Nearly 500,000 spinal fusion surgeries happen every year in the United States. Many patients wonder about their recovery journey. Understanding the recovery process is key to managing expectations and getting the best results.
and pain reduction strategies are important. The journey to recovery can be complex. But knowing what to expect can make it easier.
Key Takeaways
- Spinal fusion recovery is a gradual process that requires patience.
- Post-surgery mobility is key for a successful recovery.
- There are effective pain management strategies to reduce discomfort.
- Knowing the recovery timeline helps set realistic expectations.
- Following post-operative instructions is vital to avoid complications.
Understanding Spinal Fusion Surgery
Spinal fusion surgery is a key option for those with spinal problems. It joins vertebrae together to improve spine stability and reduce pain. This surgery is a way to find long-term relief from back issues.
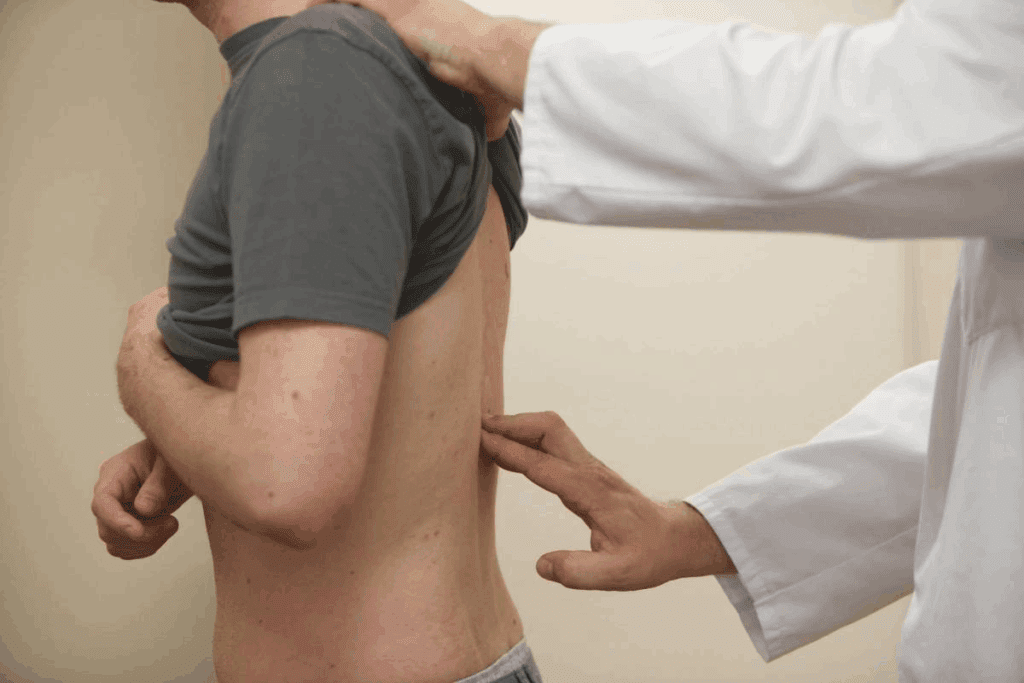
What Happens During the Procedure
The surgery starts with an incision in the back to reach the spine. Sometimes, it’s done from the front or side, depending on the case. The surgeon then uses bone grafts and metal rods to join the vertebrae.
Common Reasons for Undergoing Spinal Fusion
People get spinal fusion for many reasons. These include degenerative disc disease, scoliosis, spinal fractures, or spondylolisthesis. The main goal is to ease pain, fix deformities, and boost spinal function.
Knowing why you need spinal fusion helps prepare for the spinal fusion recovery journey.
| Condition | Description | Benefits of Spinal Fusion |
| Degenerative Disc Disease | A condition where the spinal discs lose their cushioning ability. | Reduces pain and stabilizes the spine. |
| Scoliosis | A deformity causing the spine to curve abnormally. | Corrects the curvature and improves posture. |
| Spinal Fractures | Breaks in one or more vertebrae. | Stabilizes the spine and promotes healing. |
Types of Spinal Fusion Techniques
Spinal fusion surgery uses different techniques. These include posterior lumbar interbody fusion (PLIF), anterior lumbar interbody fusion (ALIF), and transforaminal lumbar interbody fusion (TLIF). Each method is suited for different conditions and the surgeon’s preference.
