Last Updated on December 3, 2025 by Bilal Hasdemir

Nearly 500,000 spinal surgeries happen every year in the United States. Laminectomy is one of them, aimed at relieving pressure on the spinal cord or nerves. But not everyone can have this surgery. Patients go through detailed checks to see if they qualify. Learn the essential laminectomy contraindications. Understand who is not a suitable candidate for the surgery and the alternative options clearly.
Laminectomy involves removing part of the vertebrae to relieve spinal cord or nerve pressure, but certain risks and contraindications may make some patients unsuitable for this procedure. We’ll look at what makes someone a good fit for laminectomy.
Key Takeaways
- Understanding the risks associated with laminectomy is key.
- Certain spinal conditions may make laminectomy riskier.
- Pre-existing health conditions can impact eligibility for laminectomy.
- Age and overall health are important in deciding if someone can have laminectomy.
- A detailed medical check is needed before laminectomy.
Understanding Laminectomy: A Brief Overview

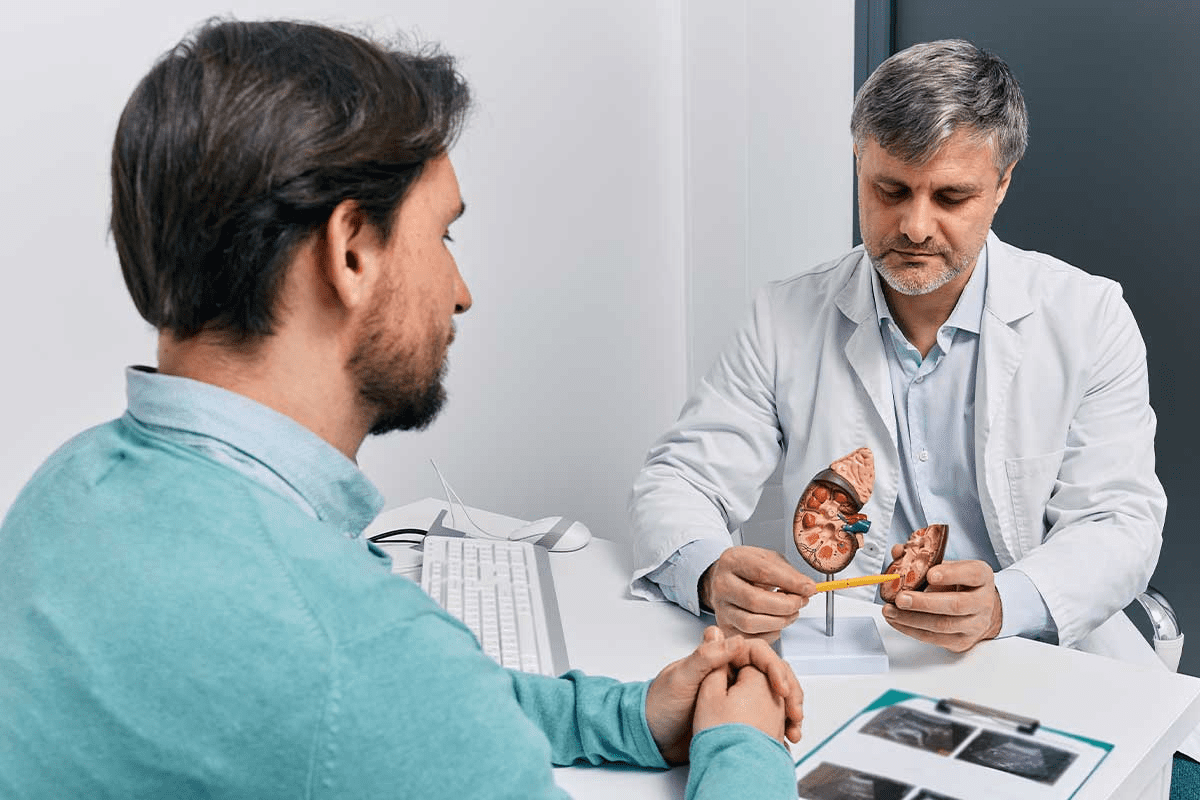
Laminectomy is a surgery used to treat many spinal problems. It removes part or all of a vertebra called the lamina. This helps relieve pressure on the spinal cord or nerves.
