvements After Epilepsy Surgery
Epilepsy surgery does more than just stop seizures. It can greatly improve a person’s life. Studies show that successful surgery can lead to better mood, more confidence, and a sense of control.
Psychosocial Benefits
Epilepsy surgery brings psychosocial benefits that boost mental and emotional health. This is because fewer seizures mean less anxiety and fear.
Mood and Anxiety Improvements
Many see improvements in mood and reduced anxiety after surgery. This is because they no longer live in fear of seizures. They feel more in charge of their lives.
Social Reintegration
Social reintegration is a big plus. Patients feel more confident in social settings, without worrying about seizures. This leads to stronger friendships and a more rewarding social life.
Daily Activities and Functional Independence
Epilepsy surgery also helps with daily activities and achieving functional independence. With fewer seizures, people can work, learn, and enjoy life more.
Driving Privileges
Another big plus is getting driving privileges back. This is possible after a certain time without seizures. It boosts independence and freedom.
Educational and Vocational Achievements
Lastly, surgery can lead to better educational and vocational achievements. Improved seizure control means better school and work performance. This leads to a more stable and fulfilling life.
In summary, epilepsy surgery offers many benefits. It improves mental health, social life, and daily independence. For many, it’s a life-changing experience.
Potential Complications and Management
Epilepsy surgery brings hope to many, but it’s important to know the possible complications. Like any surgery, it has risks that can affect how well a patient does.
Immediate Postoperative Complications
Right after surgery, patients might face issues like problems at the surgical site and neurological problems. Surgical site issues could be infections or problems with the wound. These are usually treated with antibiotics or more surgery.
Surgical Site Issues
Infections or trouble with the wound healing can happen. This means patients need to be closely watched and might need extra treatment.
Neurological Deficits
Neurological problems, like weakness or changes in feeling, can happen after surgery. These are often short-term but can sometimes last forever.
Long-term Adverse Effects
Long-term issues might include vision problems and changes in mood or behavior. It’s important to know about these possible long-term effects to take good care of patients.
Visual Field Defects
Some people might see vision problems after surgery, like blind spots. This is more likely if the surgery was near the visual pathways.
Psychiatric Outcomes
Changes in mood or behavior can also happen. Patients might need help from a mental health professional to manage these changes.
| Complication Type | Potential Complications | Management Strategies |
| Immediate Postoperative | Surgical site issues, neurological deficits | Antibiotics, additional surgery, rehabilitation |
| Long-term | Visual field defects, psychiatric outcomes | Rehabilitation, psychiatric care |
Managing these complications well is key to helping patients get the best results from surgery. Knowing the risks and benefits helps doctors and nurses support patients better.
Conclusion: The Future of Epilepsy Surgery
The field of epilepsy surgery is changing fast. This is thanks to new surgical methods, better imaging, and how we choose patients. A team effort in treating epilepsy is key to better results.
Epilepsy surgery helps a lot of people who don’t get better with medicine. It can make seizures less frequent and less severe. There are different ways to do surgery, each with its own benefits.
As we move forward, new technology and teamwork among doctors will be vital. By using the latest in surgery and caring for patients before and after surgery, we can do even better. This will help those with epilepsy get the best treatment possible.
FAQ
What are the benefits of epilepsy surgery?
Epilepsy surgery can greatly improve life for those with seizures. Many patients see a big drop in seizure frequency or even stop having seizures altogether.
How is surgical candidacy determined for epilepsy surgery?
To see if surgery is right, doctors do a detailed check. This includes brain scans and tests to find the seizure source. They also check if the area is near important brain parts.
What are the different types of epilepsy surgery procedures?
There are a few main surgeries for epilepsy. These include removing parts of the brain and cutting connections between brain halves. Each type aims to stop seizures.
What are the seizure control rates after epilepsy surgery?
How well surgery works varies. But, many people see a big drop in seizures. Some studies show up to 80% of patients can stop having seizures.
How does epilepsy surgery affect cognitive function?
Surgery can change how the brain works. Some people might get better at remembering things or speaking. But, others might see changes, like trouble with memory or language.
Can epilepsy surgery improve quality of life?
Yes, surgery can make life better. People might feel more independent and have more energy. They can also drive again and do better in school or work.
What are the possible complications of epilepsy surgery?
Surgery can have risks. Right after surgery, there might be infections or problems with brain function. Long-term, there could be changes in how the brain works.
How is medication managed after epilepsy surgery?
After surgery, doctors slowly reduce medication. The goal is to use as little as possible. This depends on how well the patient controls seizures.
What is the role of a multidisciplinary team in epilepsy surgery?
A team of doctors and experts is key. They help decide if surgery is right, do the surgery, and care for patients after. This team aims to get the best results.
What are the age-specific outcomes of epilepsy surgery?
Surgery results vary by age. Kids often see big improvements in development and seizures. Adults might feel better about their seizures and life in general.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC12240976/