Knowing about these techniques helps patients talk better with their doctors. They can choose the best option for their needs.
The Initial Recovery Phase: First 6 Weeks

Knowing what to expect in the first six weeks after surgery can make recovery easier. This time is key for managing pain, healing, and getting back to moving around.
Hospital Stay and Immediate Post-Op Experience
After spinal fusion surgery, patients usually stay in the hospital for a few days to a week. This depends on the surgery’s complexity and the patient’s health. Medical staff watch over the patient, manage pain, and teach about post-operative care.
Managing Pain and Medication Protocols
Reducing pain is a top priority in the early recovery phase. Patients get a mix of medicines to control pain, reduce swelling, and prevent infection. It’s important to take these medicines as told by doctors to manage pain well.
| Medication Type | Purpose | Common Side Effects |
| Pain Relievers | Manage post-surgery pain | Drowsiness, nausea |
| Anti-inflammatory | Reduce swelling and inflammation | Stomach upset, allergic reactions |
| Antibiotics | Prevent infection | Diarrhea, yeast infections |
Essential Movement Restrictions and Precautions
To help healing and avoid problems, patients must follow certain rules. They should not lift heavy things, bend, or twist too much. They also need to slowly get their nerves to heal.
- Avoid heavy lifting (>10 lbs)
- Minimize bending or twisting
- Gradually increase mobility
By sticking to these rules and talking often with doctors, patients can get through the early recovery phase better. This helps them do well in the long run.
Physical Sensations to Expect
After spinal fusion, patients may feel different sensations. These can range from pain to unusual nerve feelings. Knowing what to expect is key for a smooth recovery.
Distinguishing Between Normal and Abnormal Pain
Managing pain is a big concern after spinal fusion. It’s important to tell normal pain from abnormal pain. Normal pain is usually a dull ache or sharp pains when moving. Abnormal pain, on the other hand, could mean something’s wrong and may not go away.
Doctors say to watch out for pain that gets worse or comes with other symptoms like fever or numbness. If you notice this, tell your doctor right away.
“It’s important to keep an eye on your pain and tell your doctor if it changes a lot.”
Nerve Healing Sensations and Timeframes
Nerve healing sensations can vary a lot. Some people might feel tingling, numbness, or electric shock-like sensations. These feelings are usually because the nerves are healing or adjusting to the spine changes.
How long these sensations last can differ a lot. Usually, nerve healing takes months, with some feelings going away in 6 to 12 months. But remember, recovery can take even longer.
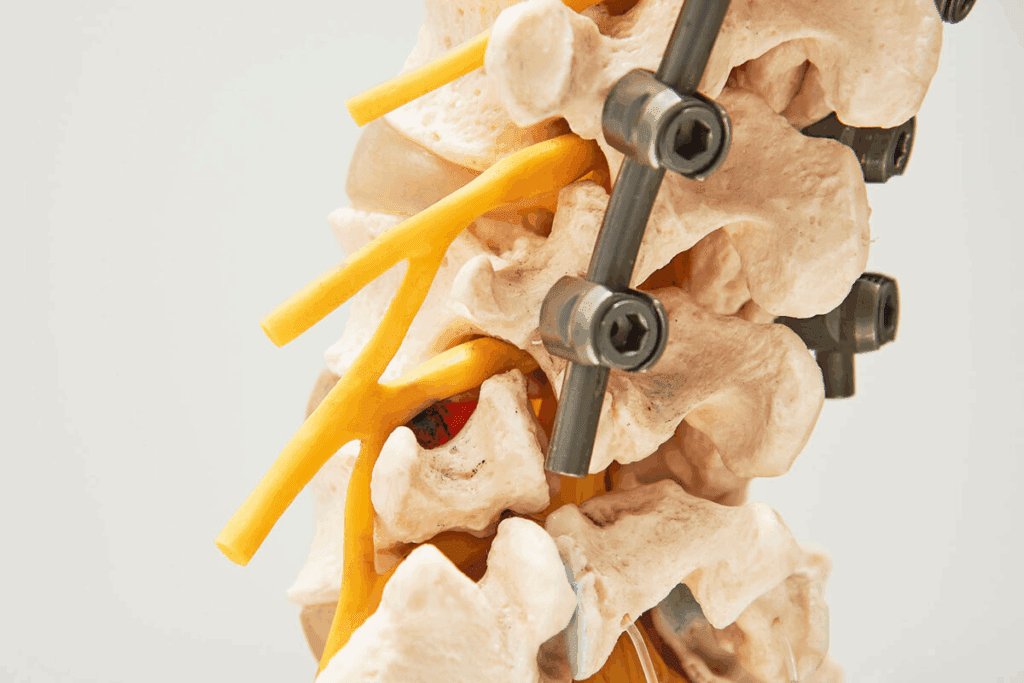
Hardware Awareness and Adaptation
Patients with spinal fusion and hardware (like rods or screws) might feel the hardware at first. This feeling can be unsettling, but it’s usually normal during recovery.
As the body heals and gets used to the hardware, the feeling of it tends to fade. Doing physical therapy as recommended can help you get used to the hardware and improve your spine’s function.