What is a laminectomy procedure?
A laminectomy is done under general anesthesia. The surgeon makes a cut in the back and moves muscles aside. Then, they remove the lamina to reach the spinal canal.
This process helps to ease symptoms like pain, numbness, or weakness in the legs. It’s a common surgery for many spinal issues, giving patients much-needed relief.
Common reasons for performing a laminectomy
Laminectomy is often needed for spinal stenosis. This is when the spinal canal narrows, putting pressure on nerves. It’s also used for herniated discs or bone spurs.
The main goal is to reduce pain, numbness, or weakness by freeing up the nerves.
- Spinal stenosis
- Herniated discs
- Nerve compression
General eligibility criteria
To get a laminectomy, patients usually need to have tried other treatments first. These might include physical therapy, medicine, or injections. The decision to have surgery depends on how bad the symptoms are and how they affect daily life.
We look at each patient’s health and their spinal condition to see if surgery is right for them. We also check for any conditions that might make surgery risky or less effective.
Laminectomy Contraindications: The Complete List

Before getting a laminectomy, it’s key to know what might make it risky or not right for you. This surgery helps relieve pressure on the spinal cord or nerves. But, it’s not for everyone due to certain health issues or spinal problems.
Absolute vs. Relative Contraindications
There are two types of contraindications for laminectomy: absolute and relative. Absolute contraindications are conditions that make surgery too risky. These include active infections, severe spinal instability, or some neurological conditions that could get worse with surgery.
Relative contraindications are conditions that might raise the surgery’s risks but don’t always mean no surgery. These include mild spinal instability, previous spinal surgeries, or some health issues that need to be managed first.
| Contraindication Type | Examples | Considerations |
| Absolute | Active infections, severe spinal instability, certain neurological conditions | Significant risk, surgery generally not recommended |
| Relative | Mild spinal instability, previous spinal surgeries, certain comorbidities | Increased risk, requires careful assessment and management |
Risk-Benefit Assessment Process
Deciding on laminectomy involves a detailed risk-benefit check. Doctors look at the patient’s health, how bad their spinal issue is, and what surgery might offer against the risks. This check is key to see if the patient is right for laminectomy.
They consider the patient’s age, other health issues, and any contraindications. They aim to make sure surgery’s benefits are greater than its risks. They want to ensure the patient will likely see a big improvement.
By looking at these factors, doctors can make smart choices about laminectomy. This helps ensure the best results for their patients.
Spinal Instability as a Major Contraindication
Spinal instability can make laminectomy procedures more complicated. It happens when vertebrae move too much, stressing the spinal cord and nerves. This can be due to wear and tear, injuries, or birth defects.
Types of Spinal Instability
There are different types of spinal instability. Degenerative instability comes from wear and tear, like in degenerative disc disease. Traumatic instability is caused by injuries, such as fractures or dislocations. Post-surgical instability can happen after surgeries, if too much is removed.
Why Instability Increases Surgical Risk
Spinal instability raises the risk of complications during laminectomy. Removing parts of the vertebrae can make the spine even more unstable. This can cause nerve or spinal cord compression, leading to further surgery needs.
Alternative Treatments for Unstable Spines
For unstable spines, treatments other than laminectomy might be better. Spinal fusion is often used, where unstable segments are fused together. This can prevent further problems. Other options include bracing, physical therapy, or pain management, depending on the case.
Spondylolisthesis and Surgical Risk Assessment
The severity of spondylolisthesis is key in understanding the risks of laminectomy. Spondylolisthesis is when a vertebra slips out of place. This can affect how stable the spine is.
Knowing the grades of spondylolisthesis helps us see the surgical risks. Grades range from I to IV, with I being the least severe and IV the most.
Grades of Spondylolisthesis
The grading is based on how much the vertebra slips:
- Grade I: 0-25% slippage
- Grade II: 26-50% slippage
- Grade III: 51-75% slippage
- Grade IV: 76-100% slippage
Higher grades mean more instability and higher risks during laminectomy.
When Spondylolisthesis Makes Laminectomy Dangerous
Laminectomy is risky for those with high-grade spondylolisthesis. It can make the spine even more unstable. This raises the risk of nerve damage or needing more surgery.
Alternative Surgical Approaches
For those with severe spondylolisthesis, spinal fusion might be suggested. It’s an alternative or addition to laminectomy. Spinal fusion joins vertebrae to stabilize the spine.
We look at many factors to choose the best surgery. These include the spondylolisthesis grade, spinal health, and the patient’s symptoms and needs.
Severe Spinal Deformities: Scoliosis and Kyphosis
Severe spinal deformities like scoliosis and kyphosis can make laminectomy tricky. These conditions cause abnormal spine curvatures. This can affect the spine’s stability and structure.
Complications Caused by Severe Curvatures
Severe scoliosis and kyphosis complicate laminectomy in several ways. The abnormal curvature makes it hard to reach the vertebrae. Also, the deformity can cause instability after surgery, raising the risk of complications.
Instability is a big worry as it might need more surgery to fix the spine.
Patients with severe deformities have unique spinal anatomy. This makes it hard to find landmarks during surgery. A detailed preoperative check is needed to plan the surgery well.
Measurement Thresholds for Contraindication
Some measurements show when laminectomy is too risky. For scoliosis, the Cobb angle is key. A Cobb angle over 40 degrees is seen as serious, making surgery riskier as the angle grows. Kyphosis is judged by the sagittal alignment, with angles over 60 degrees considered severe.
| Condition | Measurement | Threshold for Contraindication |
| Scoliosis | Cobb Angle | > 40 degrees |
| Kyphosis | Kyphotic Angle | > 60 degrees |
Alternative Treatment Options
For severe scoliosis or kyphosis, other treatments might be better. These include bracing, physical therapy, and pain management. Sometimes, a bigger surgery like spinal fusion or osteotomy is needed.
It’s important to think about the risks and benefits of surgery. This includes the patient’s health, the deformity’s severity, and how much quality of life can improve.
Mild Stenosis: When Surgery is Not Justified
When thinking about laminectomy for spinal stenosis, it’s key to know that mild cases might not need surgery. Spinal stenosis is when the spinal canal gets narrower. This can press on the spinal cord and nerves. How severe the stenosis is helps decide the best treatment.
Defining Mild vs. Severe Stenosis
Mild stenosis means a small narrowing of the spinal canal. Severe stenosis means a big narrowing, which can cause more symptoms. Knowing the difference is important for choosing the right treatment.
Doctors use imaging like MRI or CT scans to see how narrow the canal is. These images help them figure out how much narrowing there is and how it affects nerves.
Conservative Treatment Options
For mild stenosis, doctors usually suggest non-surgical treatments first. These can include:
- Physical therapy to make movements easier and muscles stronger
- Medicines like NSAIDs to lessen pain and swelling
- Epidural steroid injections to reduce swelling around nerves
- Changes in lifestyle, like losing weight and doing gentle exercises
These methods aim to ease symptoms, improve function, and maybe avoid surgery.
Monitoring Progression Guidelines
It’s important to keep an eye on mild stenosis to see if it gets worse. Monitoring guidelines might include:
- Regular check-ups to see how symptoms and function are
- Imaging studies now and then to check the canal’s size
- Changing the treatment plan if symptoms or changes in the canal happen
By watching the condition closely, doctors can decide when to act. This ensures patients get care that fits their needs.
Prior Spinal Hardware and Surgical Conflicts
Previous spinal hardware can make laminectomy procedures harder. If a patient has had spinal surgery before, hardware like rods, screws, or cages can pose challenges. We must carefully evaluate these cases to find the best solution.
Types of Implants that Complicate Laminectomy
Several spinal implants can complicate laminectomy. These include:
- Pedicle screw systems: These are commonly used in spinal fusion surgeries and can make it challenging to access the lamina.
- Interbody cages: Used for spinal fusion, these devices can alter the anatomy and make decompression more difficult.
- Spinal rods: Rods used in scoliosis correction or other deformity surgeries can limit access to certain areas of the spine.
Knowing the type and location of previous implants is key for a successful laminectomy.
Revision Surgery Considerations
When planning a laminectomy for a patient with prior spinal hardware, we must consider several factors. These include:
- The reason for the previous surgery and the type of hardware used.