Will I Feel Normal After Spinal Fusion?
After spinal fusion, many wonder if they’ll feel normal again. Recovery is different for everyone. Knowing what to expect helps manage hopes and satisfaction.
Spinal fusion joins vertebrae to ease pain and stabilize the spine. Feeling normal again means healing bones, adjusting muscles, and adapting physically and mentally.
3-6 Month Recovery Milestones
In the first 3-6 months, patients see some improvement and discomfort. Pain levels usually decrease significantly as the fusion solidifies. Patients are encouraged to start walking and low-impact exercises to heal and strengthen the back.
Some numbness, tingling, or shooting pains are common as nerves heal. These signs are usually a good sign of nerve recovery. By the end of this period, many feel more like themselves, with some limitations.
6-12 Month Progress Expectations
Between 6-12 months, most see big progress. The fusion is fully healed, and patients often report a substantial reduction in pain. Mobility and strength improve, allowing for more activities and hobbies.
Some may have occasional pain, mainly after heavy lifting or bending. But these episodes are less common and less severe. By this time, many feel close to their new normal.
Long-Term Recovery Outlook (1-2 Years)
The long-term outlook for spinal fusion patients is generally positive, as most individuals notice a significant enhancement in their quality of life within 1-2 years post-surgery. They report less pain and better function.
While some may have occasional discomfort, most lead active, fulfilling lives. It’s key to keep up with exercises and lifestyle changes to keep the spine healthy and prevent future problems.
Regaining Mobility and Function
Getting back to normal after spinal fusion surgery is key. It involves physical therapy and making lifestyle changes. Patients need to know what to expect in terms of movement, how to build strength, and adjust to new ways of moving.
Realistic Expectations for Range of Motion
Patients often wonder about their future mobility after spinal fusion. The amount of movement regained depends on the surgery and the person’s flexibility before surgery. Most patients can move quite well again, but some stiffness is normal.
“It’s like learning to walk again; your body adapts, but it takes time,” said one patient.
Strategies for Rebuilding Strength and Endurance
Building strength and endurance is vital in recovery. A good physical therapy plan is essential. It should focus on exercises that strengthen the core and improve overall fitness.
- Start with low-impact activities like walking or swimming.
- Slowly add strength training exercises.
- Do flexibility and stretching exercises to keep movement.
Adapting to New Movement Patterns
Learning new ways to move is a big part of recovery. Patients must find ways to move that don’t stress their spine. This includes new techniques for bending, lifting, and even simple actions like getting out of bed.
“Learning to move differently was challenging, but it became second nature over time.”