- The current condition of the spine and the presence of any new or ongoing issues.
- The need to remove or modify existing hardware during the laminectomy.
Careful planning and a deep understanding of the patient’s history are vital for successful revision surgery.
Imaging Requirements for Assessment
Advanced imaging is key for assessing patients with prior spinal hardware for laminectomy. We usually use:
- CT scans: To evaluate the bony anatomy and the position of any hardware.
- MRI: To assess soft tissue, including nerves and any areas of compression.
- X-rays: To provide an overall view of spinal alignment and hardware position.
These imaging studies help us understand the case’s complexity and plan the best surgical approach.
Neurological Contraindications
Some neurological conditions can make laminectomy surgery risky or not recommended. Spine surgeons must carefully check for these conditions before deciding on surgery.
Recent Brain Trauma or Surgery
Having had recent brain trauma or surgery is a big no-go for laminectomy. People with recent head injuries or brain surgery face higher risks during and after the surgery. The recovery from brain trauma or surgery is complex, and adding another surgery could harm their health.
A study in the Journal of Neurosurgery found that those with recent brain trauma face more complications after surgery. This includes getting worse neurologically.
“The presence of recent brain trauma or surgery necessitates a cautious approach when considering laminectomy, as the risks may outweigh the benefits.”
A Neurosurgeon
Stroke History and Surgical Risk
Having had a stroke is another reason to think twice about laminectomy. People with stroke history might have vascular issues that raise surgery risks. It’s important to check their vascular health before deciding on surgery.
| Stroke History | Surgical Risk | Considerations |
| Recent stroke (<6 months) | High | Postpone surgery if possible |
| Previous stroke (>6 months) | Moderate | Assess vascular health |
| No stroke history | Low | Standard evaluation |
Neurological Disorders Affecting Surgical Outcomes
Some neurological disorders can make laminectomy surgery more challenging. Conditions like Parkinson’s disease, multiple sclerosis, and peripheral neuropathy can complicate the surgery and recovery. A team approach is often needed to manage these patients well.
- Parkinson’s disease: Increased risk of post-operative falls and neurological deterioration
- Multiple sclerosis: Exacerbation of symptoms post-surgery is possible
- Peripheral neuropathy: Higher risk of nerve damage during surgery
In summary, neurological conditions are key in deciding if laminectomy is right for a patient. A detailed check of the patient’s neurological health is vital to reduce risks and aim for the best results.
Cardiovascular Conditions Limiting Surgical Eligibility
Laminectomy surgery needs a careful look at a patient’s health, focusing on their heart. Heart conditions can raise surgery risks. It’s key to check these before surgery.
Recent Cardiac Events
Those who’ve had heart attacks recently face higher surgery risks. Recent heart issues can make surgery outcomes worse. We often wait after such events to lower risks.
Uncontrolled Hypertension
High blood pressure is a big worry for laminectomy patients. High blood pressure can cause heart problems during surgery. It’s vital to control blood pressure with meds and lifestyle changes before surgery.
Anticoagulation Therapy Considerations
Patients on blood thinners need extra care before surgery. Blood thinners can make bleeding risks higher. We adjust meds and watch patients closely to lessen these risks.
Checking and managing heart conditions is key for laminectomy prep. By carefully looking at and fixing these issues, we can make surgery safer and better for patients.
Symptom Severity Assessment
When doctors check if a patient needs a laminectomy, they look at how bad the symptoms are. The type and how severe the symptoms are can decide if surgery is needed.
Purely Back Pain Without Neurological Symptoms
People with only back pain and no other symptoms might not need a laminectomy. Back pain alone is often treated without surgery. Surgery is usually considered when there are signs of nerve problems.
We check if there are other symptoms like numbness or weakness in the legs. These could mean nerve pressure. Without these symptoms, doctors look for other treatments first.
Minimal Symptoms Not Justifying Surgical Risk
For those with only a few symptoms, the risks of laminectomy might be too high. Surgical risks include infections, nerve damage, and spine instability.
- Doctors often choose not to operate for mild symptoms.
- They watch how symptoms change to see if surgery is needed.
- They try other ways to manage pain to keep the patient’s quality of life good.
Pain Management Alternatives
For those with few symptoms or not good candidates for laminectomy, there are other ways to manage pain. These include:
- Physical therapy to help move better and get stronger.
- Medicines like NSAIDs or muscle relaxants to ease pain.
- Epidural steroid injections to cut down inflammation and pain.
We help patients create a treatment plan that fits their needs and wants. Our goal is to find the best solution with the least harm.
“The key to successful treatment is not just alleviating symptoms but improving the patient’s overall quality of life.”
— Expert Spine Surgeon
Comorbidities Increasing Surgical Risk
When thinking about laminectomy, it’s key to check for comorbidities that might raise surgery risks. Comorbidities are other health issues that happen along with the main problem, like needing a laminectomy.
Diabetes and Wound Healing Concerns
Diabetes is a big comorbidity that can change how surgery goes. People with diabetes face more wound healing problems because of nerve damage and poor blood flow. Poor blood sugar control can cause more infections and slower healing. We tell diabetic patients to get their blood sugar in check before surgery.
Respiratory Conditions Affecting Anesthesia Risk
Conditions like COPD or asthma can make anesthesia harder and up the risk of breathing problems during and after surgery. Those with serious breathing issues might need extra checks and prep before surgery to lower risks.
Immunocompromised States
People with weakened immune systems, due to meds, disease, or other reasons, are more likely to get infections after surgery. We look closely at these patients’ immune health and might change their treatment to reduce risks.
Age-Related Considerations
Age is also a big factor in surgery risks. Older folks might have more health issues and less ability to bounce back, making them more prone to problems. While age isn’t a direct no-go, we carefully check older patients to see if they’re good candidates for surgery.
The table below shows the main comorbidities and how they might affect laminectomy:
| Comorbidity | Potential Impact | Pre-Surgical Considerations |
| Diabetes | Increased risk of wound healing complications and infection | Optimize blood sugar levels |
| Respiratory Conditions | Increased risk of respiratory complications during and after surgery | Evaluate and optimize respiratory function |
| Immunocompromised States | Higher risk of post-surgical infections | Assess immune status and adjust treatment plan |
| Advanced Age | Increased risk of complications due to reduced physiological reserve | Thorough pre-surgical evaluation |
Anatomical Complications: Scar Tissue and Infections
Before a laminectomy, it’s key to check for anatomical issues. These can affect how well the surgery goes.
Epidural Scar Tissue from Previous Surgeries
Epidural scar tissue is a common problem after spinal surgeries. It sticks to the dura mater or nerve roots, making surgery harder.
- Increased risk of nerve damage: Scar tissue can raise the chance of nerve damage during surgery.
- Complicated surgical approach: Surgeons might have to use a more complex method to deal with the scar tissue before the laminectomy.
Research shows that epidural scar tissue can make revision spine surgery riskier. A detailed check before surgery is vital to plan for these issues.
Active Spinal Infections
Active spinal infections are a big risk for those thinking about a laminectomy. Infections can weaken the spine and lead to more problems after surgery.
- Infection control: Infections must be controlled before surgery can happen.
- Antibiotic treatment: Patients might need antibiotics to clear the infection before the laminectomy.
A leading medical expert says, “Active spinal infections mean you can’t have elective spine surgery, like laminectomy.”
“Trying surgery when there’s an active infection can cause serious problems, like the infection spreading and the surgery site not healing right.”
Bone Quality Concerns
Bone quality is also very important for a laminectomy’s success. Bad bone quality, often from osteoporosis or other bone diseases, can make surgery harder.
- Increased risk of fractures: People with poor bone quality are more likely to break bones during or after surgery.
- Implant stability: The stability of any implants used in surgery might be worse in patients with poor bone quality.
We stress the need to check bone quality before surgery. This helps plan for any complications that might come up.
Spinal Tumors and Complex Pathologies
Spinal tumors are a big challenge in spinal surgery. They often need more than just a simple laminectomy. These cases need a detailed plan and a team effort.
When Tumors Require Alternative Approaches
Spinal tumors, whether they start in the spine or spread from elsewhere, can make surgery tricky. They might need a bigger surgery, like removing the tumor or easing pressure on the spinal cord.