By understanding the need to adapt and incorporating strategies for strength and endurance, patients can better navigate their recovery. This helps them regain their mobility and function.
Returning to Daily Activities
After spinal fusion surgery, it’s key to know how to safely get back to daily life. You’ll start with small steps, adding tasks back in slowly. This helps avoid putting too much stress on your spine.
Safe Approaches to Household Tasks and Self-Care
When you start doing household chores and taking care of yourself, be careful. Begin with easy tasks like light meal preparation or short periods of gentle stretching. As you get stronger, you can do more, but never lift, bend, or twist too much.
- Start with tasks that require minimal physical exertion.
- Use ergonomic tools and equipment to reduce strain.
- Take regular breaks to rest and avoid fatigue.
Guidelines for Resuming Driving and Transportation
Driving is a big part of daily life. Make sure you’re strong and mobile enough to drive safely. This usually takes 4-6 weeks, but it depends on your healing and your doctor’s advice.
When you start driving, adjust your seat and steering wheel for comfort. Begin with short trips and gradually make them longer as you get more comfortable.
Gradually Reintroducing Social Activities and Recreation
Social activities and fun things to do are important for your mind and heart. Start with easy, low-impact activities like short walks or small social events. Stay away from activities that could hurt your recovery, like heavy lifting or high-impact sports.
When you start doing social and fun activities again, listen to your body. If you feel pain or discomfort, slow down or change what you’re doing.
Getting back to daily life after spinal fusion surgery takes time, patience, and careful planning. By following these steps, you can safely and successfully return to your usual routine.
The Journey Back to Work
Going back to work after spinal fusion needs the right timing and accommodations. It’s also important to manage physical demands. This helps you get back to normal and recover well.
Determining the Right Timing for Work Return
The time it takes to go back to work varies. It depends on your job, the surgery type, and how you’re healing. Always listen to your doctor’s advice, as they know best.
Factors influencing return to work timing include:
- The physical demands of your job
- The extent of your surgery
- Your overall health and recovery pace
Asa renowned orthopedic surgeon, notes, “Going back to work too soon can harm your surgery’s success. Waiting too long can hurt your job and mental health.”
Necessary Workplace Accommodations and Ergonomics
Workplace changes and ergonomics are key for a smooth return. Employers must make adjustments to help employees after surgery.
Possible accommodations include:
- Modifying workstations to promote better posture and reduce strain
- Adjusting work schedules to avoid long hours or heavy lifting
- Providing ergonomic equipment to minimize discomfort
“Ergonomic adjustments can significantly reduce the risk of complications and improve the overall work experience for individuals post-spinal fusion,” says
.
Managing Work-Related Physical Demands
It’s important to manage your job’s physical demands after spinal fusion. This might mean changing tasks, taking breaks, and avoiding heavy lifting or bending.
| Job Type | Possible Modifications |
| Desk Job | Regular breaks, ergonomic chair |
| Manual Labor | Task reassignment, lifting aids |
Understanding the right timing for your return, alongside necessary accommodations and job demand management, is essential for a successful transition back to work following spinal fusion.
Effective Pain Management Strategies
Pain management is key to a smooth recovery after spinal fusion surgery. It involves using different methods to control pain effectively.
Medication Options and Considerations
Medicines are a big part of managing pain after spinal fusion. The right medicine and dose depend on your pain and health history. Here are some common ones:
- Opioids: For really bad pain, opioids might be given for a short time.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs can cut down inflammation and pain.
- Muscle Relaxants: These help with muscle spasms.
It’s important to take your medicine as told and talk to your doctor about any issues or side effects.
Non-Pharmaceutical Pain Relief Techniques
There are also non-medical ways to manage pain:
- Physical Therapy: Gentle exercises can make you move better and feel less pain.
- Heat and Cold Therapy: Heat or cold packs can ease pain and discomfort.
- Relaxation Techniques: Deep breathing, meditation, or yoga can help you relax and feel less stressed.
Using these methods with medicine can help you feel better.
“Pain is what happens when our brain perceives a threat to our body. Managing pain effectively requires a complete approach that tackles both the physical and emotional sides of pain.”