Other ways to tackle these tumors include:
- En bloc resection for primary spinal tumors
- Palliative surgery for metastatic disease
- Minimally invasive techniques for specific tumor types
Metastatic Disease Considerations
Metastatic spinal disease needs a different strategy than primary tumors. The surgery’s goal might change to just help with pain, keep nerves working, and improve life quality.
Important things to think about for metastatic disease are:
| Factor | Consideration |
| Tumor type | Different cancers react differently to treatments |
| Spinal stability | Using the Spinal Instability Neoplastic Score (SINS) helps |
| Neurological status | How bad the nerve damage is matters a lot |
Multidisciplinary Approach Requirements
Handling spinal tumors and complex cases needs a team. This team includes neurosurgeons, orthopedic surgeons, and experts in cancer treatment.
This team works together to:
- Make a detailed treatment plan
- Coordinate care among different fields
- Work together to get the best results
Body Habitus Considerations
A patient’s overall health and body shape, or body habitus, are key in deciding if they’re right for laminectomy. We look at many factors, like obesity, to figure out the risks and possible problems.
Obesity and Surgical Complications
Being overweight can make surgery risks higher during and after laminectomy. Extra weight can make the spine work harder, making spinal problems worse. It also raises the chance of infections, breathing issues, and longer recovery times.
Research shows obese patients face more risks after laminectomy, like blood clots and lung problems. So, we check patients’ BMI to understand the risks better.
BMI Thresholds for Increased Risk
BMI, or body mass index, shows how weight relates to height. For laminectomy, a high BMI means more risk of problems after surgery. A BMI of 35 or more is seen as a big risk.
We use BMI categories to judge risk:
- A BMI under 30 is seen as low risk.
- A BMI between 30 and 35 is moderate risk.
- A BMI over 35 is high risk.
Pre-surgical Weight Management
For those with a high BMI, we suggest losing weight before surgery. A good weight loss plan can lower the risk of surgery problems.
Weight loss before surgery not only improves surgery results but also boosts health. We help patients create a weight loss plan. This might include eating better, exercising, and other steps.
By looking at body habitus and helping with weight loss before surgery, we can lower risks and better outcomes for laminectomy patients.
Diagnostic Uncertainty and Inadequate Imaging
Getting a correct diagnosis is key for successful surgery, like laminectomy. When images are not clear, it makes choosing the right surgery hard for doctors and patients.
When Imaging Findings Don’t Match Symptoms
It’s tough to diagnose spinal problems when images and symptoms don’t match. Advanced imaging techniques like MRI and CT scans show the spine’s details. But, doctors must link these images with what patients feel and what they see.
If images don’t match symptoms, more tests are needed. This could be more scans, neurological assessments, or other tests to find the real problem.
Required Diagnostic Workup Before Surgery
Before doing a laminectomy, a detailed check-up is needed. This includes:
- A full medical history and physical check
- Advanced imaging like MRI and CT scans
- Neurological tests to check nerve health
- More tests if needed to find other causes
Doing a complete check-up helps doctors decide if laminectomy is right for the patient.
Second Opinion Recommendations
If there’s doubt or unclear images, getting a second opinion is wise. A specialist can give new insights, confirm the diagnosis, or suggest other treatments.
Patients should get a second opinion if they’re unsure about their diagnosis or treatment. It ensures they get the best care for their condition.
Failed Back Surgery Syndrome Considerations
Failed back surgery syndrome (FBSS) is a big challenge in spinal care. It requires looking at the risks and benefits of revision surgery. When patients keep feeling pain after surgery, it makes choosing the next steps hard.
Risk of Worsening Outcomes with Repeat Surgery
One big worry with FBSS is the risk of repeat surgery. This surgery can be tricky and might not always help. The risk of getting worse or new problems is a big thing to think about for both patients and doctors.
Several things make repeat surgery riskier, including:
- Scar tissue from before
- Changes in the spine from earlier surgeries
- The patient’s health and any other health issues
Assessment Criteria for Revision Surgery
Deciding if someone should have revision surgery is a detailed process. Important things to look at are why the first surgery didn’t work, the patient’s symptoms now, and their health. MRI scans are key in this, showing the spine’s shape and any changes.
Choosing to do revision surgery is after a deep look, including:
- Looking at the patient’s medical history and doing a physical check
- Going over past surgery records and scans
- Thinking about other ways to manage pain
Alternative Pain Management Approaches
For many with FBSS, trying other ways to manage pain might be better than surgery. These can range from medicine and physical therapy to spinal cord stimulation.
These options are often chosen because they might help without the risks of more surgery. A team of doctors, physical therapists, and others work together to find the best plan.
Conclusion: Making Informed Decisions About Laminectomy
We’ve looked into the reasons you might not need laminectomy surgery. Knowing these reasons is key to making smart choices. Things like spinal instability and severe deformities can affect how well surgery works.
Doctors are very important in this process. They look at how bad your symptoms are and any other health issues you might have. They also check your body’s structure. This helps decide if surgery is right for you or if there are better options.
In some cases, not doing surgery might be the best choice. This is when your body is too unstable for surgery.
By thinking about the pros and cons together, you and your doctor can make a good choice. This teamwork helps make sure you get the best treatment for your needs. It aims to improve your health and life quality.
FAQ
What is a laminectomy, and what conditions does it treat?
A laminectomy is a surgery that removes part of the vertebrae. This is done to relieve pressure on the spinal cord or nerves. It helps with conditions like spinal stenosis, spondylolisthesis, and spinal deformities.
What are the absolute contraindications for a laminectomy?
Conditions that make laminectomy risky include spinal instability and severe spinal deformities. Active spinal infections and certain neurological conditions also fall under this category.
How does spinal instability affect eligibility for laminectomy?
Spinal instability can make laminectomy risky. It may lead to further instability or deformity after surgery. Instead, other treatments or stabilization procedures might be considered.
Can spondylolisthesis be a contraindication for laminectomy?
Yes, severe spondylolisthesis can be a contraindication. It may require additional surgical stabilization. The grade of spondylolisthesis is key in deciding if laminectomy is suitable.
How do severe spinal deformities like scoliosis and kyphosis impact laminectomy eligibility?
Severe curvatures can make laminectomy complicated. They may require alternative treatment strategies, such as corrective surgery or other non-surgical interventions.
Is laminectomy always necessary for mild spinal stenosis?
No, mild stenosis may not need surgery. Doctors often recommend conservative treatments first. They monitor the condition for any progression.
How do previous spinal implants affect the decision to perform a laminectomy?
Previous implants can complicate laminectomy. A careful assessment is needed. Imaging studies are essential to evaluate the existing hardware.
Can recent brain trauma or stroke history affect laminectomy eligibility?
Yes, recent brain trauma or a history of stroke can increase surgical risks. This makes laminectomy potentially unsuitable or requires careful risk assessment.
How do cardiovascular conditions influence laminectomy eligibility?
Conditions like recent cardiac events, uncontrolled hypertension, and anticoagulation therapy can affect eligibility. They increase surgical risks.
Are there symptom-related criteria that determine suitability for laminectomy?
Yes, the severity and nature of symptoms are considered. Minimal symptoms may not justify the surgical risks.
How do comorbidities like diabetes and respiratory issues impact laminectomy risks?
Comorbidities can complicate surgery. They affect wound healing, anesthesia risks, and overall recovery. A careful preoperative assessment is necessary.
Can anatomical complications like epidural scar tissue or active infections affect laminectomy?
Yes, these conditions can make surgery more challenging. They may require alternative approaches or preoperative treatment.
How are spinal tumors managed in the context of laminectomy?
Spinal tumors often require a multidisciplinary approach. Laminectomy may be part of the treatment plan, depending on the tumor’s nature and location.
Does obesity affect the risks associated with laminectomy?
Yes, obesity can increase surgical complications. Pre-surgical weight management may be recommended to mitigate these risks.
Why is accurate diagnosis and adequate imaging critical before laminectomy?
Accurate diagnosis ensures that symptoms are matched to the right surgery. This reduces the risk of unnecessary or ineffective surgery.
What are the considerations for patients with failed back surgery syndrome?
Repeat surgery carries risks of worsening outcomes. Alternative pain management strategies are often considered. A careful assessment for any revision surgery is necessary.
References
National Center for Biotechnology Information. Evidence-Based Medical Insight. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6859289/