Addressing Breakthrough Pain Episodes
Breakthrough pain is sudden, intense pain that happens even with ongoing pain management. To handle it:
- Identify Triggers: Knowing what causes breakthrough pain helps manage it.
- Adjust Medication: Your doctor might change your medicine to better handle breakthrough pain.
- Use Rescue Medication: Sometimes, a special medicine is given for quick relief.
Working closely with your doctor is key to managing breakthrough pain.
Physical Therapy and Rehabilitation
Physical therapy is key after spinal fusion surgery. It helps patients get stronger, move better, and fully recover. A good physical therapy plan is made just for you and gets better as you get better.
Core Stabilization and Strengthening Protocols
Core stabilization is very important after spinal fusion. It makes the muscles around the spine stronger. This helps keep the spine stable and prevents more injuries. Exercises like planks, bridges, and pelvic tilts are part of this program.
- Planks: Strengthens the abdominal muscles and improves posture.
- Bridges: Targets the gluteal muscles and helps stabilize the lower back.
- Pelvic Tilts: Helps in mobilizing the lower back and strengthening the abdominal muscles.
Progressive Therapeutic Exercise Programs
Progressive exercises get harder as you get better. They help improve how well you can move, get stronger, and more flexible. A physical therapist will make a plan just for you.
The plan might include:
- Stretching exercises to improve flexibility.
- Strengthening exercises to build muscle around the spine.
- Aerobic exercises to enhance cardiovascular health.
Maximizing Your Physical Therapy Benefits
To get the most from physical therapy, follow your therapist’s advice. Go to all your sessions and do your exercises at home. Tell your therapist if you have any worries or if your symptoms change.
Being active in physical therapy can lead to a better recovery. You’ll get your function back and feel confident doing your daily activities again.
Long-Term Physical Considerations
After spinal fusion surgery, it’s important to know about long-term physical changes. These changes can affect your body in many ways. Knowing about them can help you recover better.
Permanent Changes in Spinal Biomechanics
Spinal fusion surgery makes permanent changes to the spine’s biomechanics. The fused part becomes stiff, changing how your spine moves. This can lead to:
- Altered stress distribution across adjacent spinal segments
- Potential for increased wear and tear on surrounding joints
- Changes in posture and gait due to the modified spinal structure
Adjacent Segment Degeneration: Risks and Prevention
One big worry after spinal fusion is adjacent segment degeneration (ASD). ASD is when the segments next to the fused area wear out. It can happen because of:
- Increased stress on adjacent segments due to the fusion
- Pre-existing degenerative conditions
- Age and overall spinal health
To lower the risk of ASD, try spine-friendly exercises. Keep a healthy lifestyle with good posture, regular exercise, and a balanced diet.
Managing Hardware-Related Sensations Long-Term
Patients with spinal fusion hardware might feel hardware-related sensations over time. These can be discomfort, clicking, or grating. To manage these feelings, you can:
- Monitor and report any discomfort to your healthcare provider
- Do physical therapy to improve spinal stability and reduce discomfort
- Keep a healthy weight to lessen stress on the spine and hardware
Understanding and dealing with these long-term physical changes can greatly improve your spinal fusion surgery’s success. It can also improve your overall quality of life.
Exercise and Physical Activity After Fusion
Knowing the right exercises after spinal fusion is vital for a good recovery. Exercise helps regain strength, improve flexibility, and keep the spine healthy.
Safe Exercise Options and Modifications
After spinal fusion, it’s important to pick gentle exercises for your spine. Some good choices include:
- Low-impact aerobics, like walking or swimming, which boost heart health without harming the spine.
- Stretching exercises that are modified for the fused area, keeping flexibility.
- Core strengthening exercises that support the spine without overloading it.
Activities to Approach with Caution or Avoid
While some activities are safe, others can risk the fused spine. It’s important to be careful or avoid:
- High-impact activities like running or jumping, which can stress the spine too much.
- Contact sports or activities with a risk of collision, which could harm the fused area.
- Bending or twisting exercises that could strain the spine or disrupt the fusion process.
Building a Sustainable Spine-Friendly Fitness Routine
Creating a lasting fitness routine after spinal fusion means:
- Starting slow and gradually adding more intensity and time to exercises.
- Mixing in cardio, strength training, and flexibility exercises.
- Listening to your body and changing your routine as needed.
By choosing spine-friendly exercises and avoiding risky activities, patients can lead a healthier, more active life after spinal fusion.
Lifestyle Modifications for Long-Term Success
Making changes to your daily routine can help your recovery after spinal fusion. These lifestyle changes can greatly improve your long-term results. They help you get the best from your surgery.
Ergonomic Adjustments for Home and Work
Ergonomics is key to reducing spine strain after surgery. Simple changes at work can make a big difference. For example, having your monitor at eye level and using an ergonomic chair can help.
Keeping things you use often within reach also helps. This way, you don’t have to stretch or bend as much.
| Ergonomic Adjustment | Benefit |
| Monitor at eye level | Reduces neck strain |
| Ergonomic chair | Supports proper posture |
| Frequently used items within reach | Minimizes stretching and bending |
Sleep Positioning and Mattress Considerations
How you sleep is important for keeping your spine aligned. Sleeping on your back with a pillow under your knees is good. Or, sleeping on your side with a pillow between your knees works too.
Also, a supportive mattress is key. It should keep its shape and support your body well.
- Use a supportive pillow to maintain neck alignment.
- Avoid sleeping on your stomach as it can cause your spine to arch.
- Consider a mattress with adjustable firmness.
Travel and Recreational Activity Adaptations
When traveling, take breaks to stretch and move. This is important, even on long trips. A supportive pillow or lumbar roll can help keep your spine aligned.
For fun activities, choose low-impact ones like swimming or cycling. These are easier on your spine.
Precautions for Traveling Post-Surgery:
- Plan regular breaks for stretching.
- Use supportive accessories like lumbar rolls.
- Avoid heavy lifting or bending.
By making these lifestyle changes, you can improve your life after spinal fusion surgery. It’s about making smart choices for your spinal health and well-being.
Mental and Emotional Adjustment
Life after spinal fusion surgery is not just about getting better physically. It’s also about adjusting mentally and emotionally. Healing is a whole-body, mind, and spirit process. Understanding the emotional side of recovery is as key as taking care of your body.
Processing Your New Physical Reality
After surgery, you might feel many emotions. These can include relief, frustration, anxiety, or even depression. It’s important to accept these feelings as part of healing.
Adjusting to your new body means coming to terms with changes. You might face new limits, learn to manage pain, or get used to hardware in your spine.
Key strategies for processing your new physical reality include:
- Keeping a journal to track your progress and emotions
- Engaging in open communication with your healthcare provider about your feelings and concerns
- Gradually resuming activities to regain confidence and independence
Strategies for Dealing with Frustration and Setbacks
Frustration and setbacks are common during recovery. Handling these challenges well is key to a positive recovery.
Setting realistic goals and celebrating small wins can keep you motivated. Also, connecting with support groups or loved ones can offer emotional support and advice.
“The greatest glory in living lies not in never falling, but in rising every time we fall.” – Nelson Mandela
This quote shows the importance of resilience in recovery. It’s about perseverance and finding strength to keep moving forward.
Finding Support Groups and Professional Resources
Support groups, whether in-person or online, are very helpful. They offer a community of people going through similar things. You can share advice, encouragement, and understanding.
Professional resources, like therapists or counselors, are also key. They can help manage anxiety, depression, or other emotional challenges during recovery.
Some benefits of seeking professional help include:
- Access to coping strategies tailored to your specific needs
- A safe space to discuss your feelings and concerns
- Support in navigating the emotional aspects of your recovery
By recognizing the importance of mental and emotional adjustment, you can take steps towards a holistic recovery. This means healing your spine and taking care of your overall well-being.
When to Be Concerned: Red Flags
It’s important to know the warning signs of complications after spinal fusion surgery. This knowledge helps in getting timely medical help. Most patients recover well, but knowing the red flags can prevent serious problems.
Signs of Complications Requiring Medical Attention
Some symptoms after spinal fusion surgery need immediate medical help. These include:
- Severe pain that doesn’t get better with medicine
- Swelling or redness around the surgery area
- Drainage or pus from the wound
- Fever over 101.5°F (38.6°C)
- Numbness, tingling, or weakness in the legs
Hardware Issues and Failure Symptoms
Hardware problems can show up in different ways. If you notice:
| Symptom | Description |
| Pain or discomfort | Increasing pain or discomfort at the surgical site |
| Hardware prominence | Visible or palpable hardware under the skin |
| Instability | Feeling of instability or giving way in the spine |
| Neurological symptoms | Numbness, tingling, or weakness related to hardware malfunction |
Infection Warning Signs and Prevention
Infection is a serious issue that can happen after spinal fusion. Look out for:
- Redness and swelling around the surgical site
- Increased pain or tenderness
- Pus or discharge from the wound
- Fever or chills
- General feeling of illness
To avoid infection, follow your surgeon’s wound care advice. Also, make sure to go to all follow-up appointments.
Conclusion: Embracing Your New Normal
Understanding your recovery expectations is key as you go through spinal fusion recovery. The journey is long and tough, but knowing what to expect helps you prepare.
Your life can get better as you heal and learn to live with your new spine. Making lifestyle changes, like using ergonomic tools and doing spine-friendly exercises, is important.
Knowing about long-term physical issues and acting early can help avoid problems. It’s about finding a balance and making choices that help your spine.
Keep working on getting stronger, adapting to new ways of moving, and adding healthy habits to your day. With time, patience, and support, you can live a better life and enjoy your new normal.
FAQ
What is spinal fusion surgery and why is it performed?
Spinal fusion surgery joins two or more vertebrae together. This helps stabilize the spine, reduce pain, and aid in healing. It’s used to treat issues like degenerative disc disease, scoliosis, or spinal fractures.
How long does it take to recover from spinal fusion surgery?
Recovery from spinal fusion surgery can take months to a year or more. It depends on how well the spine heals and how quickly you regain strength and mobility.
What are the common physical sensations after spinal fusion surgery?
After surgery, you might feel pain, numbness, tingling, or notice the hardware. These feelings are normal but it’s key to know the difference to heal properly.
Will I ever feel normal after spinal fusion surgery?
Spinal fusion surgery can greatly improve your life. But, you might not feel completely normal again. With the right rehabilitation and lifestyle changes, many people can feel very comfortable and functional.
How can I manage pain after spinal fusion surgery?
Managing pain involves using medicines, trying non-medical methods like physical therapy, and dealing with sudden pain episodes.
Can I return to my normal activities after spinal fusion surgery?
Yes, but you should start slowly and follow safe guidelines. This helps avoid problems and supports healing when doing household tasks, driving, or socializing.
How can I maintain a healthy spine after spinal fusion surgery?
Keeping your spine healthy means making lifestyle changes. This includes ergonomic adjustments, proper sleep, and travel tips. Regular exercise and physical activity are also important.
What are the long-term physical considerations after spinal fusion surgery?
Long-term concerns include changes in how your spine works, degeneration in other parts of your spine, and managing any sensations from the hardware.
Can I exercise after spinal fusion surgery?
Yes, but choose safe exercises and avoid harmful activities. Building a spine-friendly fitness routine helps with healing and keeps your spine healthy.
How can I cope with the emotional aspects of spinal fusion recovery?
Dealing with the emotional side of recovery means accepting your new body, handling frustration, and finding support. Look for groups and professional help.
What are the signs of complications after spinal fusion surgery?
Watch for signs of infection, problems with the hardware, and any failure symptoms. These need quick medical attention.
How can I adjust to my new normal after spinal fusion surgery?
Adapting to your new life means accepting lifestyle changes and learning new ways to move. Finding joy in life despite physical limits is key.
References
New England Journal of Medicine. Evidence-Based Medical Insight. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMoa066234